|
|
| Line 1: |
Line 1: |
| == Patient information== | | ==Risk factors== |
| '''For the WikiDoc page for this topic, click [[Diarrhea|here]]'''
| | {{Family tree/start}} |
| | | {{Family tree | | | | | | B01 | | | |B01='''Contamination: Foodborne, waterborne and Animal exposure''' }} |
| {{Diarrhea (patient information)}} | |
| | |
| {{CMG}}; '''Assistant Editor-in-Chief:''' Meagan E. Doherty
| |
| | |
| ==Overview==
| |
| Diarrhea is loose, watery stools. A person with diarrhea typically passes stool more than three times a day. People with diarrhea may pass more than a quart of stool a day. Acute diarrhea is a common problem that usually lasts 1 or 2 days and goes away on its own without special treatment. Prolonged diarrhea persisting for more than 2 days may be a sign of a more serious problem and poses the risk of [[dehydration]]. Chronic diarrhea may be a feature of a chronic disease. Diarrhea can cause dehydration, which means the body lacks enough fluid to function properly. Dehydration is particularly dangerous in children and older people, and it must be treated promptly to avoid serious health problems. People of all ages can get diarrhea and the average adult has a bout of acute diarrhea about four times a year. In the United States, each child will have had seven to 15 episodes of diarrhea by age 5.
| |
| | |
| ==What are the symptoms of Diarrhea?==
| |
| Diarrhea may be accompanied by [[cramping]], [[abdominal pain]], [[bloating]], [[nausea]], or an urgent need to use the bathroom. Depending on the cause, a person may have a [[fever]] or bloody stools.
| |
| | |
| ==What are the causes of Diarrhea?==
| |
| Acute diarrhea is usually related to a bacterial, viral, or parasitic infection. Chronic diarrhea is usually related to functional disorders such as irritable bowel syndrome or inflammatory bowel disease.
| |
| | |
| A few of the more common causes of diarrhea include the following:
| |
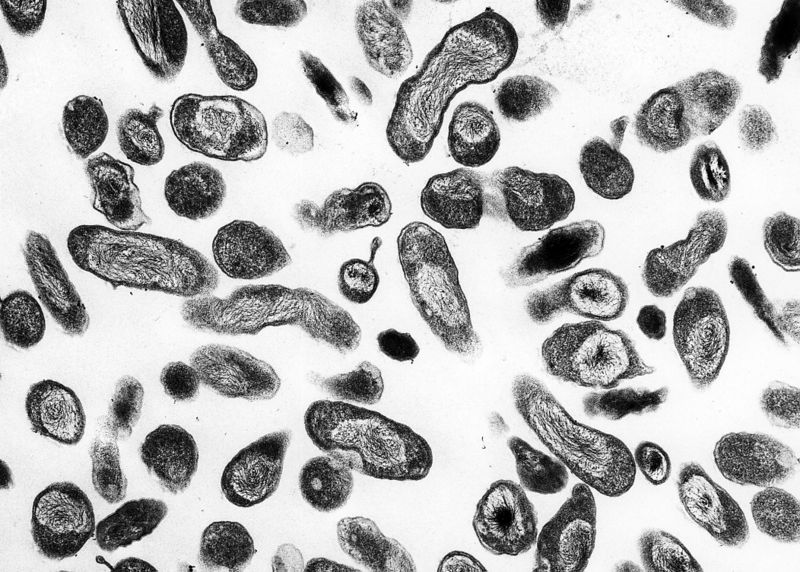
| *'''Bacterial infections'''. Several types of bacteria consumed through contaminated food or water can cause diarrhea. Common culprits include [[Campylobacter]], [[Salmonella]], [[Shigella]], and [[Escherichia coli]] (E. coli).
| |
| *'''Viral infections'''. Many viruses cause diarrhea, including [[rotavirus]], [[Norwalk virus]], [[cytomegalovirus]], [[herpes simplex virus]], and [[viral hepatitis]].
| |
| *'''Food intolerances'''. Some people are unable to digest food components such as artificial sweeteners and lactose—the sugar found in milk.
| |
| *'''Parasites'''. Parasites can enter the body through food or water and settle in the digestive system. Parasites that cause diarrhea include [[Giardia lamblia]], [[Entamoeba histolytica]], and [[Cryptosporidium]].
| |
| *'''Reaction to medicines'''. [[Antibiotics]], [[blood pressure medications]], [[cancer drugs]], and [[antacids]] containing [[magnesium]] can all cause diarrhea.
