Streptococcus pneumoniae infection: Difference between revisions
Jump to navigation
Jump to search
| Line 42: | Line 42: | ||
==Treatment== | ==Treatment== | ||
[[Streptococcus pneumoniae medical therapy|Medical Therapy]] | [[Streptococcus pneumoniae primary prevention|Primary Prevention]] | [[Streptococcus pneumoniae secondary prevention|Secondary Prevention]] | [[Streptococcus pneumoniae cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Streptococcus pneumoniae future or investigational therapies|Future or Investigational Therapies]] | [[Streptococcus pneumoniae medical therapy|Medical Therapy]] | [[Streptococcus pneumoniae primary prevention|Primary Prevention]] | [[Streptococcus pneumoniae secondary prevention|Secondary Prevention]] | [[Streptococcus pneumoniae cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Streptococcus pneumoniae future or investigational therapies|Future or Investigational Therapies]] | ||
==Antimicrobial therapy== | |||
:* Streptococcus pneumonia <ref>{{cite book | last = Bartlett | first = John | title = Johns Hopkins ABX guide : diagnosis and treatment of infectious diseases | publisher = Jones and Bartlett Learning | location = Burlington, MA | year = 2012 | isbn = 978-1449625580 }}</ref> | |||
::* (1) '''Lung (pneumonia)''' | |||
:::* Community-acquired pneumonia | |||
::::* [[Penicillin]] sensitive (minimum inhibitory concentration ≤ 2) | |||
:::::* Preferred regimen: [[Penicillin G]] 1-2 MU q6h IV {{or}} [[Ceftriaxone]] 2 g IV q24h {{or}} [[Cefotaxime]] 1-2 g IV q6-8h. | |||
:::::: Oral agents: [[Penicillin V]] 500 mg PO qid, [[Amoxicillin]] 500-1000 mg PO tid, [[Cefpodoxime]] 200 mg PO bd, [[Cefprozil]] 500 mg PO bd, [[Cefditoren]] 400 mg PO bd, [[Cefdinir]] 300 mg PO bd, {{or}} [[Doxycycline]] 100 mg PO bd. | |||
::::* [[Penicillin]]-resistant ([[Penicillin]] minimum inhibitory concentration >8) | |||
:::::* Preferred regimen:: [[Levofloxacin]] (Levaquin) 750 mg {{or}} [[Moxifloxacin]] (Avelox) 400 mg IV/PO q24h, [[Telithromycin]] (Ketek) 800 mg PO qd, [[Ceftriaxone]] IV, [[Cefotaxime]] IV, [[Vancomycin]] 15 mg/kg IV q12h {{or}} [[Linezolid]] 600 mg IV/PO q12h. | |||
::* (2)'''Sinuses (sinusitis)''' | |||
:::* Sinusitis (empiric therapy) | |||
::::* Preferred regimen: [[amoxicillin]] 500-1000 mg PO tid {{or}} [[Amoxicillin]]/[[Clavulanate]] 875/125 mg PO bd. | |||
:::* Acute exacerbations of chronic bronchitis | |||
::::* Preferred regimen: [[amoxicillin]] 2-3 PO g/day or [[Doxycycline]] 100 mg PO bd. | |||
::* (3)'''Middle ear (otitis media)''' | |||
::* (4)'''Bronchi (acute exacerbation of chronic bronchitis)''' | |||
::* (5)'''CNS (meningitis)''' | |||
:::* Empiric therapy | |||
::::* Preferred regimen: [[Vancomycin]] 15 mg/kg/day IV q12h {{and}} [[Ceftriaxone]] 2 g IV q12h {{or}} [[Cefotaxime]] 2 g IV q4h or 3 g q6h. | |||
:::* Penicillin sensitive (minimum inhibitory concentration ≤ 0.06) | |||
::::* Preferred regimen: [[Ceftriaxone]] 2 g IV q12h, {{or}} [[Cefotaxime]] 2 g IV q4h or 3 g IV q6h. | |||
:::* Penicillin resistant (minimum inhibitory concentration ≥ 0.12) or beta-lactam hypersensitivity | |||
::::* Preferred regimen: [[Vancomycin]] 30-45 mg/kg/day IV. | |||
:::: Dexamethasone 0.15 mg/kg IV q6h for 2-4 days starting 10-20 min before antibiotic. | |||
::* (6)'''Peritoneum (spontaneous bacterial peritonitis)''' | |||
::* (7)'''Pericardium (purulent pericarditis)''' | |||
::* (8)'''Skin (cellulitis)''' | |||
::* (9)'''Eye (conjunctivitis)''' | |||
::* Prevention | |||
::: Pneumovax (23-valent) prevents bacteremia; impact on rates of CAP are modest or nil. | |||
::: Prevnar vaccine for children <2 yrs age prevents invasive pneumococcal infection in adults by herd effect. Impact is impressive with rates of invasive pneumococcal infection down 80% in peds and 20-40% in adults. | |||
::: Risk for bacteremia: splenectomy, HIV, smokers, black race, multiple myeloma, asthma. | |||
==References== | |||
{{reflist|2}} | |||
==Case Studies== | ==Case Studies== | ||
Revision as of 20:03, 29 June 2015
For patient information click here
| Streptococcus pneumoniae | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
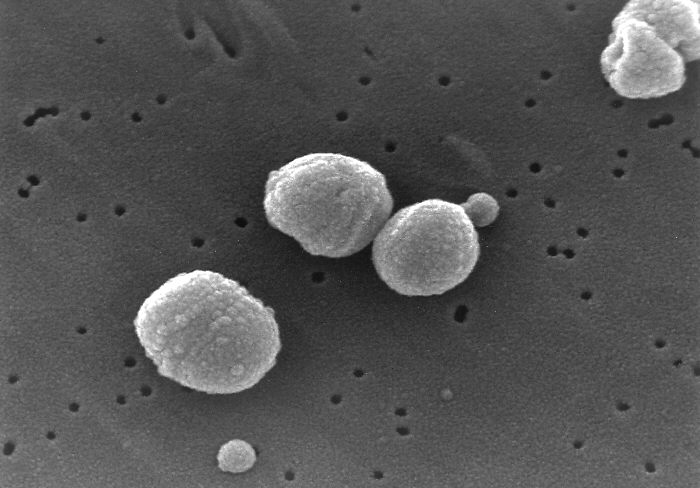 SEM micrograph of S. pneumoniae.
