Superior mesenteric artery syndrome: Difference between revisions
m (Robot: Automated text replacement (-{{reflist}} +{{reflist|2}}, -<references /> +{{reflist|2}}, -{{WikiDoc Cardiology Network Infobox}} +)) |
Ochuko Ajari (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{SI} | |||
{{CMG}} | {{CMG}} | ||
{{Infobox Disease | {{Infobox Disease | ||
| Name = SMA Syndrome | | Name = SMA Syndrome | ||
| Line 11: | Line 10: | ||
}} | }} | ||
{{ | {{SK}} Cast syndrome | ||
==Overview== | |||
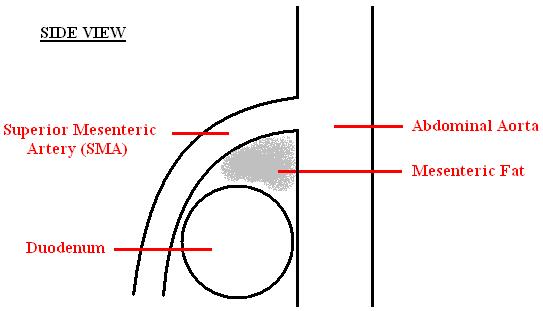
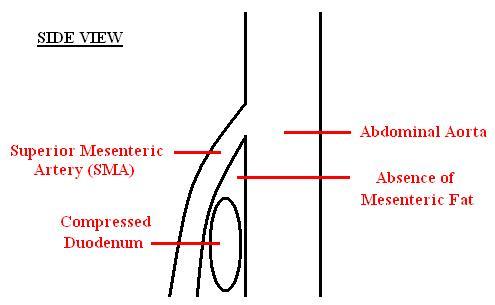
'''Superior mesenteric artery (SMA) syndrome''' is a rare, life-threatening [[gastrointestinal]] disorder characterized by a compression of the third portion of the [[duodenum]] by the [[abdominal aorta]] and the overlying [[superior mesenteric artery]]. The syndrome is typically caused by a decreased angle of 6°–25° between the aorta and the SMA (compared to a normal range of 38°-56°) due to a lack of retroperitoneal fat. <ref name="eMedicine"/> | '''Superior mesenteric artery (SMA) syndrome''' is a rare, life-threatening [[gastrointestinal]] disorder characterized by a compression of the third portion of the [[duodenum]] by the [[abdominal aorta]] and the overlying [[superior mesenteric artery]]. The syndrome is typically caused by a decreased angle of 6°–25° between the aorta and the SMA (compared to a normal range of 38°-56°) due to a lack of retroperitoneal fat. <ref name="eMedicine"/> | ||
Revision as of 19:33, 26 January 2015
{{SI} Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
| SMA Syndrome | |
 | |
|---|---|
| Abdominal and pelvic CT scan showing duodenal compression (black arrow) by the abdominal aorta and the superior mesenteric artery. |
Synonyms and keywords: Cast syndrome
Overview
Superior mesenteric artery (SMA) syndrome is a rare, life-threatening gastrointestinal disorder characterized by a compression of the third portion of the duodenum by the abdominal aorta and the overlying superior mesenteric artery. The syndrome is typically caused by a decreased angle of 6°–25° between the aorta and the SMA (compared to a normal range of 38°-56°) due to a lack of retroperitoneal fat. [1]
SMA syndrome was first described in 1842 by Carl Freiherr von Rokitansky, currently estimated to impact only 0.013% of the American population. [1] Despite 400 cases reported in English-language medical literature, recognition of SMA syndrome as a distinct clinical entity is controversial, [2] with some in the medical community doubting its existence entirely.[1] Wilkie published the first comprehensive series of 75 patients in 1927.[3]
SMA syndrome is also known as Wilkie's syndrome, cast syndrome, mesenteric root syndrome, chronic duodenal ileus and intermittent arterio-mesenteric occlusion.[4] It is a distinct disease from Nutcracker syndrome, which is the entrapment of the left renal vein between the abdominal aorta and the SMA.
Symptoms
Symptoms include early satiety, nausea, bilious vomiting of large quantities of partially undigested food, postprandial abdominal pain, eructation, external hypersensitivity of the abdominal area, and marked weight loss.[5] Weight loss, in turn, increases the duodenal compression, spurring a vicious cycle.[6] Symptoms are partially relieved when the patient is in the left lateral decubitus or knee-to-chest position. A Hayes maneuver (pressure applied below the umbilicus in cephalad and dorsal direction) elevates the root of the SMA, also easing the constriction. Symptoms are often aggravated when the patient is in the supine (face up) position.[5]
-
A diagram of a healthy mesenteric angle.
-
A diagram of a compressed duodenum due to a reduced mesenteric angle.
