Testicular cancer natural history, complications and prognosis: Difference between revisions
No edit summary |
No edit summary |
||
| (20 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{CMG}}; {{AE}} {{Rim}} {{SC}} | |||
{{CMG}}; {{AE}} {{G.D.}},{{Rim}} {{SC}} | |||
{{Testicular cancer}} | {{Testicular cancer}} | ||
==Overview== | ==Overview== | ||
[[Prognosis]] of testicular cancer is generally good, and the 5-year survival rate is approximately 96.6% (2004-2010).Common complications of testicular cancer include [[metastasis]], [[bleeding]], [[infection]], and [[infertility]]. | [[Prognosis]] of testicular cancer is generally good, and the 5-year [[Survival rates|survival rate]] is approximately 96.6% (2004-2010). Common [[complications]] of testicular cancer include [[metastasis]], [[bleeding]], [[infection]], and [[infertility]]. | ||
==Natural History== | |||
===Germ cell testicular tumor=== | |||
====Seminoma==== | |||
*[[Seminoma]] tends to occur in middle aged people. | |||
*Rarely [[metastasize|metastasize.]]<ref name="pmid26612222">{{cite journal |vauthors=Howitt BE, Berney DM |title=Tumors of the Testis: Morphologic Features and Molecular Alterations |journal=Surg Pathol Clin |volume=8 |issue=4 |pages=687–716 |date=December 2015 |pmid=26612222 |doi=10.1016/j.path.2015.07.007 |url=}}</ref> | |||
*Affects people in their 15 and 35 years old | |||
====Embryonal Carcinoma==== | |||
*[[Median]] [[age]] is 30 years old<ref name="pmid26612222">{{cite journal |vauthors=Howitt BE, Berney DM |title=Tumors of the Testis: Morphologic Features and Molecular Alterations |journal=Surg Pathol Clin |volume=8 |issue=4 |pages=687–716 |date=December 2015 |pmid=26612222 |doi=10.1016/j.path.2015.07.007 |url=}}</ref> | |||
*Has most of the component of mixed non seminoma germ tumor<ref name="pmid26612222">{{cite journal |vauthors=Howitt BE, Berney DM |title=Tumors of the Testis: Morphologic Features and Molecular Alterations |journal=Surg Pathol Clin |volume=8 |issue=4 |pages=687–716 |date=December 2015 |pmid=26612222 |doi=10.1016/j.path.2015.07.007 |url=}}</ref> | |||
*Tend to [[metastasize]] early to [[lungs]], [[retroperitoneum]], and [[liver]]<ref name="pmid19066212">{{cite journal |vauthors=Ishida M, Hasegawa M, Kanao K, Oyama M, Nakajima Y |title=Non-palpable testicular embryonal carcinoma diagnosed by ultrasound: a case report |journal=Jpn. J. Clin. Oncol. |volume=39 |issue=2 |pages=124–6 |date=February 2009 |pmid=19066212 |doi=10.1093/jjco/hyn141 |url=}}</ref> | |||
====Choriocarcinoma==== | |||
*Patient presents with early symptoms if there are [[metastatic]] lesions.<ref name="pmid26504875">{{cite journal |vauthors=Lowe K, Paterson J, Armstrong S, Walsh S, Groome M, Mowat C |title=Metastatic Testicular Choriocarcinoma: A Rare Cause of Upper GI Bleeding |journal=ACG Case Rep J |volume=3 |issue=1 |pages=36–8 |date=October 2015 |pmid=26504875 |pmc=4612755 |doi=10.14309/crj.2015.94 |url=}}</ref> | |||
*Early [[metastasis]] through hematogenous route | |||
*Tends to [[metastasize]] to [[lungs]], brain, [[liver]], [[peritoneum]], and others. | |||
*Affects most male patients in the second and third decade of their life.<ref name="pmid20057969">{{cite journal |vauthors=Lee SC, Kim KH, Kim SH, Lee NS, Park HS, Won JH |title=Mixed testicular germ cell tumor presenting as metastatic pure choriocarcinoma involving multiple lung metastases that was effectively treated with high-dose chemotherapy |journal=Cancer Res Treat |volume=41 |issue=4 |pages=229–32 |date=December 2009 |pmid=20057969 |pmc=2802842 |doi=10.4143/crt.2009.41.4.229 |url=}}</ref> | |||
====Yolk Sac tumor==== | |||
*Mostly seen in [[children]] less than 2 years old<ref name="pmid8127257">{{cite journal |vauthors=Coppes MJ, Rackley R, Kay R |title=Primary testicular and paratesticular tumors of childhood |journal=Med. Pediatr. Oncol. |volume=22 |issue=5 |pages=329–40 |date=1994 |pmid=8127257 |doi= |url=}}</ref> | |||
