Tuberous sclerosis
| Tuberous sclerosis | |
 | |
|---|---|
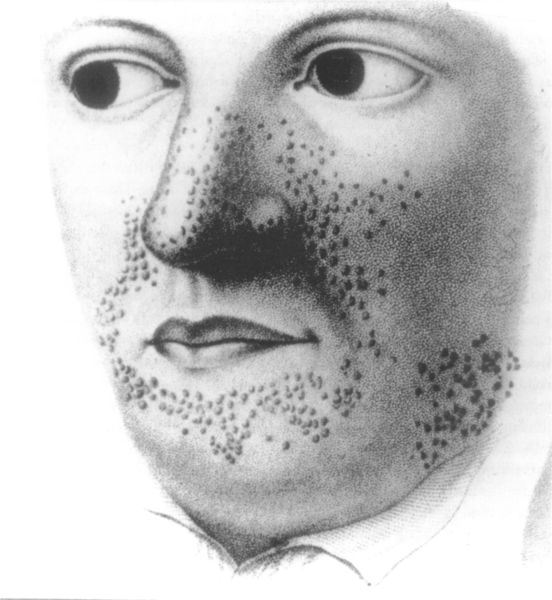
| Earliest illustration, from Rayer's atlas of skin diseases, 1835. |
|
Tuberous sclerosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tuberous sclerosis On the Web |
|
American Roentgen Ray Society Images of Tuberous sclerosis |
For patient information on this page, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]
Synonyms and keywords: Tuberous sclerosis complex, TSC, Bourneville disease, Bourneville-Pringle syndrome, epiloia
Physical Examination
Skin
-
Adenoma sebaceum.
-
Tuberous sclerosis; Subungual fibroma; Beneath the Left Index Nail
-
Tuberous sclerosis, Periungual Fibroma; Lateral Side of Left Great Toe Nail
The skin is examined under a Wood's lamp. The most common skin abnormalities include:
- Facial angiofibromas
- Ungual or subungual fibromas
- Hypomelanic macules ("ash leaf spots")
- Forehead plaques
- Shagreen patches
- Molluscum fibrosum or skin tags
- Cafe-au-lait spots or flat brown marks
- Poliosis
Head
- Pitted tooth enamel
- Rubbery growths on the tongue or gums
Eyes
- Retinal lesions - astrocytic hamartomas
- Non-retinal lesions associated with TSC include
- Coloboma
- Angiofibromas of the eyelids
- Papilledema (related to hydrocephalus)
Heart
- A heart murmur can be heard due to the obstruction of blood flow by rhabdomyomas.
Lungs
- Coarse rales are heard when lung parenchyma is involved.
- Bronchial breathing and bronchophony are heard on auscultation when multiple cysts occur in the lungs.
Extremities
- Rough growths under or around the fingernails and toenails
Neurologic
- Abnormal size of head in children - due to hydrocephalus
- Low IQ
- Learning difficulties
- Intellectual disability
- Troubled communication and social interaction
Lab tests
Molecular genetic testing is commercially available in the United States for the diagnosis of tuberous sclerosis. Genetic testing identifies mutations only in 75% - 80%. The 15%-20% failure rate is thought to be due to somatic mosaicism. Therefore a negative genetic test does not rule out the diagnosis of tuberous sclerosis.
