Small cell carcinoma of the lung pathophysiology
|
Small Cell Carcinoma of the Lung Microchapters |
|
Differentiating Small Cell Carcinoma of the Lung from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Small cell carcinoma of the lung pathophysiology On the Web |
|
American Roentgen Ray Society Images of Small cell carcinoma of the lung pathophysiology |
|
Small cell carcinoma of the lung pathophysiology in the news |
|
Directions to Hospitals Treating Small cell carcinoma of the lung |
|
Risk calculators and risk factors for Small cell carcinoma of the lung pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alejandro Lemor, M.D. [2]
Overview
Small cell lung cancer (SCLC) is the most aggressive form of lung cancer and has the highest association with smoking of all lung cancers. It usually starts in the bronchi and expands through the bronchial mucosa. Although the cancer cells are small, they grow very quickly and create large tumors. These tumors often metastasize rapidly to other parts of the body, including the brain, liver, and bone.
Pathogenesis
Molecular Abnormalities
A mutation in p53 is found in almost all of cases of small cell carcinoma (75%-100%). Other molecular abnormalities have been described that influence in the development of small cell carcinoma, such as chromosome 3p deletion (present in 90% of cases), MYC amplification (in 30% of cases), BCL2 expression (in 95% of cases), GRP (gastrin-releasing peptide) expression , RB1 deletion (loss of RB1 protein), VEGF (vascular endothelial growth factor) expression, c-kit/SCFR (stem cell factor receptor) coexpression.[1]
The stem cell factor is expressed and secreted by the tumor cells of the small cell carcinoma and when it binds to c-kit, it stimulates the growth of the neoplastic cells, this is seen in 70% of patients with small cell lung cancer.[2]
There are 4 genes that are affected with chromosomal deletion, especially with chromosome 3p and play a role in the development of small cell carcinoma. The tumor suppressor genes are FHIT (fragile histidine triad gene), RASS effector homologue (RASSF1), retinoic acid receptor B and FUS1.
The FHIT affects the cell cycle control and proapoptosis by encoding an enzyme called diadenosine triphosphate hydrolase. [3] The RASSF1 stabilizes the cell cycle and induces G2-M arrest, preventing cells to grow rapidly.[4] The mutation in the FHIT and RASSF1 gene make the tumor cells grow quicker and uncontrolled.
Paraneoplastic Syndrome
- SCLC is one of the most common tumors associated with a paraneoplastic syndrome. The most common endocrine condition associated with SCLC is syndrome of inappropriate antidiuretic hormone (SIADH), where there is an excessive secretion of antidueretic hormone (ADH) which leads to hyponatremia.
- Other conditions that are related to small cell lung cancer are:
- Production of atrial natriuretic peptide (ANP) leading to hyponatremia, natriuresis and hypotension
- Ectopic ACTH production, which causes Cushing syndrome
- Lambert-Eaton syndrome due to the production of antibodies directed against the antigens of the neuromuscular junctions
Associated Conditions
Smoking
The association between smoking and lung cancer is well established; in fact, studies from the early 1950's have demonstrated anincreased risk of lung cancer with smoking. [5][6] In particular, SCLC is highly associated with smoking, even more than the other types of lung cancer.[7]
There are more than 60 carcinogens in a cigarette,[8] including radioisotopes from the radon decay sequence, nitrosamine, and benzopyrene. These carcinogens cause oxidative stress by generating reactive oxygen species and promote point mutations in different genes, especially in TP53 and KRAS. the events culminate in the development of neoplastic cells.[9] [10] In addition, nicotine appears to depress the immune response to malignant growth in exposed tissues.
