Traveler's diarrhea medical therapy: Difference between revisions
YazanDaaboul (talk | contribs) No edit summary |
|||
| Line 6: | Line 6: | ||
==Medical Therapy== | ==Medical Therapy== | ||
===Rehydration | ===Rehydration=== | ||
*The mainstay of therapy for traveler's diarrhea is rehydration. | |||
:*Oral rehydration fluids are indicated among patients who can tolerate oral intake, otherwise IV rehydration is indicated. | |||
:*Over the counter oral rehydration solutions (ORS) are optimal options for oral rehydration and are usually available for both adults and children. | |||
:*Oral rehydration solutions may be home-made by mixing the following: | |||
::*Drinking water: 1 liter | |||
::*Salt: 0.5 teaspoon | |||
::*Sugar: 6 teaspoons | |||
:*Rehydration must be gradual until signs of dehydration (e.g. dry mouth, oliguria) are resolved. Drinking ORS must be slow (1 sip every 5 minutes). | |||
:*Children often require 1 liter of ORS, whereas adults often require 3 liters of ORS. | |||
:*Energy drinks with high concentrations of electrolytes (e.g. sports drinks) may be offered to adults, but not children. | |||
:*Fluids high in sugar content (e.g. soda) are not recommended because they may worsen the dehydration. | |||
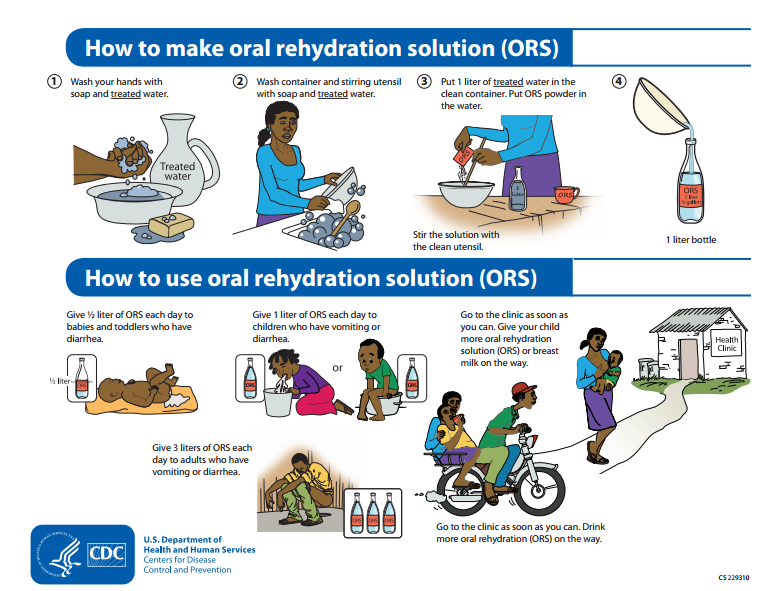
[[Image:CDC ORS.png|900px]] | |||
===Antimicrobial Therapy=== | |||
*Since the majority of cases of traveler's diarrhea are caused by bacterial pathogens, empiric antibiotic therapy is usually recommended among both adult and pediatric patients diagnosed with traveler's diarrhea. | |||
*Travelers who develop three or more loose stools in a 24-hour period — especially if associated with [[nausea]], [[vomiting]], [[abdominal]] [[cramps]], [[fever]], or [[blood in stool]]s — benefit from [[antimicrobial]] therapy. | |||
*Antibiotics usually are given for 3–5 days, but single dose [[azithromycin]] or [[levofloxacin]] have been used (for adults and children).<ref>{{cite journal|title=Azithromycin and loperamide are comparable to levofloxacin and loperamide for the treatment of traveler's diarrhea in United States military personnel in Turkey|author=Sanders JW, Frenck RW, Putnam SD, ''et al.''|journal=Clin Infect Dis|year=2007|volume=45|pages=294–301|url=http://www.journals.uchicago.edu/CID/journal/issues/v45n3/50169/brief/50169.abstract.html}}</ref> | |||
*If [[diarrhea]] persists despite therapy, travelers should be evaluated and treated for possible parasitic infection. | |||
:*There are different medications needed for bacterial [[dysentery]], for [[amoebic dysentery]], and for [[giardia]] | |||
:*There is no medication for ''[[Cryptosporidium]]'', which typically affects individuals with [[AIDS]]. | |||
:*'''Empiric Therapy'''<ref>{{Cite web | title = The Practice of Travel Medicine: Guidelines by the Infectious Diseases Society of America | url = http://www.idsociety.org/uploadedFiles/IDSA/Guidelines-Patient_Care/PDF_Library/Travel%20Medicine.pdf }} </ref> | |||
