|
|
| Line 10: |
Line 10: |
| {{SK}} TN; tic douloureux; tic doloreux; tic doloureux; prosopalgia; Fothergill neuralgia | | {{SK}} TN; tic douloureux; tic doloreux; tic doloureux; prosopalgia; Fothergill neuralgia |
|
| |
|
| ==Overview==
| |
| Trigeminal neuralgia is a [[Neuropathy|neuropathic]] disorder of the [[trigeminal nerve]] that causes episodes of intense pain in the eyes, lips, nose, scalp, forehead, and jaw.<ref>{{cite journal |author=Bayer DB, Stenger TG |title=Trigeminal neuralgia: an overview |journal=Oral Surg. Oral Med. Oral Pathol. |volume=48 |issue=5 |pages=393-9 |year=1979 |pmid=226915 |doi=}}</ref>
| |
|
| |
|
| ==Epidemiology and Demographics==
| |
| An estimated one in 15,000 people suffers from trigeminal neuralgia, although numbers may be significantly higher due to frequent misdiagnosis. It usually develops after the age of 40, although there have been cases with patients being as young as three years of age <ref>{{cite web | last = Bloom | first = R | title = Emily Garland: A young girl's painful problem took more than a year to diagnose | url = http://www.tna-support.org/newlook/sgl_files/library/newsletters/middletenn/2005%20November-December%20web%20pages.pdf | format = PDF}}</ref>.
| |
|
| |
|
| ==Natural History, Complications and Prognosis==
| |
| Trigeminal neuralgia is considered by many to be among the most painful of conditions and once was labeled the "'''suicide disease'''" because of the significant numbers of people taking their own lives before effective treatments were discovered.
| |
|
| |
|
| ==Pathophysiology==
| |
| The pain of trigeminal neuralgia is often falsely attributed to a pathology of dental origin. "Rarely do patients come to the surgeon without having had removed many, and not infrequently all, teeth on the affected side or both sides." <ref>{{cite book |last= Dandy|first=Sir Walter |authorlink=Walter Dandy |title=The Brain |edition=Special edition |series=The Classics of Neurology and Neurosurgery |year=1987 |month= |publisher=Gryphon editions |location=Birmingham |pages=179 }}</ref> Extractions do not help for the pain is originating in the trigeminal nerve and not in an individual nerve of a tooth. Because of this difficulty, many patients may go untreated for long periods of time before a correct diagnosis is made.
| |
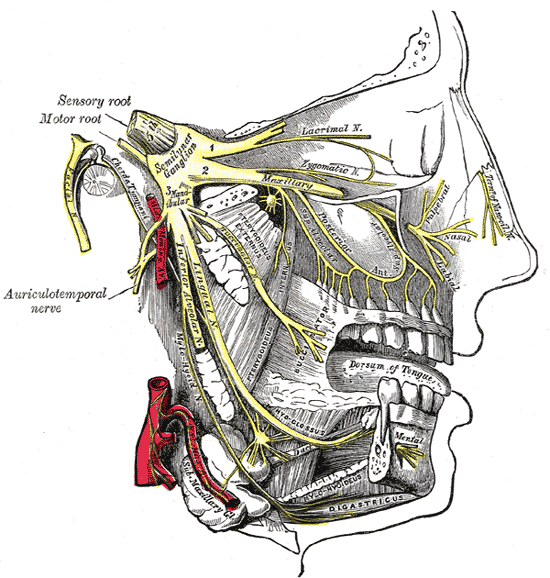
| The trigeminal nerve is the fifth [[cranial nerve]], a mixed cranial nerve responsible for sensory data such as [[tactition]] (pressure), [[thermoception]] (temperature), and [[Pain and nociception|nociception]] (pain) originating from the face above the jawline; it is also responsible for the motor function of the [[Mastication#Muscles of mastication|muscles of mastication]], the muscles involved in chewing but not facial expression. Several theories exist to explain the possible causes of this pain syndrome. The leading explanation is that a blood vessel is likely to be compressing the trigeminal nerve near its connection with the pons. The [[superior cerebellar artery]] is the most-cited culprit. Such a compression can injure the nerve's protective myelin sheath and cause erratic and hyperactive functioning of the nerve. This can lead to pain attacks at the slightest stimulation of any area served by the nerve as well as hinder the nerve's ability to shut off the pain signals after the stimulation ends. This type of injury also may be caused by an [[aneurysm]] (an outpouching of a [[blood vessel]]); by a [[tumor]]; by an [[arachnoid cyst]] in the [[cerebellopontine angle]]<ref>Babu R, Murali R. "Arachnoid cyst of the cerebellopontine angle manifesting as contralateral trigeminal neuralgia: case report", ''Neurosurgery'' 1991 Jun;28(6):886-7. (PMID 2067614)</ref>, or by a traumatic event such as a car accident or even a tongue piercing. [http://www.theglobeandmail.com/servlet/story/RTGAM.20061017.wtongues1017/BNStory/specialScienceandHealth/home] Two to four percent of patients with TN, usually younger, have evidence of [[multiple sclerosis]], which may damage either the trigeminal nerve or other related parts of the brain. When there is no structural cause, the syndrome is called [[idiopathic]]. [[Postherpetic Neuralgia]], which occurs after [[shingles]], may cause similar symptoms if the trigeminal nerve is affected.