| |
| *'''Intestinal diseases'''. [[Inflammatory bowel disease]], [[colitis]], [[Crohn’s disease]], and [[celiac disease]] often lead to diarrhea.
| |
| *'''Functional bowel disorders'''. Diarrhea can be a symptom of [[irritable bowel syndrome]].
| |
| | |
| Some people develop diarrhea after stomach surgery or removal of the [[gallbladder]]. The reason may be a change in how quickly food moves through the [[digestive system]] after stomach surgery or an increase in [[bile]] in the [[colon]] after gallbladder surgery.
| |
| | |
| People who visit foreign countries are at risk for traveler’s diarrhea, which is caused by eating food or drinking water contaminated with bacteria, viruses, or parasites. Traveler’s diarrhea can be a problem for people visiting developing countries. Visitors to the United States, Canada, most European countries, Japan, Australia, and New Zealand do not face much risk for traveler’s diarrhea.
| |
| | |
| In many cases, the cause of diarrhea cannot be found. As long as diarrhea goes away on its own, an extensive search for the cause is not usually necessary.
| |
| | |
| ==Who is at risk for Diarrhea?==
| |
| Anyone can get diarrhea. This common problem can last a day or two or for months or years, depending on the cause. Most people get better on their own, but diarrhea can be serious for babies and older people if lost fluids are not replaced. Many people throughout the world die from diarrhea because of the large volume of water lost and the accompanying loss of salts.
| |
| | |
| ==Diagnosis==
| |
| Diagnostic tests to find the cause of diarrhea may include the following:
| |
| *'''Medical history and physical examination.''' The doctor will ask you about your eating habits and medication use and will examine you for signs of illness.
| |
| *'''Stool culture.''' A sample of stool is analyzed in a laboratory to check for [[bacteria]], [[parasites]], or other signs of disease and infection.
| |
| *'''Blood tests.''' Blood tests can be helpful in ruling out certain diseases.
| |
| *'''Fasting tests.''' To find out if a food intolerance or allergy is causing the diarrhea, the doctor may ask you to avoid [[lactose]], [[carbohydrates]], wheat, or other foods to see whether the diarrhea responds to a change in diet.
| |
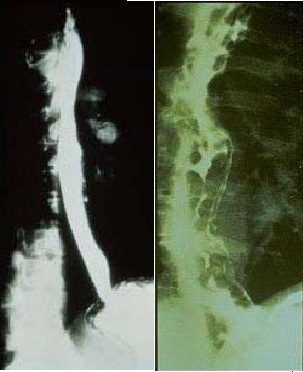
| *'''Sigmoidoscopy'''. For this test, the doctor uses a special instrument to look at the inside of the [[rectum]] and lower part of the [[colon]].
| |
| *'''Colonoscopy'''. This test is similar to a [[sigmoidoscopy]], but it allows the doctor to view the entire [[colon]].
| |
| *'''Imaging tests'''. These tests can rule out structural abnormalities as the cause of diarrhea.
| |
| | |
| ==When to seek urgent medical care==
| |
| Diarrhea is not usually harmful, but it can become dangerous or signal a more serious problem. You should see the doctor if you experience any of the following:
| |
| * Diarrhea for more than 3 days
| |
| * Severe pain in the [[abdomen]] or [[rectum]]
| |
| * A [[fever]] of 102 degrees or higher
| |
| * Blood in your stool or black, tarry stools
| |
| * Signs of [[dehydration]]
| |
| | |
| ==Treatment options==
| |
| In most cases of diarrhea, replacing lost fluid to prevent [[dehydration]] is the only treatment necessary. Medicines that stop diarrhea may be helpful, but they are not recommended for people whose diarrhea is caused by a bacterial infection or parasite. If you stop the diarrhea before having purged the bacteria or parasite, you will trap the organism in the intestines and prolong the problem. Rather, doctors usually prescribe [[antibiotics]] as a first-line treatment. [[Viral infections]] are either treated with medication or left to run their course, depending on the severity and type of virus.
| |
| | |
| ===Tips About Food===
| |
| Until diarrhea subsides, try to avoid caffeine, milk products, and foods that are greasy, high in fiber, or very sweet. These foods tend to aggravate diarrhea.