Causes
SMA syndrome can be triggered by any condition involving the dramatic reduction of the mesenteric angle. Patients predominantly have a history of chronic abdominal complaints, with intermittent exacerbations depending on the cause and grade of duodenal compression. Possibilities usually include constitutional genetic factors (such as aesthenic body build, an abnormally high and fixed position of the ligament of Treitz, or an unusually low origin of the SMA) coupled with any of the following: poor motility of the digestive tract [4], dietary disorders such as anorexia or malabsorption, exaggerated lumbar lordosis, visceroptosis, abdominal wall laxity, rapid linear growth without compensatory weight gain (particularly in teenagers), rapid severe weight loss, starvation, catabolic states (e.g. cancer and burns), prolonged bed rest, application of body casts, spinal cord injury, or scoliosis surgery.[1]
Demographics
Eight of ten patients are thin and sickly. Females are impacted twice as often as males, with 75% of cases occurring between the ages of ten and 30.[1]
Mortality
Delay in the diagnosis of SMA syndrome can result in death by malnutrition, dehydration, electrolyte abnormalities, or intestinal perforation.[1]
Diagnosis
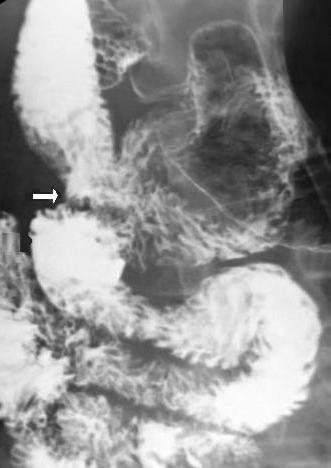
Diagnosis of SMA Syndrome is very difficult, and usually one of exclusion. Diagnosis may follow X-ray examination revealing duodenal dilation followed by abrupt constriction proximal to the overlying superior mesenteric artery, as well as a delay in transit of four to six hours through the gastroduodenal region. Suggested exams include abdominal and pelvic Computed Tomography (CT) scan and upper gastrointestinal series (UGI). Endoscopy should be used to rule out other causes of obstruction. Despite the name of the syndrome, it is not a vascular disease. Vascular imaging studies of the abdomen, including computed tomography and contrast angiography, are often normal. In the case of spinal cord injury, impaired abdominal sensation due to nerve damage makes the clinical picture even more obscure. [7]
-
Upper gastrointestinal series showing duodenojejunostomy (white arrow).
-
Upper gastrointestinal series showing duodenal dilation (white arrow).
Treatment
In mild or acute cases, conservative treatment should be attempted first, involving the reversal or removal of the precipitating factor with proper nutrition and replacement of fluid and electrolytes either by surgically-inserted jejunal feeding tube, nasogastric intubation, or peripherally inserted central catheter (PICC line) administering total parenteral nutrition (TPN). Symptoms typically improve after restoration of weight.[8] If conservative treatment fails, or if the case is severe or chronic, surgical intervention is required. The first operation for SMA syndrome, duodenojejunostomy, was proposed in 1907 by Bloodgood.[5] This open surgery involves the creation of an alternate route between the duodenum and the jejunum,[9] bypassing the compression caused by the abdominal aorta and the superior mesenteric artery. Although invasive, duodenojejunostomy has a 90% success rate.[1]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Avinash Shetty (2006-07-16). "Superior Mesenteric Artery Syndrome". eMedicine. WebMD. Retrieved 2008-04-09.
- ↑ Cohen LB, Field SP, Sachar DB (1985). "The superior mesenteric artery syndrome. The disease that isn't, or is it?". J. Clin. Gastroenterol. 7 (2): 113–6. PMID 4008904.
- ↑ Welsch T, Büchler MW, Kienle P (2007). "Recalling superior mesenteric artery syndrome". Dig Surg. 24 (3): 149–56. doi:10.1159/000102097. PMID 17476104.
- ↑ 4.0 4.1 Laffont I, Bensmail D, Rech C, Prigent G, Loubert G, Dizien O (2002). "Late superior mesenteric artery syndrome in paraplegia: case report and review". Spinal Cord. 40 (2): 88–91. doi:10.1038/sj.sc.3101255. PMID 11926421.
- ↑ 5.0 5.1 5.2 Baltazar U, Dunn J, Floresguerra C, Schmidt L, Browder W (2000). "Superior mesenteric artery syndrome: an uncommon cause of intestinal obstruction". South. Med. J. 93 (6): 606–8. PMID 10881780.Free full text with registration at Medscape
- ↑ "S: Superior mesenteric artery syndrome". GASTROLAB Digestive Dictionary. GASTROLAB. April 1, 2008. Retrieved 2008-04-09.
- ↑ Roth, Eliot (1991). "Superior mesenteric artery syndrome in acute traumatic quadriplegia: case reports and literature review". Arch Phys Med Rehabil. 2 (6): 417–20. Text "PMID: 2059111 " ignored (help); Unknown parameter
|coauthors=ignored (help); Unknown parameter|month=ignored (help) - ↑ Manu N, Martin L (2006). "Weight Loss Induced Small Bowel Obstruction". The Internet Journal of Gastroenterology. 4 (2).
- ↑ "Duodenojejunostomy". The Free Dictionary. Farlex. Retrieved 2008-04-09.