Radon Exposure
There are several studies on the association between the exposure to radon and lung cancer.[11][12][13] This gas damages the epithelial lining of the lung by interacting directly with the cellular DNA (causing chromosomal damage and gene mutations) or indirectly through the effect of free radicals. Radon gas emits alpha particles that react with the water molecule, creating several reactive oxygen species that react with other molecules and cause biologic damage to the lung cells. [14][15] [16]
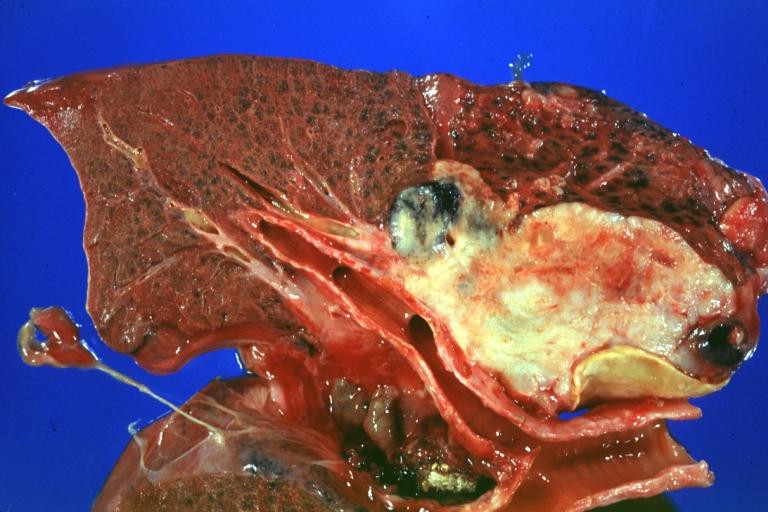
Gross Pathology
-
Gross fixed tissue opened bronchus at hilum showing tumor close-up.
-
Gross natural color photo of left upper lobe neoplasm extending into mediastinal pleura and surrounding portion of aorta node metastasis easily seen small cell carcinoma (unusual spindle cell areas)
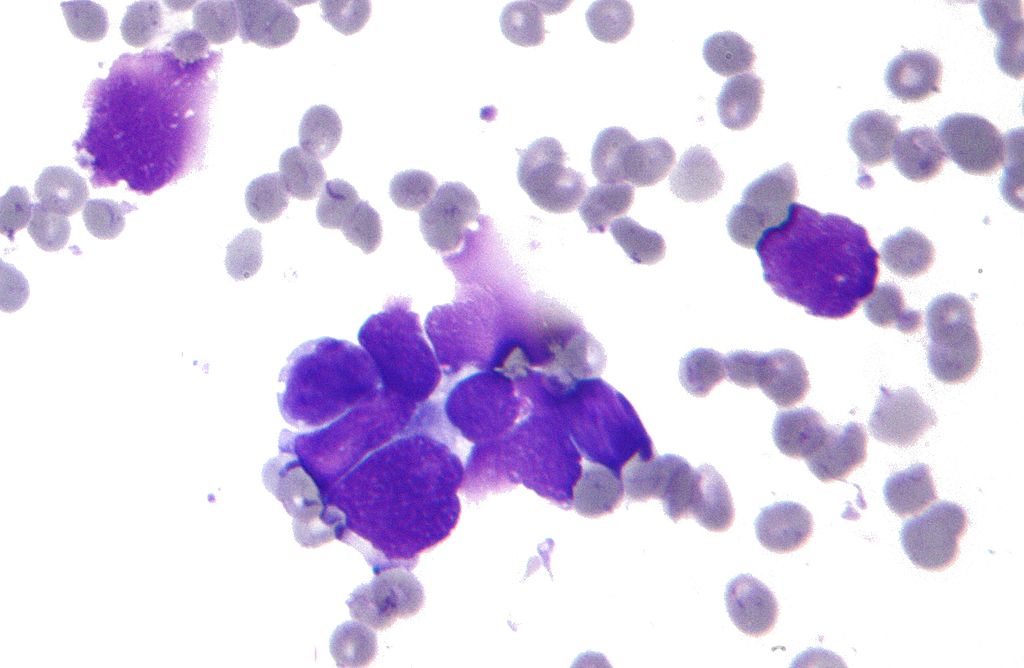
Microscopic Pathology
The tumor cells are small and round, but sometimes can be ovoid or spindle shaped. They have a scant cytoplasm with a high mitotic count and a hyperchromatic nuclei. Nearly all SCLC are immunoreactive for keratin, thyroid transcription factor 1, and epithelial membrane antigen. Neuroendocrine and neural differentiation result in the expression of dopa decarboxylase, calcitonin, neuron-specific enolase, chromogranin A, CD56 (also known as nucleosomal histone kinase 1 or neural-cell adhesion molecule), gastrin-releasing peptide, and insulin-like growth factor 1. One or more markers of neuroendocrine differentiation can be found in approximately 75% of SCLC. [17]
-
Histopathologic image of small cell carcinoma of the lung. CT-guided core needle biopsy. H & E stain.