| |
| | |
| As you improve, you can add soft, bland foods to your diet, including bananas, plain rice, boiled potatoes, toast, crackers, cooked carrots, and baked chicken without the skin or fat. For children, the pediatrician may also recommend a bland diet. Once the diarrhea has stopped, the pediatrician will likely encourage children to return to a normal and healthy diet if it can be tolerated.
| |
| | |
| ===Contraindicated medications===
| |
| {{MedCondContrPI
| |
| | |
| |MedCond =Diarrhea|Ethacrynic acid}}
| |
| | |
| ==Where to find medical care for Diarrhea==
| |
| [http://maps.google.com/maps?f=q&hl=en&geocode=&q={{urlencode:{{#if:{{{1|}}}|{{{1}}}|yourdisease}}}}&sll=37.0625,-95.677068&sspn=65.008093,112.148438&ie=UTF8&ll=37.0625,-95.677068&spn=91.690419,149.414063&z=2&source=embed Directions to Hospitals Treating Diarrhea]
| |
| | |
| ==Prevention of Diarrhea==
| |
| * Wash your hands often, especially after going to the bathroom and before eating.
| |
| * Teach children to not put objects in their mouth.
| |
| * When taking antibiotics, try eating food with Lactobacillus acidophilus, a healthy bacteria. This helps replenish the good bacteria that antibiotics can kill. Yogurt with active or live cultures is a good source of this healthy bacteria.
| |
| * Use alcohol-based hand gel frequently.
| |
| | |
| Traveler’s diarrhea happens when you consume food or water contaminated with bacteria, viruses, or parasites. You can take the following precautions to prevent traveler’s diarrhea when you travel outside of the United States:
| |
| * Do not drink tap water or use it to brush your teeth.
| |
| * Do not drink unpasteurized milk or dairy products.
| |
| * Do not use ice made from tap water.
| |
| * Avoid all raw fruits and vegetables, including lettuce and fruit salads, unless they can be peeled and you peel them yourself.
| |
| * Do not eat raw or rare meat and fish.
| |
| * Do not eat meat or shellfish that is not hot when served.
| |
| * Do not eat food from street vendors.
| |
| | |
| You can safely drink bottled water—if you are the one to break the seal—along with carbonated soft drinks, and hot drinks such as coffee or tea.
| |
| | |
| Depending on where you are going and how long you will stay, your doctor may recommend that you take antibiotics before leaving to protect you from possible infection.
| |
| | |
| ==What to expect (Outlook/Prognosis)==
| |
| The Prognosis for diarrhea is usually good. Diarrhea is common and usually goes away on its own unless it is an underlying symptom of a chronic disease. It is important to replace lost fluid due to diarrhea because if you become severely dehydrated it can be fatal.
| |
| | |
| ==Sources==
| |
| http://digestive.niddk.nih.gov/ddiseases/pubs/diarrhea/
| |
| | |
| [[Category:Patient information]]
| |
| [[Category:primary care]]
| |
| [[Category:Gastroenterology]]
| |
| [[Category:Water-borne diseases]]
| |
| [[Category:Digestive disease symptoms]]
| |
| [[Category:Conditions diagnosed by stool test]]
| |
| | |
| | |
| | |
| {{WH}}
| |
| {{WS}}
| |
| | |
| ==Pathophysiology Diarrhea==
| |
| Normal fluid intake for an adult is about 2 L/d. The average amount of gastrointestinal secretions (composed of salivary glands, gastric, biliary, and pancreatic secretions) is 7-8 L/d, depending on the weight and age. The absorptive surface of the small intestine is formed by villis that reabsorb the majority of secreted water and electrolytes. The small intestine absorbs 75% of upper GI tract secretions. The rest of the secretions absorb in the large intestine. Colon absorbs 90% of its exposed volume, means that colon is the most effective absorbing organ in the GI system.<br>
| |
| Decrease in the small intestine absorption, regardless of causes, may not cause diarrhea unless, there is a dysfunction in colon or the volume of the secretions exceeds the absorptive ability of the colon.
