SLAP tear
| SLAP tear | |
 | |
|---|---|
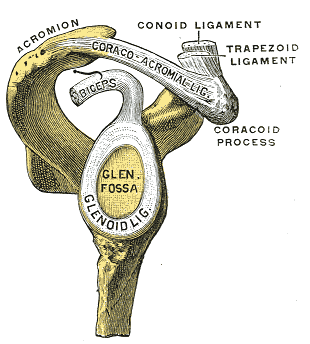
| Glenoid fossa of right side. (Glenoidal labrum labeled as "glenoid lig.") | |
| ICD-9 | 840.7 |
A SLAP (Superior Labrum from Anterior to Posterior) tear or lesion is an injury to the Glenoid labrum, a part of the shoulder joint.
Overview
The shoulder joint is considered a 'ball and socket' joint. However, in bony terms the 'socket' (the glenoid fossa of the scapula) is quite small, covering at most only a third of the 'ball' (the head of the humerus). The socket is somewhat deepened by a circumferential rim of fibrocartilage which is called the glenoidal labrum. Previously there was some argument as to the structure (it is fibrocartilaginous as opposed to the hyaline cartilage found in the remainder of the glenoid fossa) and function (whilst it has previously been considered a redundant evolutionary remnant, it is now considered an integral structure in the shoulder's stability). Currently most authorities agree that the tendon of the long head of the biceps brachii muscle proximally becomes fibrocartilaginous prior to attaching to the superior aspect of the glenoid, and in a similar arrangement the long head of the triceps brachii inserts inferiorly.[1] Together these cartilaginous extensions of the tendon are termed the 'glenoid labrum'. A SLAP (Superior Labrum from Anterior to Posterior) tear or lesion occurs when there is damage to the superior or uppermost area of the labrum. SLAP lesions have come into public awareness with their increasing frequency in overhead and particularly throwing athletes. The increased frequency relates to the relatively recent description of labral injuries in throwing athletes [2] and the initial definitions of the 4 SLAP sub-types[3] all happening in the last 20 years or so. The identification and treatment of these injuries continues to evolve today, however it is safe to say that a baseball pitcher suffering a 'dead arm' caused by a SLAP lesion today is far more likely to recover such that he can return to the game at its highest level than was the case 20 or 30 years ago.
Sub-types
At least ten types of this injury are recognized with varying degrees of damage,[4] seven of which are listed here
- Degenerative fraying of the superior portion of the labrum, with the labrum remaining firmly attached to the glenoid rim
- Separation of the superior portion of the glenoid labrum and tendon of the biceps brachii muscle from the glenoid rim
- Bucket-handle tears of the superior portion of the labrum without involvement of the biceps brachii (long head) attachment
- Bucket-handle tears of the superior portion of the labrum extending into the biceps tendon
- Anteroinferior Bankart lesion that extends upward to include a separation of the biceps tendon
- Unstable radial of flap tears associated with separation of the biceps anchor
- Anterior extension of the SLAP lesion beneath the middle glenohumeral ligament
Symptoms
There are several symptoms that are common with this type of injury
- A dull throbbing ache in the joint. This can be brought on by very strenuous exertion or simple household chores. Sufferers notice that they turn to ice packs more frequently for relief.
- Difficulty sleeping due to shoulder discomfort. The SLAP lesion decreases the stability of the joint which when combined with lying in bed causes the shoulder to drop. This in turn pulls on the muscles and ligaments causing discomfort.
- For an athlete involved in a throwing sport such as baseball, pain and a catching feeling are prevalent.
- Any applied force overhead or pushing directly into the shoulder can result in impingement and catching sensations.
Treatment
Very few patients with SLAP lesion injuries return to full capability without surgical intervention. Very rarely physical therapy can strengthen the supporting muscles in the shoulder joint to the point of reestablishing stability. For all other cases the choice is do nothing or have surgery to reattach the labrum to the glenoid.
While the surgery can be performed as a traditional open procedure, the recommended course of action is an arthroscopic surgery. This type of procedure is vastly less intrusive to the body and reduces chances of infection.
During the procedure the surgeon should check the general health of the shoulder joint. There are at least twenty different items of conditions that he/she should examine or look for. These include:
- SLAP lesion – labrum/glenoid separation at the tendon of the biceps muscle
- Bankart lesion – labrum/glenoid separation at the inferior glenohumeral ligament
- Biceps Tendon
- Bone – glenoid, humerus - general surface condition
- Ligaments – check for tears and condition
Procedure
The basic procedure is as follows.
Following inspection and determination of the extent of the injury the basic labrum repair, be it SLAP or Bankart lesion is as follows.
The glenoid and labrum are roughened to increase contact surface area and promote re-growth.
Locations for the bone anchors are selected based on number and severity of tear. A really bad tear involving SLAP and Bankart lesions may require seven anchors. Simple tears may only require one.
The glenoid is drilled for the anchor implantation.
The anchors are inserted in the glenoid.
The suture component of the implant is tied through the labrum and knotted such that the labrum is in tight contact with the glenoid surface.
Surgical Recovery
Stage one – For the first four weeks the arm is typically kept in a sling. Some surgeons only have the patient in a sling for a week. Patients may find themselves in an immobilizer sling, which adds a waist support to prevent movement. Needless to say, the first stage of recovery is about not stressing the repair site. This is the initial healing phase of the recovery.
Stage two – Initial physical therapy. The goal here is to increase range of motion. Load bearing through the joint should be avoided to allow the repair to complete.
Stage three – Increased range of motion and initial strength training. At this point, about eight to ten weeks out, the repair should be complete but not ready for full loading yet. Return to day-to-day activities, but not strenuous activity.
Stage four – completion. At about six months out the repair should be strong enough for a return to full activity.
Note that this timeline will vary according to surgeon preferences and the extent of damage.
References
- ↑ Huber, W.P. and R.V. Putz, Periarticular fiber system of the shoulder joint. Arthroscopy, 1997. 13(6): p. 680-91.
- ↑ Andrews, J.R., E.G. Carson, and W.D. McLeod, Glenoid labrum tears related to the long head of the biceps. American journal of sports medicine, 1985. 13(5): p. 337-341.
- ↑ Snyder, S.J., et al., SLAP lesions of the shoulder. Arthroscopy, 1990. 6(4): p. 274-9.
- ↑ Mohana-Borges, A.V., C.B. Chung, and D. Resnick, Superior labral anteroposterior tear: classification and diagnosis on MRI and MR arthrography. AJR Am J Roentgenol, 2003. 181(6): p. 1449-62.
External links
- slaptear.com FAQs, Blogs, and discussion about slap tear injuries
- Radiographics search on Superior Labrum