-
Micrograph of a small-cell carcinoma of the lung showing cells with nuclear moulding, minimal amount of cytoplasm and stippled chromatin. FNA specimen. Field stain.
-
Anaplastic (microcellular, oat cell) carcinoma from the lung (histopathology)
-
Histopathologic image of small-cell carcinoma of the lung. CT-guided core needle biopsy.
-
Small Cell Carcinoma, Pleural FNA.
References
- ↑ Grace K. Dy & Alex A. Adjei (2002). "Novel targets for lung cancer therapy: part I". Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 20 (12): 2881–2894. PMID 12065566. Unknown parameter
|month=ignored (help) - ↑ K. Hibi, T. Takahashi, Y. Sekido, R. Ueda, T. Hida, Y. Ariyoshi, H. Takagi & T. Takahashi (1991). "Coexpression of the stem cell factor and the c-kit genes in small-cell lung cancer". Oncogene. 6 (12): 2291–2296. PMID 1722571. Unknown parameter
|month=ignored (help) - ↑ Yuri Pekarsky, Alexey Palamarchuk, Kay Huebner & Carlo M. Croce (2002). "FHIT as tumor suppressor: mechanisms and therapeutic opportunities". Cancer biology & therapy. 1 (3): 232–236. PMID 12432269. Unknown parameter
|month=ignored (help) - ↑ Rong Rong, Weixin Jin, Jennifer Zhang, M. Saeed Sheikh & Ying Huang (2004). "Tumor suppressor RASSF1A is a microtubule-binding protein that stabilizes microtubules and induces G2/M arrest". Oncogene. 23 (50): 8216–8230. doi:10.1038/sj.onc.1207901. PMID 15378022. Unknown parameter
|month=ignored (help) - ↑ R. DOLL & A. B. HILL (1950). "Smoking and carcinoma of the lung; preliminary report". British medical journal. 2 (4682): 739–748. PMID 14772469. Unknown parameter
|month=ignored (help) - ↑ Peter N. Lee, Barbara A. Forey & Katharine J. Coombs (2012). "Systematic review with meta-analysis of the epidemiological evidence in the 1900s relating smoking to lung cancer". BMC cancer. 12: 385. doi:10.1186/1471-2407-12-385. PMID 22943444.
- ↑ NCCN Clinical Practice Guidelines in Oncology. Small Cell Lung Cancer, version 2.2014
- ↑ Hecht, S (Oct 2003). "Tobacco carcinogens, their biomarkers and tobacco-induced cancer". Nature Reviews. Cancer. Nature Publishing Group. 3 (10): 733–744. doi:10.1038/nrc1190. PMID 14570033. Retrieved 2007-08-10.