| |
| | |
| | |
| {{Family tree | | | | | | B01 | | | |B01='''[[CNS]] dysregulation and [[psychosocial factors]]''' }} | |
| {{Family tree | | | | | | |!| | | | | }} | | {{Family tree | | | | | | |!| | | | | }} |
| {{Family tree | | | | | | |!| | | | | }} | | {{Family tree | | | | | | |!| | | | | }} |
| Line 119: |
Line 11: |
| {{familytree |boxstyle=text-align: left; | | | | | | B01 | | | |B01= '''Environmental factors''': <br>•Diet <br>•[[Infections]]}} | | {{familytree |boxstyle=text-align: left; | | | | | | B01 | | | |B01= '''Environmental factors''': <br>•Diet <br>•[[Infections]]}} |
| {{Family tree/end}} | | {{Family tree/end}} |
| | |
| | |
| | ==Pathophysiology Diarrhea== |
| | Normal fluid intake for an adult is about 2 L/d. The average amount of gastrointestinal secretions (composed of salivary glands, gastric, biliary, and pancreatic secretions) is 7-8 L/d, depending on the weight and age. The absorptive surface of the small intestine is formed by villis that reabsorb the majority of secreted water and electrolytes. The small intestine absorbs 75% of upper GI tract secretions. The rest of the secretions absorb in the large intestine. Colon absorbs 90% of its exposed volume, means that colon is the most effective absorbing organ in the GI system.<br> |
| | Decrease in the small intestine absorption, regardless of causes, may not cause diarrhea unless, there is a dysfunction in colon or the volume of the secretions exceeds the absorptive ability of the colon. |
|
| |
|
| ==References== | | ==References== |
| Line 177: |
Line 74: |
| {{Reflist|2}} | | {{Reflist|2}} |
|
| |
|
| == Risk Factors ==
| | |
| * Antibiotic use
| |
| * High-risk sexual behavior (STDs)
| |
| * Immunosuppression
| |
| * Recent travel to endemic area
| |
| ===Pathophysiology prev=== | | ===Pathophysiology prev=== |
| <div style="-webkit-user-select: none;"> | | <div style="-webkit-user-select: none;"> |
| Line 193: |
Line 86: |
| {{CMG}} {{AE}} | | {{CMG}} {{AE}} |
|
| |
|
| == Risk Factors ==
| | |
| * Antibiotic use
| |
| * High-risk sexual behavior (STDs)
| |
| * Immunosuppression
| |
| * Recent travel to endemic area
| |
| ===Pathophysiology prev=== | | ===Pathophysiology prev=== |
| <div style="-webkit-user-select: none;"> | | <div style="-webkit-user-select: none;"> |
| Line 208: |
Line 97: |
| {{Cirrhosis}} | | {{Cirrhosis}} |
| {{CMG}} {{AE}} | | {{CMG}} {{AE}} |
|
| |
| == Risk Factors ==
| |
| * Antibiotic use
| |
| * High-risk sexual behavior (STDs)
| |
| * Immunosuppression
| |
| * Recent travel to endemic area
| |
|
| |
|
| |
|
| == History and Symptoms == | | == History and Symptoms == |
| Line 251: |
Line 133: |
|
| |
|
| ==Overview== | | ==Overview== |
|
| |
| ==Medical Therapy==
| |
| * Fluid resuscitation (oral, if not IV)
| |
| * Patients should be advised to do the following until symptoms subside:
| |
| ** Hydrate with liquids that are [[caffeine]] free and contain [[glucose]]
| |
| ** Avoid [[lactose]]
| |
| ** Chew gum that is free of [[sorbitol]]
| |
| ** Eat raw fruit
| |
| * For patients with [[lactose intolerance]], a lactose-free diet is advised
| |
| * For patients with malabsorption diseases, a gluten free diet is advised
| |
| * Consultation with [[oncology]], surgery and/or gastroenterology may be required for intestinal [[neoplasm]]
| |
| * Control blood sugar ([[diabetic neuropathy]])
| |
|
| |
| ===Empirical Therapy===
| |
| Empirical therapy is used as an initial treatment before diagnostic testing or after diagnostic testing has failed to confirm a diagnosis or when there is no specific treatment or when specific treatment fails to effect a cure.
| |
|
| |
| * Empirical trials of antimicrobial therapy like [[metronidazole]] for protozoal diarrhea or [[fluoroquinolone]] for enteric bacterial diarrhea if the prevalence of bacterial or protozoal infection is high in a specific community or situation.
| |
|
| |
| * Most cases of diarrhea, except for high-volume secretory states, respond to a sufficiently high dose of [[opium]] or [[morphine]]. [[Codeine]], synthetic opioids [[diphenoxylate]] and [[loperamide]] are less potent. However loperamide is generally used because of its less abuse potential.