| |
|
| |
|
| ==Causes==
| |
| === Complete Differential Diagnosis for Trigeminal Neuralgia ===
| |
| In alphabetical order. <ref>Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016</ref> <ref>Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X</ref>
| |
|
| |
|
| *[[Acoustic Neuroma]]
| |
| *Blood vessels compressing the [[trigeminal nerve]] root
| |
| *[[Brain Tumor]]
| |
| *Chronic meningeal infection
| |
| *[[Cluster headache]]
| |
| *[[Dental Infection]]
| |
| *[[Glossopharyngeal neuralgia]]
| |
| *[[Idiopathic]]
| |
| *Ischemic cerebrovascular disorders
| |
| *[[Multiple Sclerosis]]
| |
| *Physical damage to the nerve
| |
| *[[Postherpetic neuralgia]]
| |
| *[[Temporomadibular Joint Syndrome]]
| |
| *Vascular malformation
| |
|
| |
|
| ==Diagnosis==
| |
| ===Symptoms===
| |
| The episodes of pain occur paroxysmally, or suddenly. To describe the pain sensation, patients describe a trigger area on the face, so sensitive that touching or even air currents can trigger an episode of pain. It affects lifestyle as it can be triggered by common activities in a patient's daily life, such as toothbrushing. Breezes, whether cold or warm, wintry weather or even light touching such as a kiss can set off an attack. The attacks are said to feel like stabbing electric shocks or shooting pain that becomes intractable. Individual attacks affect one side of the face at a time, last several seconds or longer, and repeats up to hundreds of times throughout the day. The pain also tends to occur in cycles with complete remissions lasting months or even years. 3-5% of cases are bilateral, or occurring on both sides. This normally indicates problems with both trigeminal nerves since one serves strictly the left side of the face and the other serves the right side. Pain attacks typically worsen in frequency or severity over time. A great deal of patients develop the pain in one branch, then over years the pain will travel through the other nerve branches.
| |
|
| |
|
| Signs of this can be seen in males who may deliberately miss an area of their face when shaving, in order to avoid triggering an episode. Although trigeminal neuralgia is not fatal, successive recurrences may be incapacitating, and the fear of provoking an attack may make sufferers reluctant to engage in normal activities.
| |
|
| |
|
| There is a variant of trigeminal neuralgia called "atypical trigeminal neuralgia". In some cases of atypical trigeminal neuralgia, the sufferer experiences a severe, relentless underlying pain similar to a migraine in addition to the stabbing pains. This variant is sometimes called "trigeminal neuralgia, type 2"[http://www.ohsu.edu/facialpain/facial_pain-dx.shtml], based on a recent classification of facial pain<ref>Burchiel KJ. "A new classification for facial pain", ''Neurosurgery'' 2003 Nov;53(5):1164-6; discussion 1166-7. (PMID 14580284)</ref>. In other cases, the pain is stabbing and intense, but may feel like burning or prickling, rather than a shock. Sometimes, the pain is a combination of shock-like sensations, migraine-like pain, and burning or prickling pain. It can also feel as if a boring piercing pain is unrelenting.
| |
|
| |
|
| ==Treatment==
| |
| There is no cure for trigeminal neuralgia, but most people find relief from medication, from one of the five surgical options or sometimes from one of the many so-called "complementary or alternative" therapies. Atypical trigeminal neuralgia, which involves a more constant and burning pain, is more difficult to treat, both with medications and surgery. Surgery may result in varying degrees of numbness to the patient and lead occasionally to ''"anesthesia dolorosa,"'' which is numbness with intense pain. However, many people do find dramatic relief with minimal side effects from the various surgeries that are now available.<ref>{{cite journal | last = Weigel | first = G | coauthors = Casey, K. | title = Striking Back: The Trigeminal Neuralgia and Face Pain Handbook | journal = Trigeminal Neuralgia Association ISBN 0-9672393-2-X | year = 2004 }}</ref> During a TN attack, some patients may get quick relief by applying an ice pack or a readily available source of cold temperature to the area of pain.
| |
|
| |
|
| ===Medications===
| |
| * [[Anticonvulsant]]s such as [[carbamazepine]], [[oxcarbazepine]], [[topiramate]], [[phenytoin]], or [[gabapentin]] are generally the most effective medications. Pain relievers usually do not help. Anticonvulsant effects may be potentiated with an adjuvant such as [[baclofen]] or [[clonazepam]]. [[Baclofen]] may also help some patients eat more normally if jaw movement tends to aggravate the symptoms.
| |
|
| |
|
| * If anticonvulsants don't help and surgical options have failed or are ruled out, the pain may be treated long-term with an [[opioid]] such as [[methadone]].
