Thymoma differential diagnosis
|
Thymoma Microchapters |
|
Diagnosis |
|---|
|
Case Studies |
|
Thymoma differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Thymoma differential diagnosis |
|
Risk calculators and risk factors for Thymoma differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Amr Marawan, M.D. [2]
Differential Diagnosis
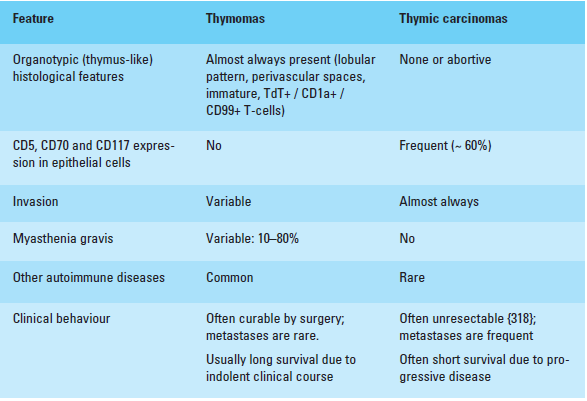
Differential diagnosis of thymomas types A, AB, B and thymic carcinomas.[1]
 |
Anterior Mediastinal Masses
It's very difficult to differentiate radiologically.
- Thymic masses
- Thymoma Benign tumor that arise from the thymus and is associated with more than 15% of patients with myasthenia gravis.
- Thymic Cyst: It is incidental mass that may be congenital or acquired. It might contain parathyroid or salivary tissue, as they has a common embryological origin.
- Thymic Hyperplasia: Resected only if associated paraneoplastic syndrome.
- Thymolipoma: Increased thymic size with mixed adipose tissue.
- Thymic carcinoma: Rare thymic tumor, poor survival rate, high rate of recurrence. Sometimes called type C thymoma.
- Thymic Carcinoid: Also called thymic neuroendocrine tumors, uncommon and present as mass in the anterior mediastinum.
- Ectopic parathyroid tissue.
- Germ cell tumors
Most common site for extragonadal germ cell tumors is the mediastinum.
- [[Teratomas]s: Represents two thirds of mediastinal GCTs. Usually benign, but when malignant it's very aggressive and very poor prognosis.
- Dermoid cysts: Very rare tumor, only 118 cases have been reported.[2]
- -Malignant GCTs: 90% of malignant mediastinal GCTs occur in males. Full physical examination and scrotal U/S is required.
- Seminomas: Slightly more common, grow slowly but might reach large sizes.
- Non-seminomatous GCTs: Consists of yolk sac tumor, embryonal cell carcinoma, and/or choriocarcinoma. Commonly between 20-40 years of age.
Tumor markers are very helpful in diagnosing GCTs. AFP is normal in teratoma and “pure” seminomas. Beta-HCG is mildly elevated in 10 percent of patients with seminomas. Ninety percent of non-seminomatous GCTs have elevated AFP and/or beta-HCG.
- Lymphoma (terrible, could be middle or posterior mediastinal too)
Nodular sclerosing Hodgkin’s lymphoma and primary mediastinal B-cell lymphoma are the two common types that present in the mediastinum. Usually has systemic symptoms as fever weight loss and night sweats and may also have other symptoms as chest pain, wheezing, dyspnea or superior vena cava syndrome.
- Thyroid (intrathyroid goitre)
Presents with shortness of breath or dysphagia.