| |
|
| |
| * The somatostatin analogue [[octreotide]] has proven effectiveness in [[carcinoid tumors]] and other peptide-secreting tumors, dumping syndrome, and chemotherapy-induced diarrhea.
| |
|
| |
| * Intraluminal agents include adsorbants, such as activated charcoal, and binding resins like [[bismuth]] and stool modifiers, such as medicinal fiber.
| |
|
| |
| ===Pharmacotherapy===
| |
| * [[Antibiotics]] (malabsorption diseases)
| |
| * [[Anticholinergics]] (IBS)
| |
| * Antimolality agents
| |
| * Antibiotic therapy (severe disease)
| |
| * [[Metoclopramide]] (diabetic neuropathy)
| |
| * Nonspecific antidiarrheal agents
| |
|
| |
| ===Symptomatic Treatment===
| |
| * Symptomatic treatment for diarrhea involves the patient consuming adequate amounts of water to replace that loss, preferably mixed with [[electrolyte]]s to provide essential [[salt]]s and some amount of [[nutrient]]s. For many people, further treatment is unnecessary.
| |
| * The following types of diarrhea indicate medical supervision is required:
| |
| ** Diarrhea in infants;
| |
| ** Moderate or severe diarrhea in young children;
| |
| ** Diarrhea associated with [[blood]];
| |
| ** Diarrhea that continues for more than two weeks;
| |
| ** Diarrhea that is associated with more general illness such as non-cramping [[abdominal pain]], [[fever]], [[weight loss]], etc;
| |
| ** [[Traveler's diarrhea|Diarrhea in travelers]], since they are more likely to have exotic infections such as parasites;
| |
| ** Diarrhea in food handlers, because of the potential to infect others;
| |
| ** Diarrhea in institutions such as hospitals, child care centers, or geriatric and convalescent homes.
| |
|
| |
| A severity score is used to aid diagnosis.<ref name="pmid2371542">{{cite journal |author=Ruuska T, Vesikari T |title=Rotavirus disease in Finnish children: use of numerical scores for clinical severity of diarrhoeal episodes |journal=Scand. J. Infect. Dis. |volume=22 |issue=3 |pages=259–67 |year=1990 |pmid=2371542 |doi=}}</ref>
| |
|
| |
| ===Pathogen Specific===
| |
| ====Immunocompetent====
| |
| *'''Bacterial''' <ref name="pmid11170940">{{cite journal| author=Guerrant RL, Van Gilder T, Steiner TS, Thielman NM, Slutsker L, Tauxe RV et al.| title=Practice guidelines for the management of infectious diarrhea. | journal=Clin Infect Dis | year= 2001 | volume= 32 | issue= 3 | pages= 331-51 | pmid=11170940 | doi=10.1086/318514 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11170940 }} </ref>
| |
|
| |
| :* '''1. Shigella species'''
| |
| ::*Preferred regimen (1):
| |
| :::*Adult dose: [[TMP-SMZ]], 160 and 800 mg, respectively bid for 3 days (if susceptible ) {{or}} [[Fluoroquinolone]] (e.g., 300 mg [[Ofloxacin]], 400 mg [[Norfloxacin]], {{or}} 500 mg [[Ciprofloxacin]] bid for 3 days)
| |
| :::*Pediatric dose: [[TMP-SMZ]], 5 and 25 mg/kg, respectively bid for 3 days
| |
|
| |
| ::*Preferred regimen (2):
| |
| :::*Adult dose: [[Nalidixic acid]] 1 g/d for 5 days {{or}} [[Ceftriaxone]]; [[Azithromycin]]
| |
| :::*Pediatric dose: [[Nalidixic acid]], 55 mg/kg/d for 5 days
| |
|
| |
| :*'''2. Non-typhi species of Salmonella'''
| |