:* ''' | |||
::* '''Antibiotic treatment''' | ::* '''Antibiotic treatment''' | ||
:::* Preferred regimen (1): [[Norfloxacin]] 400 mg PO bid | :::* Preferred regimen (1): [[Norfloxacin]] 400 mg PO bid single dose or 1-day therapy | ||
:::* Preferred regimen (2): [[Ciprofloxacin]] 500 mg PO bid | :::* Preferred regimen (2): [[Ciprofloxacin]] 500 mg PO bid single dose or 1-day therapy | ||
:::* Preferred regimen (3): [[Ofloxacin]] 200 mg PO bid | :::* Preferred regimen (3): [[Ofloxacin]] 200 mg PO bid single dose or 1-day therapy | ||
:::* Preferred regimen (4): [[Levofloxacin]] 500 mg PO qd | :::* Preferred regimen (4): [[Levofloxacin]] 500 mg PO qd single dose or 1-day therapy | ||
:::* | :::* Alternative regimen (1): [[Azithromycin]] 1000 mg PO single dose {{or}} [[Azithromycin]] 500 mg PO for 1-3 days | ||
:::* Preferred regimen ( | |||
===Symptomatic Management=== | |||
* '''Symptomatic management'''<ref>{{Cite web | title = The Practice of Travel Medicine: Guidelines by the Infectious Diseases Society of America | url = http://www.idsociety.org/uploadedFiles/IDSA/Guidelines-Patient_Care/PDF_Library/Travel%20Medicine.pdf }} </ref> | |||
:*'''Abdominal discomfort''' | |||
::* Preferred regimen (1): [[Bismuth subsalicylate]] 1 oz PO every 30 min for 8 doses | |||
:*'''Vomiting''' | |||
::* Preferred regimen (2): [[Loperamide]] 4 mg PO {{then}} 2 mg after each loose stool not to exceed 16 mg daily | |||
::*Note (1): Antimotility agents are not generally recommended for patients with bloody diarrhea or those who have diarrhea and fever. | |||
::*Note (2): Loperamide can be used in children, and liquid formulations are available. In practice, however, these drugs are rarely given to small children (aged <6 years) | |||
===Antimotility Agents === | ===Antimotility Agents === | ||
Revision as of 16:25, 1 March 2016
|
Traveler's diarrhea Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Traveler's diarrhea medical therapy On the Web |
|
American Roentgen Ray Society Images of Traveler's diarrhea medical therapy |
|
Risk calculators and risk factors for Traveler's diarrhea medical therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
TD usually is a self-limited disorder and often resolves without specific treatment; however, oral rehydration therapy is often beneficial to replace lost fluids and electrolytes. Antibiotics are used in those who develop three or more loose stools in a 24-hour period — especially if associated with nausea, vomiting, abdominal cramps, fever or blood in stools
Medical Therapy
Rehydration
- The mainstay of therapy for traveler's diarrhea is rehydration.
- Oral rehydration fluids are indicated among patients who can tolerate oral intake, otherwise IV rehydration is indicated.
