|
|
| (2 intermediate revisions by one other user not shown) |
| Line 1: |
Line 1: |
| * One fifth of the Americans with CAD have CTO (chronic total occlusion).
| |
| * CTO lesions are commonly ischemic, and studies have shown that despite collateral circulation, normal coronary flow reserve is found in less than 10% of patients. The presence of CTO has been associated with worse cardiovascular outcomes and death in select patient populations.
| |
| * Despite the presence of symptoms and objective evidence of ischemia or viability in the CTO myocardial territory, revascularization rates for such patients remain low.
| |
| * Here we will briefly review the improvements in current techniques, cardiovascular outcomes associated with successful CTO percutaneous coronary intervention (PCI), and discuss the current guidelines and appropriate use criteria for CTO PCI in stable ischemic heart disease (SIHD).
| |
| Current Progress
| |
|
| |
| Historically, CTO PCI attempt rates have been low and vary considerably among centers. In fact, the presence of a CTO is one of the most common reasons for referral for coronary artery bypass grafting. Similarly, those patients who are not candidates for surgery, or choose not to have surgery, are frequently not offered percutaneous revascularization and treated with only medical therapy. CTO findings in the SYNTAX (Synergy Between Percutaneous Coronary Intervention With TAXUS and Cardiac Surgery) trial was the most common reason for incomplete revascularization. The low rates of CTO PCI stem from the historic low success rates and potential for increased complications. Over the past decade, however, there has been a significant improvement in the technologies available for CTO PCI as well as the international dissemination of advanced CTO PCI techniques and skill sets. Technological advancements have included the development of specific CTO wires including soft tip wires to facilitate retrograde wiring, penetration wires to facilitate puncture of the proximal and distal caps as well as to facilitate re-entry from the subintimal space. Dedicated microcatheters for collateral channel dilatation as well as dedicated re-entry systems have been similarly developed to facilitate the success of both retrograde and dissection and re-entry techniques.7-8 The most important measure to improve success rates of CTO PCI came from the development of the hybrid algorithm for CTO PCI, which created a procedure plan for each CTO based on four anatomic variables:
| |
|
| |
| The ambiguity of the proximal occlusion cap
| |
| The quality of the distal coronary segment after the CTO
| |
| The operator ability to cross the collaterals
| |
| The length of the occlusion segment9
| |
| The hybrid algorithm for CTO PCI combines all available crossing techniques (antegrade wire escalation, antegrade dissection and re-entry, and retrograde approaches) to optimize procedural efficacy, efficiency, and safety.9 The hybrid algorithm also emphasizes adopting the following three principles:
| |
|
| |
| Clinical indication drives the decision for CTO PCI attempt.
| |
| Lesion characteristics decide the initial procedure approach.
| |
| The provision of an "exit failure mode" aims to increase procedure efficiency by decreasing the amount of time trying a single approach.
| |
| The hybrid algorithm and the three principles culminated in the improved success rates, procedure efficiency, and safety of present day CTO PCI. The OPEN CTO (Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion) study, the most contemporary CTO PCI registry available to date, reveals current trends in modern day CTO PCI, including a technical success rate of 86% (using core laboratory adjudication) with an associated risk of major adverse cardiac and cerebrovascular events (MACCE) of 7% and 0.9% risk of death.10
| |
|
| |
| Cardiovascular Outcomes
| |
|
| |
| Successful CTO PCI has been associated with numerous cardiovascular benefits, including improvement in left ventricular ejection fraction (LVEF), improved wall motion of the affected segment, and reduction in arrhythmic vulnerability.11-16 Quality-of-life variables have also been shown to improve after successful CTO PCI, including improvements in angina, heart failure symptoms, physical activity, and overall treatment satisfaction.10,17-18 Most importantly, successful CTO PCI has been associated with a reduction in all-cause mortality in registry data and met-analysis.19-20 Goa et al. published a meta-analysis of 5,958 patients who had undergone successful CTO PCI and compared them with 1,511 patients who had undergone unsuccessful CTO PCI.21 They found that successful CTO PCI using drug-eluting stents was associated with lower long-term mortality, lower risk of myocardial infarction, and lower risk of MACCE. Similarly, CTO PCI allows for complete revascularization, which has been associated with lower long-term mortality, lower rates of myocardial infarction, and lower rates of repeat revascularization, independent of the initial revascularization strategy. A post-hoc analysis of the 4-year outcomes of the SYNTAX trial showed the presence of CTO as the strongest predictor of incomplete revascularization after PCI, and incomplete revascularization was associated with higher adverse events, including increased mortality.22