| |
|
| |
|
| * Low doses of some [[antidepressant]]s can be effective in treating neuropathic pain.
| |
|
| |
|
| * [[Botox]] can be injected into the nerve by a physician, and has been found helpful using the "migraine" pattern adapted to the patient's special needs.
| |
|
| |
|
| Many patients cannot tolerate medications for years, and an alternate treatment is to take a drug such as [[gabapentin]] and place it in an externally applied cream base by a pharmacist who [[Compounding|compounds]] drugs. Also helpful is taking a "drug holiday" when remissions occur and rotating medications if one becomes ineffective.
| |
|
| |
|
| ===Surgery===
| |
| Surgery may be recommended, either to relieve the pressure on the nerve or to selectively damage it in such a way as to disrupt pain signals from getting through to the brain. In trained hands, surgical success rates have been reported at better than 90 percent.
| |
|
| |
|
| Of the five surgical options, the [[microvascular decompression]] is the only one aimed at fixing the presumed cause of the pain. In this procedure, the surgeon enters the skull through a 25mm (one-inch) hole behind the ear. The nerve is then explored for an offending blood vessel, and when one is found, the vessel and nerve are separated or "decompressed" with a small pad. When successful, MVD procedures can give permanent pain relief with little to no facial numbness.
| |
|
| |
|
| Three other procedures use needles or catheters that enter through the face into the opening where the nerve first splits into its three divisions. Excellent success rates using a cost effective [[percutaneous]] surgical procedure known as '''balloon compression''' have been reported<ref>{{cite journal | last = Natarajan | first = M | title = Percutaneous trigeminal ganglion balloon compression: experience in 40 patients | journal = Neurology (Neurological Society of India) | year = 2000 | volume = 48 | issue = 4 | pages = 330-2 | pmid = 11146595}}</ref>. This technique has been helpful in treating the elderly for whom surgery may not be an option due to coexisting health conditions. Balloon compression is also the best choice for patients who have [[ophthalmic]] nerve pain or have experienced recurrent pain after [[microvascular decompression]].
| |
|
| |
|
| Similar success rates have been reported with glycerol injections and radiofrequency rhizotomies. Glycerol injections involve injecting an alcohol-like substance into the cavern that bathes the nerve near its junction. This liquid is corrosive to the nerve fibers and can mildly injure the nerve enough to hinder the errant pain signals. In a radiofrequency rhizotomy, the surgeon uses an electrode to heat the selected division or divisions of the nerve. Done well, this procedure can target the exact regions of the errant pain triggers and disable them with minimal numbness.
| |
|
| |
|
| ===Stereotactic Radiation Therapy===
| | ==External Links== |
| The nerve can also be damaged to prevent pain signal transmission using [[Gamma Knife]] or a linear accelerator-based radiation therapy (e.g. Novalis, Cyberknife). No incisions are involved in this procedure. It uses radiation to bombard the nerve root, this time targeting the selective damage at the same point where vessel compressions are often found. This option is used especially for those people who are medically unfit for a long [[general anesthesia|general anaesthetic]], or who are taking medications for prevention of blood clotting (e.g., [[warfarin]]). A prospective Phase I trial performed at Marseille, France, showed that 83% of patients were pain-free at 12 months, with 58% pain-free and off all medications. Side effects were mild, with 6% experiencing mild tingling and 4% experiencing mild numbness.<ref name="pmid16776335">{{cite journal |author=Régis J, Metellus P, Hayashi M, Roussel P, Donnet A, Bille-Turc F |title=Prospective controlled trial of gamma knife surgery for essential trigeminal neuralgia |journal=J. Neurosurg. |volume=104 |issue=6 |pages=913–24 |year=2006 |pmid=16776335 |doi=}}</ref>
| |
| | |
| ==References==
| |
| {{reflist|2}}
| |
| | |
| ==External links== | |
| *[http://www.tna-support.org/ Trigeminal Neuralgia Association] | | *[http://www.tna-support.org/ Trigeminal Neuralgia Association] |
| *[http://www.mytn.co.uk/ A Personal Perspective on Trigeminal Neuralgia (TN) and the Micro Vascular Decompression (MVD) procedure]
| |
| *[http://www.kgeh.com/kgBrainSpine/aboutsurgery.html About surgery for trigeminal neuralgia]
| |
| *[http://www.umanitoba.ca/cranial_nerves/trigeminal_neuralgia/manuscript/index.html/ Your Complete Guide to Trigeminal Neuralgia]
| |
| * {{MedlinePlusOverview|trigeminalneuralgia}}
| |
|
| |
|
| {{PNS diseases of the nervous system}} | | {{PNS diseases of the nervous system}} |
| Line 97: |
Line 43: |
| {{WikiDoc Help Menu}} | | {{WikiDoc Help Menu}} |
| {{WikiDoc Sources}} | | {{WikiDoc Sources}} |
|
| |
| [[Category:Primary care]] | | [[Category:Primary care]] |
| [[Category:Neurosurgery]] | | [[Category:Neurosurgery]] |