- Over the counter oral rehydration solutions (ORS) are optimal options for oral rehydration and are usually available for both adults and children.
- Oral rehydration solutions may be home-made by mixing the following:
- Drinking water: 1 liter
- Salt: 0.5 teaspoon
- Sugar: 6 teaspoons
- Rehydration must be gradual until signs of dehydration (e.g. dry mouth, oliguria) are resolved. Drinking ORS must be slow (1 sip every 5 minutes).
- Children often require 1 liter of ORS, whereas adults often require 3 liters of ORS.
- Energy drinks with high concentrations of electrolytes (e.g. sports drinks) may be offered to adults, but not children.
- Fluids high in sugar content (e.g. soda) are not recommended because they may worsen the dehydration.
Antimicrobial Therapy
- Since the majority of cases of traveler's diarrhea are caused by bacterial pathogens, empiric antibiotic therapy is usually recommended among both adult and pediatric patients diagnosed with traveler's diarrhea.
- Travelers who develop three or more loose stools in a 24-hour period — especially if associated with nausea, vomiting, abdominal cramps, fever, or blood in stools — benefit from antimicrobial therapy.
- Antibiotics usually are given for 3–5 days, but single dose azithromycin or levofloxacin have been used (for adults and children).[1]
- If diarrhea persists despite therapy, travelers should be evaluated and treated for possible parasitic infection.
- There are different medications needed for bacterial dysentery, for amoebic dysentery, and for giardia
- There is no medication for Cryptosporidium, which typically affects individuals with AIDS.
- Empiric Therapy[2]
- Antibiotic treatment
- Preferred regimen (1): Norfloxacin 400 mg PO bid single dose or 1-day therapy
- Preferred regimen (2): Ciprofloxacin 500 mg PO bid single dose or 1-day therapy
- Preferred regimen (3): Ofloxacin 200 mg PO bid single dose or 1-day therapy
- Preferred regimen (4): Levofloxacin 500 mg PO qd single dose or 1-day therapy
- Alternative regimen (1): Azithromycin 1000 mg PO single dose OR Azithromycin 500 mg PO for 1-3 days
Symptomatic Management
- Symptomatic management[3]
- Abdominal discomfort
- Preferred regimen (1): Bismuth subsalicylate 1 oz PO every 30 min for 8 doses
- Vomiting
- Preferred regimen (2): Loperamide 4 mg PO THEN 2 mg after each loose stool not to exceed 16 mg daily
- Note (1): Antimotility agents are not generally recommended for patients with bloody diarrhea or those who have diarrhea and fever.
- Note (2): Loperamide can be used in children, and liquid formulations are available. In practice, however, these drugs are rarely given to small children (aged <6 years)
Antimotility Agents
Antimotility agents (loperamide, diphenoxylate, and paregoric) primarily reduce diarrhea by slowing transit time in the gut, and, thus, allows more time for absorption. Some persons believe diarrhea is the body's defense mechanism to minimize contact time between gut pathogens and intestinal mucosa. In several studies, antimotility agents have been useful in treating travelers' diarrhea by decreasing the duration of diarrhea. However, these agents should never be used by persons with fever or bloody diarrhea, because they can increase the severity of disease by delaying clearance of causative organisms. Because antimotility agents are now available over the counter, their injudicious use is of concern. Adverse complications (toxic megacolon, sepsis, and disseminated intravascular coagulation) have been reported as a result of using these medications to treat diarrhea.
References
- ↑ Sanders JW, Frenck RW, Putnam SD; et al. (2007). "Azithromycin and loperamide are comparable to levofloxacin and loperamide for the treatment of traveler's diarrhea in United States military personnel in Turkey". Clin Infect Dis. 45: 294&ndash, 301.
- ↑ "The Practice of Travel Medicine: Guidelines by the Infectious Diseases Society of America" (PDF).
- ↑ "The Practice of Travel Medicine: Guidelines by the Infectious Diseases Society of America" (PDF).