| |
|
| |
| There have been 3 randomized control trials to date evaluating CTO PCI outcomes. The EXPLORE (Evaluating Xience and Left Ventricular Function in PCI on Occlusions After STEMI) trial included 304 patients with ST-segment elevation myocardial infarction who had a non-culprit CTO diagnosed at the time of their ST-segment elevation myocardial infarctions.23 Patients were assigned to CTO PCI within 1 week of the initial event versus medical therapy. The investigator found that CTO PCI was feasible and safe; however, it did not provide any overall benefit in LVEF or left ventricular end diastolic volume. Interestingly, the subgroup of patients who underwent CTO PCI of the left anterior descending artery, who likely had the largest amount of myocardium at risk, did improve their LVEF (47.2 vs. 40.4%, p = 0.02). The DECISION-CTO (Optimal Medical Therapy With or Without Stenting For Coronary Chronic Total Occlusion) trial, which was terminated early due to slow enrollment, randomized 417 patients to optimal medical therapy and CTO PCI and 398 patients to optimal medical therapy alone. There were no differences in the primary outcome of mortality at 3 years or secondary outcomes, including repeat revascularization, mortality at 5 years, or quality of life. In addition to early termination, there were several limitations to the DECISION-CTO trial design, including the lack of assessment of symptoms once non-CTO lesions were revascularized and the lack of assessment for ischemia and viability in the myocardial territories supplied by the CTO. Interestingly, the per-protocol and as-treated analysis revealed a trend toward better outcome with CTO PCI versus optimal medical therapy. The trial has yet to be peer-reviewed and published. Lastly, EURO-CTO (A Randomized Multicentre Trial to Evaluate the Utilization of Revascularization or Optimal Medical Therapy for the Treatment of Chronic Total Occlusions), which was also terminated early secondary to slow enrollment, randomized 407 patients with CTO in a 2:1 fashion to either optimal medical therapy and CTO PCI or optimal medical therapy alone. The investigators found that patients who received CTO PCI had significant improvement in angina frequency when compared with optimal medical therapy (p = 0.009) and improvement in their Canadian Cardiovascular Society Angina scores (p < 0.001). There were similar MACCE rates at 12 months between the 2 arms.
| |
|
| |
| Two out of the three randomized trials of CTO PCI were terminated early and did not meet their target enrollment numbers secondary to slow enrollment, which indicates the potential of significant selection bias. Patients who were enrolled are likely to have fewer symptoms and lower risk ischemia.
| |
|
| |
| Clinical trials comparing optimal medical therapy and CTO PCI versus optimal medical therapy alone are therefore still needed. Investigators performing such trials face significant difficulties, including high cost to conduct randomized control trials, barriers to randomize patients who are highly symptomatic, and the relative few number of centers with high CTO PCI success rates to avoid bias against CTO PCI in an intention-to-treat analysis.
| |
|
| |
| Guidelines
| |
|
| |
| The 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention recommended CTO PCI in patients with clinical indications and suitable anatomy when performed by operators with appropriate expertise (Class IIa, Level of Evidence [LOE] B).24
| |
|
| |
| The 2014 European Society of Cardiology and European Association for Cardio-Thoracic Surgery guidelines on myocardial revascularization recommend CTO PCI to be considered in patients with expected ischemia reduction in a corresponding myocardial territory and/or angina relief (Class IIa, LOE B). They recommend an initial anterograde approach and consideration of a retrograde approach if this fails or a primary retrograde approach in selected patients (Class IIb, LOE C).25
| |
|
| |
| The ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 Appropriate Use Criteria for Coronary Revascularization in Patients With Stable Ischemic Heart Disease have eliminated the separate criteria for CTO lesions as was the case in the 2012 guidelines. Currently, indications for revascularization in SIHD are determined irrespective of whether the lesion is a CTO.26 The indication for revascularization of a coronary artery lesion, whether CTO or severe stenosis, is based on symptoms, the extent of antianginal medications, and the risk of ischemia.