Imaging
CT
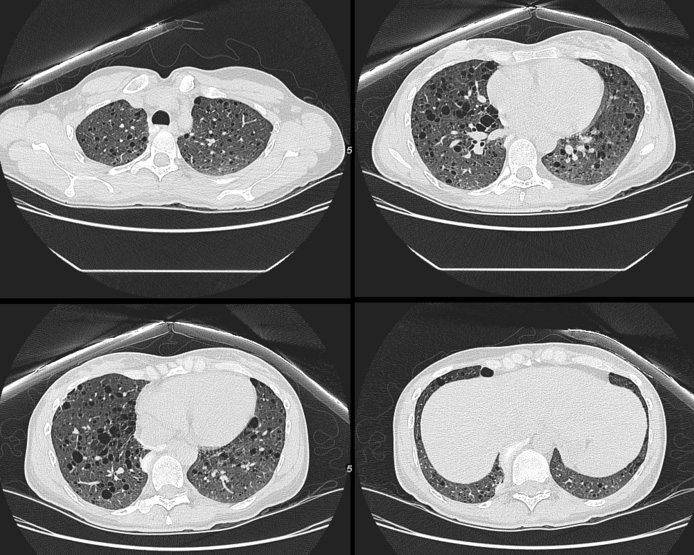 |
 |
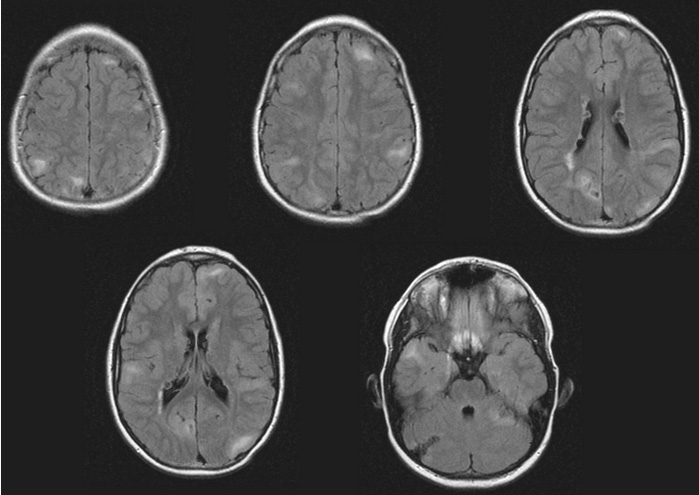
MRI
The tubers are typically triangular in configuration, with the apex pointed towards the ventricles, and are thought to represent foci of abnormal neuronal migration. The T2 signal abnormalities may subside in adulthood, but will still be visible on histopathological analysis. On magnetic resonance imaging, TSC patients can exhibit other signs consistent with abnormal neuron migration (radial white matter tracts hyperintense on T2WI, heterotopic gray matter).
Echocardiography
- A cardiac rhabdomyoma can be discovered using echocardiography in approximately 50% of people with TSC.
Ultrasoud
- Ultrasound abdomen is used to visualize kidney angiomyolipomas and cysts
- Prenatal ultrasound, performed by an obstetric sonographer specializing in cardiology, can detect a rhabdomyoma after 20 weeks. This rare tumour is a strong indicator of TSC in the child, especially if there is a family history of TSC.
Treatment
Medical therapy
Drug therapy for some of the manifestations of TSC is currently in the developmental stage.[1] For example, a 2008 study found that treatment with rapamycin rescued learning and memory deficits in a mouse model of tuberous sclerosis.[2] Community TSC is a distributed computing project to find drugs to treat TSC.[citation needed] The patients usually have relapse of symptoms in the clinical course. Unless any vital function is affected, life expectancy is good. Majority of patients will require some medications to control symptoms, e.g., anti-epileptics to control seizures. In 2010 everolimus was approved for the treatment of subependymal giant cell astrocytoma.
Other drugs used include:
Facial angiofibromas is a socially embarrassing rash that starts to appear during childhood and can be removed using dermabrasion or laser treatment.
Surgical therapy
Ungual or subungual fibromas may need to be surgically removed if they enlarge or cause bleeding.
References
- ↑ Yates JR (2006). "Tuberous sclerosis". Eur. J. Hum. Genet. 14 (10): 1065–73. doi:10.1038/sj.ejhg.5201625. PMID 16868562. Unknown parameter
|month=ignored (help) - ↑ Ehninger D, Han S, Shilyansky C; et al. (2008). "Reversal of learning deficits in a Tsc2+/− mouse model of tuberous sclerosis". Nat Med. 14 (8): 843–8. doi:10.1038/nm1788. PMC 2664098. PMID 18568033. Lay summary – Science News (23 June 2008).
- ↑ Tsao CY (2009). "Current trends in the treatment of infantile spasms". Neuropsychiatr Dis Treat. 5: 289–99. PMC 2695218. PMID 19557123.
- ↑ Simon D. Shorvon (2010). Handbook of Epilepsy Treatment. John Wiley and Sons. pp. 93–. ISBN 978-1-4051-9818-9. Retrieved 11 October 2010.
Support Groups
- United Kingdom: The Tuberous Sclerosis Association. Awareness month is October.
- United States: Tuberous Sclerosis Alliance. Awareness month is May.
- Canada: Tuberous Sclerosis Canada. Awareness month is May.
- Australasia: Australasian Tuberous Sclerosis Society.
- Brazil: Associação Brasileira de Esclerose Tuberosa (Brazilian Tuberous Sclerosis Association) Template:Pt icon
- Taiwan: Taiwan Tuberous Sclerosis Complex
Template:Phakomatoses and other congenital malformations not elsewhere classified