| ||||||||||||||
| Scientific classification | ||||||||||||||
| ||||||||||||||
| Binomial name | ||||||||||||||
| Streptococcus pneumoniae (Klein 1884) Chester 1901 |
Template:Streptococcus pneumoniae Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Historical Perspective
Pathophysiology
Causes
Differentiating Streptococcus pneumoniae from other Diseases
Epidemiology & Demographics
Risk Factors
Natural History, Complications & Prognosis
Diagnosis
History & Symptoms | Physical Examination | Lab Tests | Chest X Ray | CT | Other Imaging Findings | Other Diagnostic Studies
Treatment
Medical Therapy | Primary Prevention | Secondary Prevention | Cost-Effectiveness of Therapy | Future or Investigational Therapies
Antimicrobial therapy
- Streptococcus pneumonia [1]
- (1) Lung (pneumonia)
- Community-acquired pneumonia
- Penicillin sensitive (minimum inhibitory concentration ≤ 2)
- Preferred regimen: Penicillin G 1-2 MU q6h IV OR Ceftriaxone 2 g IV q24h OR Cefotaxime 1-2 g IV q6-8h.
- Oral agents: Penicillin V 500 mg PO qid, Amoxicillin 500-1000 mg PO tid, Cefpodoxime 200 mg PO bd, Cefprozil 500 mg PO bd, Cefditoren 400 mg PO bd, Cefdinir 300 mg PO bd, OR Doxycycline 100 mg PO bd.
- Penicillin-resistant (Penicillin minimum inhibitory concentration >8)
- Preferred regimen:: Levofloxacin (Levaquin) 750 mg OR Moxifloxacin (Avelox) 400 mg IV/PO q24h, Telithromycin (Ketek) 800 mg PO qd, Ceftriaxone IV, Cefotaxime IV, Vancomycin 15 mg/kg IV q12h OR Linezolid 600 mg IV/PO q12h.
- (2)Sinuses (sinusitis)
- Sinusitis (empiric therapy)
- Preferred regimen: amoxicillin 500-1000 mg PO tid OR Amoxicillin/Clavulanate 875/125 mg PO bd.
- Acute exacerbations of chronic bronchitis
- Preferred regimen: amoxicillin 2-3 PO g/day or Doxycycline 100 mg PO bd.
- (3)Middle ear (otitis media)
- (4)Bronchi (acute exacerbation of chronic bronchitis)
- (5)CNS (meningitis)
- Empiric therapy
- Preferred regimen: Vancomycin 15 mg/kg/day IV q12h AND Ceftriaxone 2 g IV q12h OR Cefotaxime 2 g IV q4h or 3 g q6h.
- Penicillin sensitive (minimum inhibitory concentration ≤ 0.06)
- Preferred regimen: Ceftriaxone 2 g IV q12h, OR Cefotaxime 2 g IV q4h or 3 g IV q6h.
- Penicillin resistant (minimum inhibitory concentration ≥ 0.12) or beta-lactam hypersensitivity
- Preferred regimen: Vancomycin 30-45 mg/kg/day IV.
- Dexamethasone 0.15 mg/kg IV q6h for 2-4 days starting 10-20 min before antibiotic.
- (6)Peritoneum (spontaneous bacterial peritonitis)
- (7)Pericardium (purulent pericarditis)
- (8)Skin (cellulitis)
- (9)Eye (conjunctivitis)
- Prevention
- Pneumovax (23-valent) prevents bacteremia; impact on rates of CAP are modest or nil.
- Prevnar vaccine for children <2 yrs age prevents invasive pneumococcal infection in adults by herd effect. Impact is impressive with rates of invasive pneumococcal infection down 80% in peds and 20-40% in adults.
- Risk for bacteremia: splenectomy, HIV, smokers, black race, multiple myeloma, asthma.
References
- ↑ Bartlett, John (2012). Johns Hopkins ABX guide : diagnosis and treatment of infectious diseases. Burlington, MA: Jones and Bartlett Learning. ISBN 978-1449625580.