*Patients are usually [[asymptomatic]] at onset<ref name="pmid25547829">{{cite journal |vauthors=Wei Y, Wu S, Lin T, He D, Li X, Liu J, Liu X, Hua Y, Lu P, Wei G |title=Testicular yolk sac tumors in children: a review of 61 patients over 19 years |journal=World J Surg Oncol |volume=12 |issue= |pages=400 |date=December 2014 |pmid=25547829 |pmc=4326497 |doi=10.1186/1477-7819-12-400 |url=}}</ref> | |||
*Tends to have elevated alpha fetoproteins ([[AFP]]) | |||
====Spermatocytic tumor==== | |||
*Seen in old men | |||
*Barely [[metastasize]]<ref name="pmid9227931">{{cite journal |vauthors=Bosl GJ, Motzer RJ |title=Testicular germ-cell cancer |journal=N. Engl. J. Med. |volume=337 |issue=4 |pages=242–53 |date=July 1997 |pmid=9227931 |doi=10.1056/NEJM199707243370406 |url=}}</ref> | |||
===Sex cord stromal testicular tumor=== | |||
====Leydig cell tumor==== | |||
*Seen mostly in any age | |||
*[[Benign]] in boys aged 5 to 10 years old and [[malignant]] in adults aged 30 to 60 years old<ref name="pmid17284120">{{cite journal |vauthors=Al-Agha OM, Axiotis CA |title=An in-depth look at Leydig cell tumor of the testis |journal=Arch. Pathol. Lab. Med. |volume=131 |issue=2 |pages=311–7 |date=February 2007 |pmid=17284120 |doi=10.1043/1543-2165(2007)131[311:AILALC]2.0.CO;2 |url=}}</ref><ref name="pmid2024387">{{cite journal |vauthors=Dilworth JP, Farrow GM, Oesterling JE |title=Non-germ cell tumors of testis |journal=Urology |volume=37 |issue=5 |pages=399–417 |date=May 1991 |pmid=2024387 |doi= |url=}}</ref> | |||
*It [[Metastasize|metastasizes]] in the regional [[Lymph node|lymph nodes]] such as [[iliac]], [[inguinal]] and retroperitonial nodes<ref name="pmid3756826">{{cite journal| author=Grem JL, Robins HI, Wilson KS, Gilchrist K, Trump DL| title=Metastatic Leydig cell tumor of the testis. Report of three cases and review of the literature. | journal=Cancer | year= 1986 | volume= 58 | issue= 9 | pages= 2116-9 | pmid=3756826 | doi=10.1002/1097-0142(19861101)58:9<2116::aid-cncr2820580925>3.0.co;2-x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3756826 }}</ref> | |||
====Sertoli cell tumor==== | |||
* It affects both infants and older adults | |||
* [[Malignancy]] is seen in infants in presence of [[metastasis]]<ref name="pmid2024387">{{cite journal |vauthors=Dilworth JP, Farrow GM, Oesterling JE |title=Non-germ cell tumors of testis |journal=Urology |volume=37 |issue=5 |pages=399–417 |date=May 1991 |pmid=2024387 |doi= |url=}}</ref> | |||
* [[Sertoli cell]] tumor is associated with [[Peutz-Jeghers syndrome]] and Carney complex. | |||
* large cell calcifying [[Sertoli cells|sertoli cell]] [[tumor]] is associated with Carney's complex (syndrome of [[myxoma]], spotty [[pigmentation]] and [[endocrine]] overactivity).<ref name="pmid11832717">{{cite journal |vauthors=Washecka R, Dresner MI, Honda SA |title=Testicular tumors in Carney's complex |journal=J. Urol. |volume=167 |issue=3 |pages=1299–302 |date=March 2002 |pmid=11832717 |doi= |url=}}</ref><ref name="pmid7446466">{{cite journal |vauthors=Proppe KH, Scully RE |title=Large-cell calcifying Sertoli cell tumor of the testis |journal=Am. J. Clin. Pathol. |volume=74 |issue=5 |pages=607–19 |date=November 1980 |pmid=7446466 |doi=10.1093/ajcp/74.5.607 |url=}}</ref> | |||
====Granulosa cell tumor==== | |||
*It is rare type of testicular cancer. | |||
* Seen mostly in the [[ovary]] | |||
Adult type: | |||
*It rarely [[Metastasize|metastasizes]]. | |||
*Seen in the 4th decade of life.<ref name="pmid17628299">{{cite journal |vauthors=Ditonno P, Lucarelli G, Battaglia M, Mancini V, Palazzo S, Trabucco S, Bettocchi C, Paolo Selvaggi F |title=Testicular granulosa cell tumor of adult type: a new case and a review of the literature |journal=Urol. Oncol. |volume=25 |issue=4 |pages=322–5 |date=2007 |pmid=17628299 |doi=10.1016/j.urolonc.2006.08.019 |url=}}</ref> | |||
Juvenile type | |||
* It is seen mostly in [[infants]].<ref name="pmid10688023">{{cite journal |vauthors=Garrett JE, Cartwright PC, Snow BW, Coffin CM |title=Cystic testicular lesions in the pediatric population |journal=J. Urol. |volume=163 |issue=3 |pages=928–36 |date=March 2000 |pmid=10688023 |doi= |url=}}</ref> | |||
* It is mostly [[benign]] | |||
