Vulvar cancer pathophysiology: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
|||
| Line 36: | Line 36: | ||
| Squamous cell carcinoma of vulva|| | | Squamous cell carcinoma of vulva|| | ||
* Most lesions originate in the labia, primarily the [[labia majora]]. Other areas affected are the [[clitoris]], and [[fourchette]], and the local glands | * Most lesions originate in the labia, primarily the [[labia majora]]. Other areas affected are the [[clitoris]], and [[fourchette]], and the local glands | ||
* | * Unifocal | ||
| | | | ||
* Eosinophilia | * Eosinophilia | ||
Revision as of 20:11, 6 October 2015
|
Vulvar cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Vulvar cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Vulvar cancer pathophysiology |
|
Risk calculators and risk factors for Vulvar cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Monalisa Dmello, M.B,B.S., M.D. [2]
Overview
Development of vulvar cancer is the result of multiple genetic mutations.
Pathogenesis of vulvar cancer
- Human papillomaviruses subtypes 16 and 18 (High risk) play an essential role in the pathogenesis of vulvar cancer. Once HPV enters an epithelial cell, the virus begins to make the proteins it encodes.
- Two of the proteins made by high-risk HPVs (E6 and E7) interfere with cell functions that normally prevent excessive growth, helping the cell to grow in an uncontrolled manner and to avoid cell death. Many times these infected cells are recognized by the immune system and eliminated. Sometimes, however, these infected cells are not destroyed, and a persistent infection results. As the persistently infected cells continue to grow, they may develop mutations in cellular genes that promote even more abnormal cell growth.
- HPV- related vulvar carcinoma is most commonly seen in younger women. vulvar intraepithelial neoplasia (VIN), related to HPV infection, subsequently leads to invasive vulvar cancer.[1]
Gross Patholgy
Microscopic Pathology
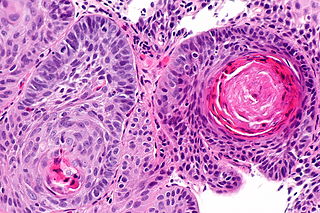
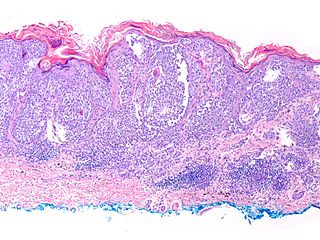
Histologic subtypes of vulvar Cancer include:[2][3][4][5]
- Vulvar carcinomas
- Squamous cell carcinoma
- Basal cell carcinoma
- Vulvar Paget disease
- Adenocarcinoma
- Transitional cell carcinoma
- Verrucous carcinoma
- Merkel cell tumors
- Verrucous carcinoma
- Vulvar malignant melanoma
- Vulvar sarcoma
- Leiomyosarcoma
- Malignant fibrous histiocytoma
- Epithelial sarcoma
| Vulvar carcinomas Subtype | Features on Gross Pathology | Features on Histopathological Microscopic Analysis |
| Squamous cell carcinoma of vulva |
|
 |
| Basal cell carcinoma of vulva |
|
 |
| Vulvar melanoma |
|
 |
References
- ↑ The Histopathology of Vulvar Neoplasia. Wilkinson, E, Glob. libr. women's med.http://www.glowm.com/section_view/heading/The%2520Histopathology%2520of%2520Vulvar%2520Neoplasia/item/256#13421 URL Accessed on September 30, 2015
- ↑ Hoffman, Barbara (2012). Williams gynecology. New York: McGraw-Hill Medical. ISBN 9780071716727.
- ↑ Malignant melanoma. Libre pathology. http://librepathology.org/wiki/index.php/Malignant_melanoma. URL Accessed on September 30, 2015
- ↑ Basal cell carcinoma . Libre pathology. http://librepathology.org/wiki/index.php/Basal_cell_carcinoma. URL Accessed on September 30, 2015
- ↑ Squamous cell carcinoma. Libre pathology. http://librepathology.org/wiki/index.php/Squamous_cell_carcinoma. URL Accessed on September 30, 2015