| ::*Preferred regimen: Not recommended routinely, but if severe or patient is younger than 6 monthes or older than 50 year old or has prostheses, valvular heart disease, severe atherosclerosis, malignancy, or uremia, [[TMP-SMZ]] (if susceptible) {{or}} [[Fluoroquinolone]], bid for 5 to 7 days; [[Ceftriaxone]], 100 mg/kg/d in 1 or 2 divided doses
| |
|
| |
| :*'''3. Campylobacter species'''
| |
| ::*Preferred regimen: [[Erythromycin]] 500 mg bid for 5 days
| |
|
| |
| :*'''4. Escherichia coli species'''
| |
| ::*'''4.1. Enterotoxigenic'''
| |
| :::*Preferred regimen: [[TMP-SMZ]], 160 and 800 mg, respectively, bid, for 3 days (if susceptible), {{or}} [[Fluoroquinolone]] (e.g., 300 mg [[Ofloxacin]], 400 mg [[Norfloxacin]], or 500 mg [[Ciprofloxacin]] bid for 3 days)
| |
|
| |
| ::*'''4.2. Enteropathogenic'''
| |
| :::*Preferred regimen: [[TMP-SMZ]], 160 and 800 mg, respectively, bid, for 3 days (if susceptible), {{or}} [[Fluoroquinolone]] (e.g., 300 mg [[Ofloxacin]], 400 mg [[Norfloxacin]], or 500 mg [[Ciprofloxacin]] bid for 3 days)
| |
|
| |
| ::*'''4.3. Enteroinvasive'''
| |
| :::*Preferred regimen: [[TMP-SMZ]], 160 and 800 mg, respectively, bid, for 3 days (if susceptible), {{or}} [[Fluoroquinolone]] (e.g., 300 mg [[Ofloxacin]], 400 mg [[Norfloxacin]], or 500 mg [[Ciprofloxacin]] bid for 3 days)
| |
|
| |
| ::*'''4.4. Enterohemorrhagic'''
| |
| :::*Preferred regimen: Avoid antimotility drugs; role of antibiotics unclear, and administration should be avoided.
| |
|
| |
| :*'''5. Aeromonas/Plesiomonas'''
| |
| ::*Preferred regimen: [[TMP-SMZ]], 160 and 800 mg, respectively, bid for 3 days (if susceptible), [[Fluoroquinolone]] (e.g., 300 mg [[Ofloxacin]], 400 mg [[Norfloxacin]], or 500 mg [[Ciprofloxacin]] bid for 3 days)
| |
|
| |
| :*'''6. Yersinia species'''
| |
| ::*Preferred regimen: Antibiotics are not usually required; [[Deferoxamine]] therapy should be withheld; for severe infections or associated bacteremia treat as for immunocompromised hosts, using combination therapy with [[Doxycycline]], [[Aminoglycoside]], [[TMP-SMZ]], {{or}} [[Fluoroquinolone]]
| |
|
| |
| :*'''7. Vibrio cholerae O1 or O139'''
| |
| ::*Preferred regimen (1): [[Doxycycline]] 300-mg single dose
| |
| ::*Preferred regimen (2): [[Tetracycline]] 500 mg qid for 3 days
| |
| ::*Preferred regimen (3): [[TMP-SMZ]] 160 and 800 mg, respectively, bid for 3 days
| |
| ::*Preferred regimen (4): single-dose [[Fluoroquinolone]]
| |
|
| |
| :*'''8. Toxigenic Clostridium difficile'''
| |
| ::*Preferred regimen: Offending antibiotic should be withdrawn if possible; [[Metronidazole]], 250 mg qid to 500 mg tid for 3 to 10 days
| |
|
| |
| *'''Parasites''' <ref name="pmid11170940">{{cite journal| author=Guerrant RL, Van Gilder T, Steiner TS, Thielman NM, Slutsker L, Tauxe RV et al.| title=Practice guidelines for the management of infectious diarrhea. | journal=Clin Infect Dis | year= 2001 | volume= 32 | issue= 3 | pages= 331-51 | pmid=11170940 | doi=10.1086/318514 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11170940 }} </ref>
| |
| :*'''1. Giardia'''
| |
| ::*Preferred regimen: [[Metronidazole]] 250-750 mg tid for 7-10 days
| |
|
| |
| :*'''2. Cryptosporidium species'''
| |
| ::*Preferred regimen: If severe, consider [[Paromomycin]], 500 mg tid for 7 days
| |
|
| |
| :*'''3. Isospora species'''
| |
| ::*Preferred regimen: [[TMP-SMZ]], 160 and 800 mg, respectively, bid for 7 to 10 days
