Tricuspid atresia surgery: Difference between revisions
Jump to navigation
Jump to search
| Line 9: | Line 9: | ||
*** If the [[pulmonary artery]] comes from the [[left ventricle]] and is overflowed, [[pulmonary artery]] banding is useful for lowering the [[pulmonary blood flow]]. | *** If the [[pulmonary artery]] comes from the [[left ventricle]] and is overflowed, [[pulmonary artery]] banding is useful for lowering the [[pulmonary blood flow]]. | ||
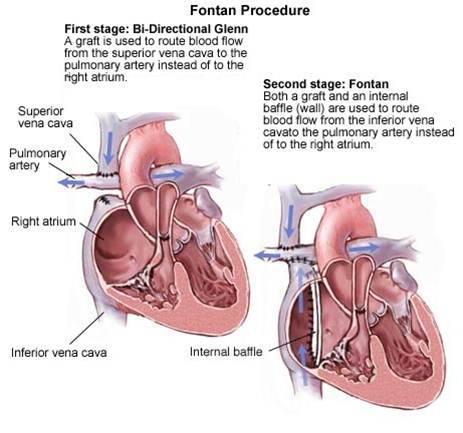
*** In older children, [[bi-direction Glenn shunt]] which is the connection between [[superior vena cava]] to the[[ pulmonary artery]] will be done for transferring the blood to the pulmonary system. | *** In older children, [[bi-direction Glenn shunt]] which is the connection between [[superior vena cava]] to the[[ pulmonary artery]] will be done for transferring the blood to the pulmonary system. | ||
***[[Fontan]] procedure is a conduit between the[[ inferior vena cava]] and the[[ pulmonary artery]] whether transfers the systemic venous blood to [[pulmonary circulation at the age of 2-3 years old. | ***[[Fontan]] procedure is a conduit between the [[ inferior vena cava]] and the[[ pulmonary artery]] whether transfers the systemic venous blood to [[pulmonary circulation at the age of 2-3 years old. | ||
***[[Endocarditis]] prophylaxis before every procedure is recommended. | ***[[Endocarditis]] prophylaxis before every procedure is recommended. | ||
Revision as of 16:49, 21 August 2020
|
Tricuspid atresia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenarios |
|
Case Studies |
|
Tricuspid atresia surgery On the Web |
|
American Roentgen Ray Society Images of Tricuspid atresia surgery |
|
Risk calculators and risk factors for Tricuspid atresia surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Keri Shafer, M.D. [2] Priyamvada Singh, MBBS [3]; Assistant Editor-In-Chief: Kristin Feeney, B.S. [4]
Surgery
- Surgery is the mainstay of therapy for tricuspid atresia.
- In the first 8 weeks of life if there are severe Cyanosis and pulmonary obstruction and normal positioning aorta and pulmonary artery, making a shunt between systemic subclavian artery to thepulmonary artery is necessary which is called Blalock -Taussig(BT shunt).
- If the pulmonary artery comes from the left ventricle and is overflowed, pulmonary artery banding is useful for lowering the pulmonary blood flow.
- In older children, bi-direction Glenn shunt which is the connection between superior vena cava to thepulmonary artery will be done for transferring the blood to the pulmonary system.
- Fontan procedure is a conduit between the inferior vena cava and thepulmonary artery whether transfers the systemic venous blood to [[pulmonary circulation at the age of 2-3 years old.
- Endocarditis prophylaxis before every procedure is recommended.
Surgical Interventions
There are a number of interventional methods to address a tricuspid atresia. These include:
- PGE1 to maintain patent ductus arteriosus
- Modified Blalock-Taussig shunt to maintain pulmonary blood flow by placing a Gortex conduit between the subclavian artery and the pulmonary artery.
- Cavopulmonary anastomosis (hemi-Fontan or bidirectional Glenn) to provide stable pulmonary flow
- Fontan procedure to redirect inferior vena cava and hepatic vein flow into the pulmonary circulation
ACC/AHA 2008 Guidelines for the Management of Adults With Congenital Heart Disease (DO NOT EDIT)[1][2]
Surgical Options for Patients With Single Ventricle (DO NOT EDIT)[1][2]
| Class I |
| "1. Surgeons with training and expertise in congenital heart disease (CHD) should perform operations for single-ventricle anatomy or physiology. (Level of Evidence: C)" |
Evaluation and Follow-Up After Fontan Procedure (DO NOT EDIT)[1][2]
| Class I |
| "1. Lifelong follow-up is recommended for patients after a Fontan type of operation; this should include a yearly evaluation by a cardiologist with expertise in the care of adult congenital heart disease (ACHD) patients. (Level of Evidence: C)" |
Surgery for Adults With Prior Fontan Repair (DO NOT EDIT)[1][2]
| Class I |
| "1. Surgeons with training and expertise in CHD should perform operations on patients with prior Fontan repair for single-ventricle physiology. (Level of Evidence: C)" |
| "2. Reoperation after Fontan is indicated for the following: (Level of Evidence: C)" |
| "a. Unintended residual atrial septal defect (ASD) that results in right-to-left shunt with symptoms and/or cyanosis not amenable to transcatheter closure. (Level of Evidence: C)" |
| "b. Hemodynamically significant residual systemic artery-to-pulmonary artery shunt, residual surgical shunt, or residual ventricle-to-pulmonary artery connection not amenable to transcatheter closure. (Level of Evidence: C)" |
| "c. Moderate to severe systemic atrioventricular (AV) valve regurgitation. (Level of Evidence: C)" |
| "d. Significant (greater than 30-mm Hg peak-to-peak) subaortic obstruction. (Level of Evidence: C)" |
| "e. Fontan pathway obstruction. (Level of Evidence: C)" |
| "f. Development of venous collateral channels or pulmonary arteriovenous malformation not amenable to transcatheter management. (Level of Evidence: C)" |
| "g. Pulmonary venous obstruction. (Level of Evidence: C)" |
| "h. Rhythm abnormalities, such as complete AV block or sick sinus syndrome, that require epicardial pacemaker insertion. (Level of Evidence: C)" |
| "i. Creation or closure of a fenestration not amenable to transcatheter intervention. (Level of Evidence: C)" |
| Class IIa |
| "1. Reoperation for Fontan conversion (i.e., revision of an atriopulmonary connection to an intracardiac lateral tunnel, intra-atrial conduit, or extracardiac conduit) can be useful for recurrent atrial fibrillation or flutter without hemodynamically significant anatomic abnormalities. A concomitant Maze procedure should also be performed. (Level of Evidence: C)" |
| Class IIb |
| "1. Heart transplantation may be beneficial for severe SV dysfunction or protein losing enteropathy (PLE). (Level of Evidence: C)" |
References
- ↑ 1.0 1.1 1.2 1.3 Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA; et al. (2008). "ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: Executive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines for the management of adults with congenital heart disease)". Circulation. 118 (23): 2395–451. doi:10.1161/CIRCULATIONAHA.108.190811. PMID 18997168.
- ↑ 2.0 2.1 2.2 2.3 Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA; et al. (2008). "ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease). Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". J Am Coll Cardiol. 52 (23): e1–121. doi:10.1016/j.jacc.2008.10.001. PMID 19038677.