St. Louis encephalitis epidemiology and demographics
|
St. Louis encephalitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
St. Louis encephalitis epidemiology and demographics On the Web |
|
American Roentgen Ray Society Images of St. Louis encephalitis epidemiology and demographics |
|
St. Louis encephalitis epidemiology and demographics in the news |
|
Blogs on St. Louis encephalitis epidemiology and demographics |
|
Risk calculators and risk factors for St. Louis encephalitis epidemiology and demographics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: : Vishnu Vardhan Serla M.B.B.S. [2]
Overview
Epidemiology and Demographics
St. Louis encephalitis virus (SLEV) is transmitted to humans through the bite of an infected mosquito. All residents of and visitors to areas where SLEV activity has been identified are at risk of SLEV infection, particularly persons who engage in outdoor work and recreational activities, and those living in low-income areas. Most SLEV infections are silent; clinical infections range in severity from mild nonspecific febrile illnesses to meningitis or encephalitis. The risk of severe disease and fatality increases with age. SLEV infection is thought to confer life-long immunity against re-infection.
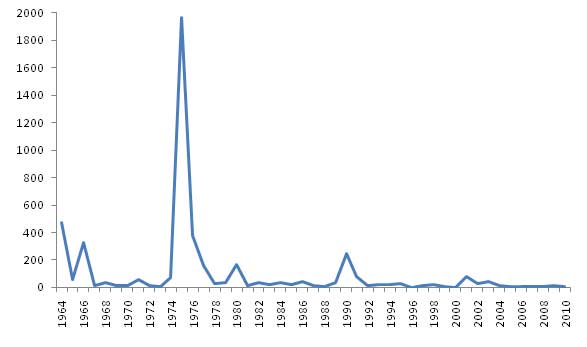
In the United States, the annual number of reported SLEV neuroinvasive disease cases reported fluctuates widely, as result of periodic epidemics. From 1964 through 2009, an average of 102 cases were reported annually (range 2-1,967). To ensure standardization of reporting across the country, CDC recommends that the national surveillance case definition be consistently applied by all state health departments.
In temperate areas of the United States, SLEV disease cases occur primarily in the late summer or early fall. In the southern states, where the climate is milder, cases can occur year round. Although the geographic range of the virus extends from Canada to Argentina, human cases have almost exclusively occurred in the United States. The majority of cases have occurred in eastern and central states, where episodic urban-centered outbreaks have recurred since the 1930s. In the rural west, transmission has followed a more endemic pattern. The largest epidemic of SLEV neuroinvasive disease ever recognized occurred in the United States in 1975, with nearly 2,000 cases reported, primarily from the central states in the Ohio-Mississippi River Basin.