| |
|
| |
| Conclusions
| |
|
| |
| As adoption of CTO PCI becomes more common and as evidence of cardiovascular benefits continues to evolve, guidelines have favorably acknowledged the appropriateness of CTO PCI. Currently, due to the lack of evidence from randomized control trials, routine use of CTO PCI is not recommended. Patients who have symptoms of ischemia despite optimal medical therapy, those with moderate to large areas of myocardium at jeopardy, and patients with ischemic cardiomyopathies with viable myocardium are likely to gain the most benefit from CTO PCI. CTO PCI should be performed by operators who are well versed in CTO PCI techniques and management of associated complications. Most importantly, informed discussions with patients and providers emphasizing the risk and benefits associated with CTO PCI for a given patient's condition are the keys to providing patients with appropriate CTO PCI.
| |
|
| |
|
| |
|
| |
| ==Physical examination== | | ==Physical examination== |
| ==References== | | ==References== |
| Line 48: |
Line 5: |
| {{WH}} | | {{WH}} |
| {{WS}} | | {{WS}} |
|
| |
| [[Category:Primary care]]
| |
| [[Category:Gastroenterology]]
| |
|
| |
| [[Category:Needs overview]]
| |
|
| |
|
| ==References== | | ==References== |
| Line 94: |
Line 46: |
| {{WH}} | | {{WH}} |
| {{WS}} | | {{WS}} |
|
| |
| [[Category:Primary care]]
| |
| [[Category:Gastroenterology]]
| |
|
| |
| [[Category:Needs overview]]
| |
|
| |
|
| ==Other Imaging Findings== | | ==Other Imaging Findings== |
| Line 122: |
Line 69: |
| {{WH}} | | {{WH}} |
| {{WS}} | | {{WS}} |
|
| |
| [[Category:Primary care]]
| |
| [[Category:Gastroenterology]]
| |
|
| |
| [[Category:Needs overview]]
| |
|
| |
|
| ===Pathophysiology prev=== | | ===Pathophysiology prev=== |
| Line 177: |
Line 119: |
| ===Image and text to the right=== | | ===Image and text to the right=== |
|
| |
|
| <figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>[[File:Global distribution of leptospirosis.jpg|577x577px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017. | | <figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>[[File:Global distribution of leptospirosis.jpg|577x577px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017. |
|
| |
|
| ===Gallery=== | | ===Gallery=== |
| Line 192: |
Line 134: |
| ==References== | | ==References== |
| {{Reflist|2}} | | {{Reflist|2}} |
|
| |
| [[Category:Gastroenterology]]
| |
| [[Category:Hepatology]]
| |
| [[Category:Disease]]
| |
|
| |
| {{WS}} | | {{WS}} |
| {{WH}} | | {{WH}} |
| Line 203: |
Line 140: |
| REFERENCES | | REFERENCES |
| <references /> | | <references /> |
| | |
| | [[Category:Gastroenterology]] |
| | [[Category:Needs overview]] |
| | [[Category:Hepatology]] |
| | [[Category:Disease]] |
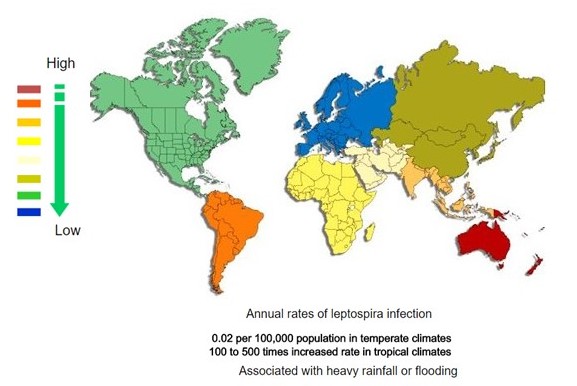 </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
![Histopathology of a pancreatic endocrine tumor (insulinoma). Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/2/2f/Pancreatic_insulinoma_histology_2.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Chromogranin A immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/a/a3/Pancreatic_insulinoma_histopathology_3.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Insulin immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/d/d5/Pancreatic_insulinoma_histology_4.JPG)