| |
|
| |
| :*'''4. Cyclospora species'''
| |
| ::*Preferred regimen: [[TMP/SMZ]], 160 and 800 mg, respectively, bid for 7 days
| |
|
| |
| :*'''5. Microsporidium species'''
| |
| ::*Preferred regimen: Not determined
| |
|
| |
| :*'''6. Entamoeba histolytica'''
| |
| ::*Preferred regimen (1): [[Metronidazole]] 750 mg tid for 5 to 10 days {{and}} [[Diiodohydroxyquinoline|Diiodohydroxyquin]] 650 mg tid for 20 days
| |
| ::*Preferred regimen (2): [[Metronidazole]] 750 mg tid for 5 to 10 days {{and}} [[Paromomycin]] 500 mg tid for 7 days
| |
|
| |
| ====Immunocompromised====
| |
| *'''Bacterial''' <ref name="pmid11170940">{{cite journal| author=Guerrant RL, Van Gilder T, Steiner TS, Thielman NM, Slutsker L, Tauxe RV et al.| title=Practice guidelines for the management of infectious diarrhea. | journal=Clin Infect Dis | year= 2001 | volume= 32 | issue= 3 | pages= 331-51 | pmid=11170940 | doi=10.1086/318514 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11170940 }} </ref>
| |
| :* '''1. Shigella species:'''
| |
| ::*Preferred regimen (1):
| |
| :::*Adult dose: [[TMP-SMZ]], 160 and 800 mg, respectively bid for 7 to 10 days (if susceptible ) {{or}} [[Fluoroquinolone]] (e.g., 300 mg [[Ofloxacin]], 400 mg [[Norfloxacin]], {{or}} 500 mg [[Ciprofloxacin]] bid for 7 to 10 days)
| |
| :::*Pediatric dose:[[TMP-SMZ]], 5 and 25 mg/kg, respectively bid for 7 to 10 days
| |
|
| |
| ::*Preferred regimen (2):
| |
| :::*Adult dose: [[Nalidixic acid]] 1 g/d for 7 to 10 days {{or}} [[Ceftriaxone]]; [[Azithromycin]]
| |
| :::*Pediatric dose: [[Nalidixic acid]], 55 mg/kg/d for 7 to 10 days
| |
|
| |
| :*'''2. Non-typhi species of Salmonella'''
| |
| ::*Preferred regimen: Not recommended routinely, but if severe or patient is younger than 6 monthes or older than 50 old or has prostheses, valvular heart disease, severe atherosclerosis, malignancy, or uremia, [[TMP-SMZ]] (if susceptible) {{or}} [[Fluoroquinolone]], bid for 14 days (or longer if relapsing); [[ceftriaxone]], 100 mg/kg/d in 1 or 2 divided doses
| |
|
| |
| :*'''3. Campylobacter species'''
| |
| ::*Preferred regimen: [[Erythromycin]], 500 mg bid for 5 days (may require prolonged treatment)
| |
|
| |
| :*'''4. Escherichia coli species'''
| |
| ::*'''4.1. Enterotoxigenic'''
| |
| :::*Preferred regimen: [[TMP-SMZ]], 160 and 800 mg, respectively, bid for 3 days (if susceptible), {{or}} [[Fluoroquinolone]] (e.g., 300 mg [[Ofloxacin]], 400 mg [[Norfloxacin]], or 500 mg [[Ciprofloxacin]] bid for 3 days) (Consider fluoroquinolone as for enterotoxigenic E. coli)
| |
|
| |
| ::*'''4.2. Enteropathogenic'''
| |
| :::*Preferred regimen: [[TMP-SMZ]], 160 and 800 mg, respectively, bid,for 3 days (if susceptible), {{or}} [[Fluoroquinolone]] (e.g., 300 mg [[Ofloxacin]], 400 mg [[Norfloxacin]], or 500 mg [[Ciprofloxacin]] bid for 3 days)
| |
|
| |
| ::*'''4.3. Enteroinvasive'''
| |
| :::*Preferred regimen: [[TMP-SMZ]], 160 and 800 mg, respectively, bid,for 3 days (if susceptible), {{or}} [[Fluoroquinolone]] (e.g., 300 mg [[Ofloxacin]], 400 mg [[Norfloxacin]], or 500 mg [[Ciprofloxacin]] bid for 3 days)
| |
|
| |
| ::*'''4.4. Enterohemorrhagic'''
| |
| :::*Preferred regimen: Avoid antimotility drugs; role of antibiotics unclear, and administration should be avoided.
