Venous thromboembolism: Difference between revisions
No edit summary |
No edit summary |
||
| Line 114: | Line 114: | ||
*With PE, depending upon the severity of the disease, the patient experience | *With PE, depending upon the severity of the disease, the patient experience | ||
**[[Dyspnea|shortness of breath]] | **[[Dyspnea|shortness of breath]] | ||
**[[Syncope]] | **[[Syncope|Loss of Consciousness]] | ||
**[[Chest pain|pleuritic chest pain]] | **[[Chest pain|pleuritic chest pain]] | ||
**[[Cough]] | **[[Cough]] | ||
**[[Hemoptysis]]. | **[[Hemoptysis|Blood in sputum]]. | ||
*While with DVT, patient can complain of | *While with DVT, patient can complain of | ||
**swelling of lower extremity which can be warm and tender. | **swelling of lower extremity which can be warm and tender. | ||
Revision as of 14:56, 25 October 2011
Editors-in-Chief: C. Michael Gibson, M.S., M.D. Associate Editor-In-Chief: Ujjwal Rastogi, MBBS [1]
|
Venous thromboembolism Microchapters |
Overview
Venous thromboembolism (VTE) is a hypernym which includes Deep venous thrombosis (DVT) and pulmonary embolism (PE). It is a major public health problem and one of the most common cause of preventable cause of death in hospital patients. It is the third most common cardiovascular disorder after coronary artery disease and stroke. It is frequently underestimated and misdiagnosed and failure to provide adequate prophylaxis and therapy can be fatal for the patient.
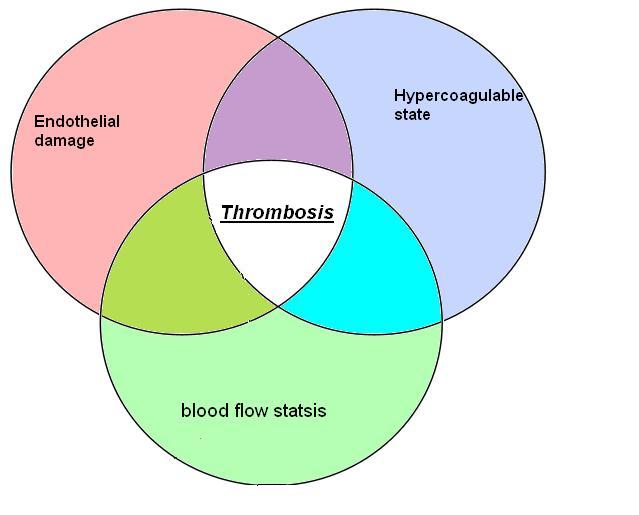
Pathophysiology
Figure : Virchow's triad encompasses three broad categories of factors that are thought to contribute to venous thrombosis.
Classification Scheme
VTE includes DVT and PE, which are further divided into:
- Deep Venous Thrombosis: Its classified as
- Superficial
- Upper extremity
- Isolated Calf
- Proximal
- Pulmonary embolism:its classified as
- Silent
- Symptomatic
- Fatal
Epidemiology
Annualy, more than 900,000 cases are reported to have clinicaly evident Venous thromboembolism. More than 300,000 deaths are attributed to pulmonary embolism in United states[1]. More than 25,000 people die in England from venous thromboembolism developed in hospital. This is more than the total number of deaths attributable to Breast cancer, AIDS, and road traffic accidents, when combined together. Close to a third of total patients encounter some sort of a long term effects.[2]
Risk Factors
Recently a research group[3]. has postulated a risk-prediction algorithm for VTE. This algorith helps:
- Estimates individual risk for VTE
- To start prophylaxis in patients at risk for VTE.
This algorithm does not work in these conditions:
- History of venous thrombosis
- Family history of venous thrombosis.
- Pregnant patients
- Patients on Anticoagulations
- Symptoms suggestive of thrombosis.
The various variables that are taken into account are as follows
| Age |
| Body mass index |
| Smoking status (non-smoker; ex-smoker; light, moderate, or heavy smoker) |
| Townsend deprivation score |
| Varicose veins |
| Congestive cardiac failure |
| Rheumatoid arthritis |
| Chronic renal disease |
| Inflammatory bowel disease |
| Cancer:(lung, gastrointestinal, pancreas, renal, breast, prostate, other) |
| Recent hospital admission |
| Recent hip fracture or hip surgery (or both) |
| Current use of antipsychotic drugs:(none, atypical, typical) |
| Current use of tamoxifen |
| Current use of hormone replacement therapy: (none, equine or non-equine hormone replacement therapy) |
| Use of antiplatelets |
| Cardiovascular disease(stroke, transient ischaemic attack, or coronary artery disease) |
| Atrial fibrillation |
| Asthma |
| Chronic obstructive pulmonary disease |
| Family history of venous thromboembolism |
To calculate the risk prediction click here
Differential Diagnosis
There are other conditions that can mimic VTE
- Venous
- Superficial thrombophlebitis
- Post-thrombotic syndrome
- Chronic venous insufficiency
- Venous obstruction
- Other
- Cellulitis
- Baker's cyst
- Torn gastrocnemius muscle
- Fracture
- Haematoma
- Acute arterial ischaemia
- Lymphoedema
- Hypoproteinaemia (for example, cirrhosis, nephrotic syndrome)
Diagnosis
History & Symptoms
As VTE involves both DVT and PE, the patient can present with complaints of either of the disease.
- With PE, depending upon the severity of the disease, the patient experience
- While with DVT, patient can complain of
- swelling of lower extremity which can be warm and tender.
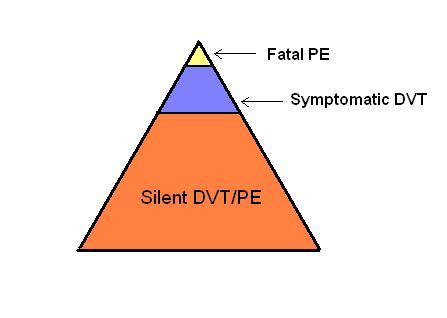
Only 10-20% of VTE is clinically recognized, as depicted by the figure below
Figure :The challenge in diagnosis of VTE
See also
- Venous thromboembolism: Under-recognized and under-treated
- Deep vein thrombosis
- Pulmonary embolism
- Thrombosis
- Nephrotic syndrome and risk of venous and arterial thromboembolism
References
- ↑ Heit JA (2008). "The epidemiology of venous thromboembolism in the community". Arterioscler Thromb Vasc Biol. 28 (3): 370–2. doi:10.1161/ATVBAHA.108.162545. PMC 2873781. PMID 18296591.
- ↑ Prandoni P, Lensing AW, Cogo A, Cuppini S, Villalta S, Carta M; et al. (1996). "The long-term clinical course of acute deep venous thrombosis". Ann Intern Med. 125 (1): 1–7. PMID 8644983.
- ↑ Hippisley-Cox J, Coupland C (2011). "Development and validation of risk prediction algorithm (QThrombosis) to estimate future risk of venous thromboembolism: prospective cohort study". BMJ. 343: d4656. doi:10.1136/bmj.d4656. PMC 3156826. PMID 21846713. line feed character in
|title=at position 12 (help)