- ↑ Pleasance, Erin D.; Stephens, Philip J.; O’Meara, Sarah; McBride, David J.; Meynert, Alison; Jones, David; Lin, Meng-Lay; Beare, David; Lau, King Wai; Greenman, Chris; Varela, Ignacio; Nik-Zainal, Serena; Davies, Helen R.; Ordoñez, Gonzalo R.; Mudie, Laura J.; Latimer, Calli; Edkins, Sarah; Stebbings, Lucy; Chen, Lina; Jia, Mingming; Leroy, Catherine; Marshall, John; Menzies, Andrew; Butler, Adam; Teague, Jon W.; Mangion, Jonathon; Sun, Yongming A.; McLaughlin, Stephen F.; Peckham, Heather E.; Tsung, Eric F.; Costa, Gina L.; Lee, Clarence C.; Minna, John D.; Gazdar, Adi; Birney, Ewan; Rhodes, Michael D.; McKernan, Kevin J.; Stratton, Michael R.; Futreal, P. Andrew; Campbell, Peter J. (2009). "A small-cell lung cancer genome with complex signatures of tobacco exposure". Nature. 463 (7278): 184–190. doi:10.1038/nature08629. ISSN 0028-0836.
- ↑ David M. DeMarini (2004). "Genotoxicity of tobacco smoke and tobacco smoke condensate: a review". Mutation research. 567 (2–3): 447–474. doi:10.1016/j.mrrev.2004.02.001. PMID 15572290. Unknown parameter
|month=ignored (help) - ↑ S. Darby, D. Hill, A. Auvinen, J. M. Barros-Dios, H. Baysson, F. Bochicchio, H. Deo, R. Falk, F. Forastiere, M. Hakama, I. Heid, L. Kreienbrock, M. Kreuzer, F. Lagarde, I. Makelainen, C. Muirhead, W. Oberaigner, G. Pershagen, A. Ruano-Ravina, E. Ruosteenoja, A. Schaffrath Rosario, M. Tirmarche, L. Tomasek, E. Whitley, H.-E. Wichmann & R. Doll (2005). "Radon in homes and risk of lung cancer: collaborative analysis of individual data from 13 European case-control studies". BMJ (Clinical research ed.). 330 (7485): 223. doi:10.1136/bmj.38308.477650.63. PMID 15613366. Unknown parameter
|month=ignored (help) - ↑ J. H. Lubin, J. D. Jr Boice, C. Edling, R. W. Hornung, G. R. Howe, E. Kunz, R. A. Kusiak, H. I. Morrison, E. P. Radford & J. M. Samet (1995). "Lung cancer in radon-exposed miners and estimation of risk from indoor exposure". Journal of the National Cancer Institute. 87 (11): 817–827. PMID 7791231. Unknown parameter
|month=ignored (help) - ↑ B. Grosche, M. Kreuzer, M. Kreisheimer, M. Schnelzer & A. Tschense (2006). "Lung cancer risk among German male uranium miners: a cohort study, 1946-1998". British journal of cancer. 95 (9): 1280–1287. doi:10.1038/sj.bjc.6603403. PMID 17043686. Unknown parameter
|month=ignored (help) - ↑ Harley, N. H.; Chittaporn, P.; Heikkinen, M. S. A.; Meyers, O. A.; Robbins, E. S. (2008). "Radon carcinogenesis: risk data and cellular hits". Radiation Protection Dosimetry. 130 (1): 107–109. doi:10.1093/rpd/ncn123. ISSN 0144-8420.
- ↑ Al-Zoughool, Mustafa; Krewski, Daniel (2009). "Health effects of radon: A review of the literature". International Journal of Radiation Biology. 85 (1): 57–69. doi:10.1080/09553000802635054. ISSN 0955-3002.
- ↑ Michael C. R. Alavanja (2002). "Biologic damage resulting from exposure to tobacco smoke and from radon: implication for preventive interventions". Oncogene. 21 (48): 7365–7375. doi:10.1038/sj.onc.1205798. PMID 12379879. Unknown parameter
|month=ignored (help) - ↑ National Cancer Institute: PDQ® Small Cell Lung Cancer Treatment. Bethesda, MD: National Cancer Institute. Available at: http://www.cancer.gov/cancertopics/pdq/treatment/small-cell-lung/healthprofessional.