| |
|
| |
| :*'''5. Aeromonas/Plesiomonas'''
| |
| ::*Preferred regimen: [[TMP-SMZ]], 160 and 800 mg, respectively, bid for 3 days (if susceptible), [[Fluoroquinolone]] (e.g., 300 mg [[ofloxacin]], 400 mg [[norfloxacin]], or 500 mg [[Ciprofloxacin]] bid for 3 days)
| |
|
| |
| :*'''6. Yersinia species'''
| |
| ::*Preferred regimen: [[Doxycycline]], [[Aminoglycoside]] (in combination) or [[TMP-SMZ]] or [[Fluoroquinolone]]
| |
|
| |
| :*'''7. Vibrio cholerae O1 or O139'''
| |
| ::*Preferred regimen: [[Doxycycline]], 300-mg single dose; or [[Tetracycline]], 500 mg qid for 3 days; or [[TMP-SMZ]], 160 and 800 mg, respectively, bid for 3 days; or single-dose [[Fluoroquinolone]]
| |
|
| |
| :*'''8. Toxigenic Clostridium difficile'''
| |
| ::*Preferred regimen: Offending antibiotic should be withdrawn if possible; [[Metronidazole]], 250 mg qid to 500 mg tid for 3 to 10 days
| |
|
| |
| *'''Parasites''' <ref name="pmid11170940">{{cite journal| author=Guerrant RL, Van Gilder T, Steiner TS, Thielman NM, Slutsker L, Tauxe RV et al.| title=Practice guidelines for the management of infectious diarrhea. | journal=Clin Infect Dis | year= 2001 | volume= 32 | issue= 3 | pages= 331-51 | pmid=11170940 | doi=10.1086/318514 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11170940 }} </ref>
| |
| :*'''1. Giardia'''
| |
| ::*Preferred regimen: [[Metronidazole]], 250-750 mg tid for 7-10 days
| |
|
| |
| :*'''2. Cryptosporidium species'''
| |
| ::*Preferred regimen: [[Paromomycin]], 500 mg tid for 14 to 28 days, then bid if needed; highly active antiretroviral therapy including a protease inhibitor is warranted for patients with AIDS
| |
|
| |
| :*'''3. Isospora species'''
| |
| ::*Preferred regimen: [[TMP-SMZ]], 160 and 800 mg, respectively, qid for 10 days, followed by [[TMP-SMZ]] thrice weekly, or weekly [[Sulfadoxine]] (500 mg) and [[Pyrimethamine]] (25 mg) indefinitely for patients with AIDS
| |
|
| |
| :*'''4. Cyclospora species'''
| |
| ::*Preferred regimen: [[TMP-SMZ]], 160 and 800 mg, respectively, qid for 10 days, followed by [[TMP-SMZ]] thrice weekly indefinitely
| |
|
| |
| :*'''5. Microsporidium species'''
| |
| ::*Preferred regimen: [[Albendazole]], 400 mg bid for 3 weeks; highly active antiretroviral therapy including a protease inhibitor is warranted for patients with AIDS
| |
|
| |
| :*'''6. Entamoeba histolytica'''
| |
| ::*Preferred regimen: [[Metronidazole]], 750 mg tid for 5 to 10 days, plus either [[Diiodohydroxyquinoline|Diiodohydroxyquin]], 650 mg tid for 20 days, or [[Paromomycin]], 500 mg tid for 7 days
| |
|
| |
| ===Contraindicated medications===
| |
| {{MedCondContrAbs
| |
|
| |
| |MedCond =Diarrhea|Ethacrynic acid}}
| |
|
| |
|
| ==References== | | ==References== |
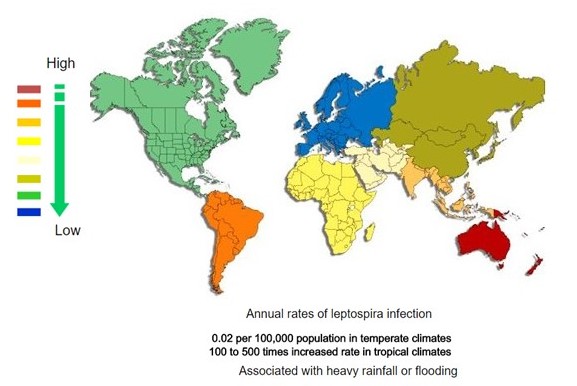 </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
![Histopathology of a pancreatic endocrine tumor (insulinoma). Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/2/2f/Pancreatic_insulinoma_histology_2.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Chromogranin A immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/a/a3/Pancreatic_insulinoma_histopathology_3.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Insulin immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/d/d5/Pancreatic_insulinoma_histology_4.JPG)