* It has an underlined association with [[sex chromosome]] [[abnormalities]], [[ambiguous genitalia]], and ipsilateral [[cryptorchidism]].<ref name="pmid8154078">{{cite journal |vauthors=Gourlay WA, Johnson HW, Pantzar JT, McGillivray B, Crawford R, Nielsen WR |title=Gonadal tumors in disorders of sexual differentiation |journal=Urology |volume=43 |issue=4 |pages=537–40 |date=April 1994 |pmid=8154078 |doi= |url=}}</ref> | |||
==Complications== | ==Complications== | ||
| Line 14: | Line 63: | ||
:* [[Brain]] | :* [[Brain]] | ||
* Post-surgery complications | * Post-surgery [[complications]] | ||
:* [[Bleeding]] | :* [[Bleeding]] | ||
:* [[Infection]] | :* [[Infection]] | ||
| Line 20: | Line 69: | ||
==Prognosis== | ==Prognosis== | ||
* Between 2004 and 2010, the 5-year relative survival of patients with testicular cancer was 96.6%.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | * Between 2004 and 2010, the 5-year relative [[Survival rate|survival]] of [[patients]] with testicular cancer was 96.6%.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | ||
* When stratified by age, the 5-year relative survival of patients with testicular cancer was 95.4% and 86.4% for patients <65 and ≥ 65 years of age respectively.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | * When stratified by age, the 5-year relative [[Survival rate|survival]] of [[patients]] with testicular cancer was 95.4% and 86.4% for [[patients]] <65 and ≥ 65 years of age respectively.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | ||
* The survival of patients with testicular cancer varies with the stage of the disease. Shown below is a table depicting the 5-year relative survival by the stage of testicular cancer:<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | * The survival of patients with testicular cancer varies with the stage of the [[disease]]. Shown below is a table depicting the 5-year relative [[Survival rate|survival]] by the stage of testicular cancer:<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | ||
{| style="cellpadding=0; cellspacing= 0; width: 600px;" | {| style="cellpadding=0; cellspacing= 0; width: 600px;" | ||
|- | |- | ||
! style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Stage'''!! style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" | '''5-year relative survival (%), (2004-2010)''' | |||
|- | |- | ||
! style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''All stages''' | |||
| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |95.3% | |||
|- | |- | ||
! style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''Localized''' | |||
| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |99.2% | |||
|- | |- | ||
! style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''Regional''' | |||
| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |96% | |||
|- | |- | ||
! style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''Distant''' | |||
| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |73.1% | |||
|- | |- | ||
! style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''Unstaged''' | |||
| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |78.8% | |||
|} | |} | ||
Latest revision as of 10:03, 1 July 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Gertrude Djouka, M.D.[2],Rim Halaby, M.D. [3] Shanshan Cen, M.D. [4]
|
Testicular cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Testicular cancer natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Testicular cancer natural history, complications and prognosis |
|
FDA on Testicular cancer natural history, complications and prognosis |
|
CDC on Testicular cancer natural history, complications and prognosis |
|
Testicular cancer natural history, complications and prognosis in the news |
|
Blogs on Testicular cancer natural history, complications and prognosis |
|
Risk calculators and risk factors for Testicular cancer natural history, complications and prognosis |
Overview
Prognosis of testicular cancer is generally good, and the 5-year survival rate is approximately 96.6% (2004-2010). Common complications of testicular cancer include metastasis, bleeding, infection, and infertility.
Natural History
Germ cell testicular tumor
Seminoma
- Seminoma tends to occur in middle aged people.
- Rarely metastasize.[1]
- Affects people in their 15 and 35 years old
Embryonal Carcinoma
- Median age is 30 years old[1]
- Has most of the component of mixed non seminoma germ tumor[1]
- Tend to metastasize early to lungs, retroperitoneum, and liver[2]
Choriocarcinoma
- Patient presents with early symptoms if there are metastatic lesions.[3]
- Early metastasis through hematogenous route
- Tends to metastasize to lungs, brain, liver, peritoneum, and others.
- Affects most male patients in the second and third decade of their life.[4]
Yolk Sac tumor
- Mostly seen in children less than 2 years old[5]
- Patients are usually asymptomatic at onset[6]
- Tends to have elevated alpha fetoproteins (AFP)
Spermatocytic tumor
- Seen in old men
- Barely metastasize[7]
Sex cord stromal testicular tumor
Leydig cell tumor
- Seen mostly in any age
- Benign in boys aged 5 to 10 years old and malignant in adults aged 30 to 60 years old[8][9]
- It metastasizes in the regional lymph nodes such as iliac, inguinal and retroperitonial nodes[10]
Sertoli cell tumor
- It affects both infants and older adults
- Malignancy is seen in infants in presence of metastasis[9]
- Sertoli cell tumor is associated with Peutz-Jeghers syndrome and Carney complex.
- large cell calcifying sertoli cell tumor is associated with Carney's complex (syndrome of myxoma, spotty pigmentation and endocrine overactivity).[11][12]
Granulosa cell tumor
- It is rare type of testicular cancer.
- Seen mostly in the ovary
Adult type:
- It rarely metastasizes.
- Seen in the 4th decade of life.[13]
Juvenile type
- It is seen mostly in infants.[14]
- It is mostly benign
- It has an underlined association with sex chromosome abnormalities, ambiguous genitalia, and ipsilateral cryptorchidism.[15]
Complications
Common complications of testicular cancer include:
- Abdomen
- Lungs
- Retroperitoneal area
- Brain
- Post-surgery complications
Prognosis
- Between 2004 and 2010, the 5-year relative survival of patients with testicular cancer was 96.6%.[16]
- When stratified by age, the 5-year relative survival of patients with testicular cancer was 95.4% and 86.4% for patients <65 and ≥ 65 years of age respectively.[16]
- The survival of patients with testicular cancer varies with the stage of the disease. Shown below is a table depicting the 5-year relative survival by the stage of testicular cancer:[16]
| Stage | 5-year relative survival (%), (2004-2010) |
|---|---|
| All stages | 95.3% |
| Localized | 99.2% |
| Regional | 96% |
| Distant | 73.1% |
| Unstaged | 78.8% |
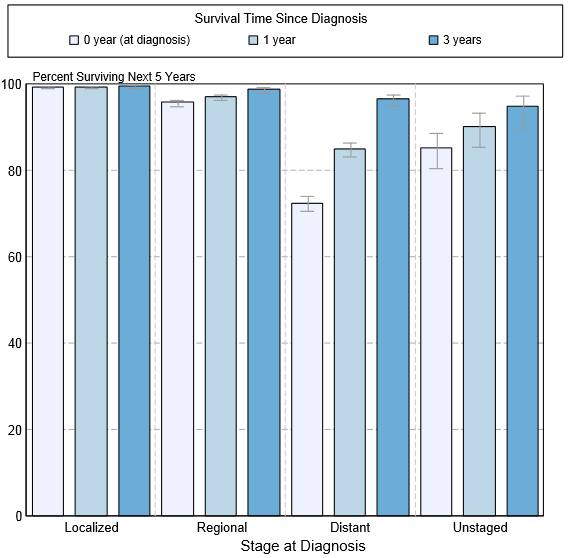
- Shown below is an image depicting the 5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 1998 and 2010 of testicular cancer by stage at diagnosis according to SEER. These graphs are adapted from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.[16]
References
- ↑ 1.0 1.1 1.2 Howitt BE, Berney DM (December 2015). "Tumors of the Testis: Morphologic Features and Molecular Alterations". Surg Pathol Clin. 8 (4): 687–716. doi:10.1016/j.path.2015.07.007. PMID 26612222.
- ↑ Ishida M, Hasegawa M, Kanao K, Oyama M, Nakajima Y (February 2009). "Non-palpable testicular embryonal carcinoma diagnosed by ultrasound: a case report". Jpn. J. Clin. Oncol. 39 (2): 124–6. doi:10.1093/jjco/hyn141. PMID 19066212.
- ↑ Lowe K, Paterson J, Armstrong S, Walsh S, Groome M, Mowat C (October 2015). "Metastatic Testicular Choriocarcinoma: A Rare Cause of Upper GI Bleeding". ACG Case Rep J. 3 (1): 36–8. doi:10.14309/crj.2015.94. PMC 4612755. PMID 26504875.
- ↑ Lee SC, Kim KH, Kim SH, Lee NS, Park HS, Won JH (December 2009). "Mixed testicular germ cell tumor presenting as metastatic pure choriocarcinoma involving multiple lung metastases that was effectively treated with high-dose chemotherapy". Cancer Res Treat. 41 (4): 229–32. doi:10.4143/crt.2009.41.4.229. PMC 2802842. PMID 20057969.
- ↑ Coppes MJ, Rackley R, Kay R (1994). "Primary testicular and paratesticular tumors of childhood". Med. Pediatr. Oncol. 22 (5): 329–40. PMID 8127257.
- ↑ Wei Y, Wu S, Lin T, He D, Li X, Liu J, Liu X, Hua Y, Lu P, Wei G (December 2014). "Testicular yolk sac tumors in children: a review of 61 patients over 19 years". World J Surg Oncol. 12: 400. doi:10.1186/1477-7819-12-400. PMC 4326497. PMID 25547829.
- ↑ Bosl GJ, Motzer RJ (July 1997). "Testicular germ-cell cancer". N. Engl. J. Med. 337 (4): 242–53. doi:10.1056/NEJM199707243370406. PMID 9227931.
- ↑ Al-Agha OM, Axiotis CA (February 2007). "An in-depth look at Leydig cell tumor of the testis". Arch. Pathol. Lab. Med. 131 (2): 311–7. doi:10.1043/1543-2165(2007)131[311:AILALC]2.0.CO;2. PMID 17284120.
- ↑ 9.0 9.1 Dilworth JP, Farrow GM, Oesterling JE (May 1991). "Non-germ cell tumors of testis". Urology. 37 (5): 399–417. PMID 2024387.
- ↑ Grem JL, Robins HI, Wilson KS, Gilchrist K, Trump DL (1986). "Metastatic Leydig cell tumor of the testis. Report of three cases and review of the literature". Cancer. 58 (9): 2116–9. doi:10.1002/1097-0142(19861101)58:9<2116::aid-cncr2820580925>3.0.co;2-x. PMID 3756826.
- ↑ Washecka R, Dresner MI, Honda SA (March 2002). "Testicular tumors in Carney's complex". J. Urol. 167 (3): 1299–302. PMID 11832717.
- ↑ Proppe KH, Scully RE (November 1980). "Large-cell calcifying Sertoli cell tumor of the testis". Am. J. Clin. Pathol. 74 (5): 607–19. doi:10.1093/ajcp/74.5.607. PMID 7446466.
- ↑ Ditonno P, Lucarelli G, Battaglia M, Mancini V, Palazzo S, Trabucco S, Bettocchi C, Paolo Selvaggi F (2007). "Testicular granulosa cell tumor of adult type: a new case and a review of the literature". Urol. Oncol. 25 (4): 322–5. doi:10.1016/j.urolonc.2006.08.019. PMID 17628299.
- ↑ Garrett JE, Cartwright PC, Snow BW, Coffin CM (March 2000). "Cystic testicular lesions in the pediatric population". J. Urol. 163 (3): 928–36. PMID 10688023.
- ↑ Gourlay WA, Johnson HW, Pantzar JT, McGillivray B, Crawford R, Nielsen WR (April 1994). "Gonadal tumors in disorders of sexual differentiation". Urology. 43 (4): 537–40. PMID 8154078.
- ↑ 16.0 16.1 16.2 16.3 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.