Right ventricular myocardial infarction
| Myocardial infarction | |
| ICD-10 | I21-I22 |
|---|---|
| ICD-9 | 410 |
| DiseasesDB | 8664 |
| MedlinePlus | 000195 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Acute myocardial infarction involving only the free wall of the right ventricle is a rare event [1] More commonly, right ventricular infarction is associated with infarction of the inferior wall of the left ventricle, occurring in more than one-third of such cases [2] [3] [4] [5] [6] [7] [8] [9] [10], even when thrombolytic therapy is given [11].
One study of 113 patients with a first acute inferior wall infarction reported that the presence of preinfarction angina within 72 hours of the infarction was associated with a reduction in the incidence of right ventricular infarction (odds ratio 0.2) and combined hypotension and shock (odds ratio 0.1) [12]. This is possibly the result of ischemic preconditioning.
- Ninety percent of right ventricular infarcts result from occlusion of the proximal right coronary artery, while another 5 to 10 percent arise after occlusion of the left anterior descending artery [13] [14] [15] [16]
Although more than one-third of cases are clinically silent [17], the presence of right ventricular infarction often has important implications for both management and prognosis.
Differential diagnosis of conditions to distinguish from right ventricular infarction
- Acute pericarditis
- Pneumothorax
- Pulmonary Embolism
- Hypertrophic Cardiomyopathy
- Restrictive cardiomyopathy
- Tricuspid Regurgitation
- Cor Pulmonale
- Constrictive pericarditis
- Endomyocardial fibrosis
- Primary pulmonary hypertension
- Secondary pulmonary hypertension
Diagnosis
- Because the right ventricle has a remarkable tendency to recover function rapidly, diagnostic tests are most reliable when performed soon after presentation. Clinical suspicion and a careful physical examination demonstrating the signs are the first step.
In general, requirements of diagnosing a right ventricular myocardial infarction as follow:
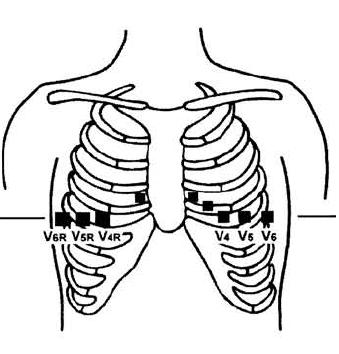
- Right-sided ST segment elevation of > 1 mm (leads V3R through V6R)
- Right ventricular asynergy as demonstrated by echocardiography or cardiac nuclear imaging
- Mean right arterial pressure of ≥ 10 mm Hg or a < 5 mm Hg difference from mean pulmonary capillary wedge pressure (equivalent to left atrial pressure)
- Non-compliant right atrial pressure waveform pattern (steep and deep x and y descents)
History and Symptoms
- Ischemia or infarction of the right ventricle results in decreased right ventricular compliance, reduced filling, and diminished right-sided stroke volume with concomitant right venticular dilation and alteration in septal curvature [18] These hemodynamic and geometric changes lead to decreased left ventricular filling and contractile function with a concomitant fall in cardiac output [19] [20] [21] [22] [23] [24]. The net effect is that left-sided filling pressures may be below normal despite clinical signs of high pressure on the right side. This disparity has important implications for therapy (see below).
- Patients with hemodynamically significant right ventricular infarction typically present with hypotension, jugular vein distention, and occasionally shock, all in the presence of clear lung fields. Valvular insufficiency can also occur, leading to tricuspid regurgitation. These findings are in contrast to the frequent pulmonary congestion, third or fourth heart sounds, and mitral regurgitation with left ventricular infarcts.
Laboratory Studies
- The diagnosis of right ventricular infarction is suspected in the appropriate clinical setting when the right atrial pressure exceeds 10 mmHg and the ratio of right atrial pressure to pulmonary capillary wedge pressure exceeds 0.8 (normal mean value less than 0.6)[25] [26] [27] [28] [29].
However, these findings may not be present in patients with only minimal right ventricular dysfunction or in those with intravascular volume depletion. In the latter setting, a volume challenge may unmask the signs of right ventricular infarction [30]
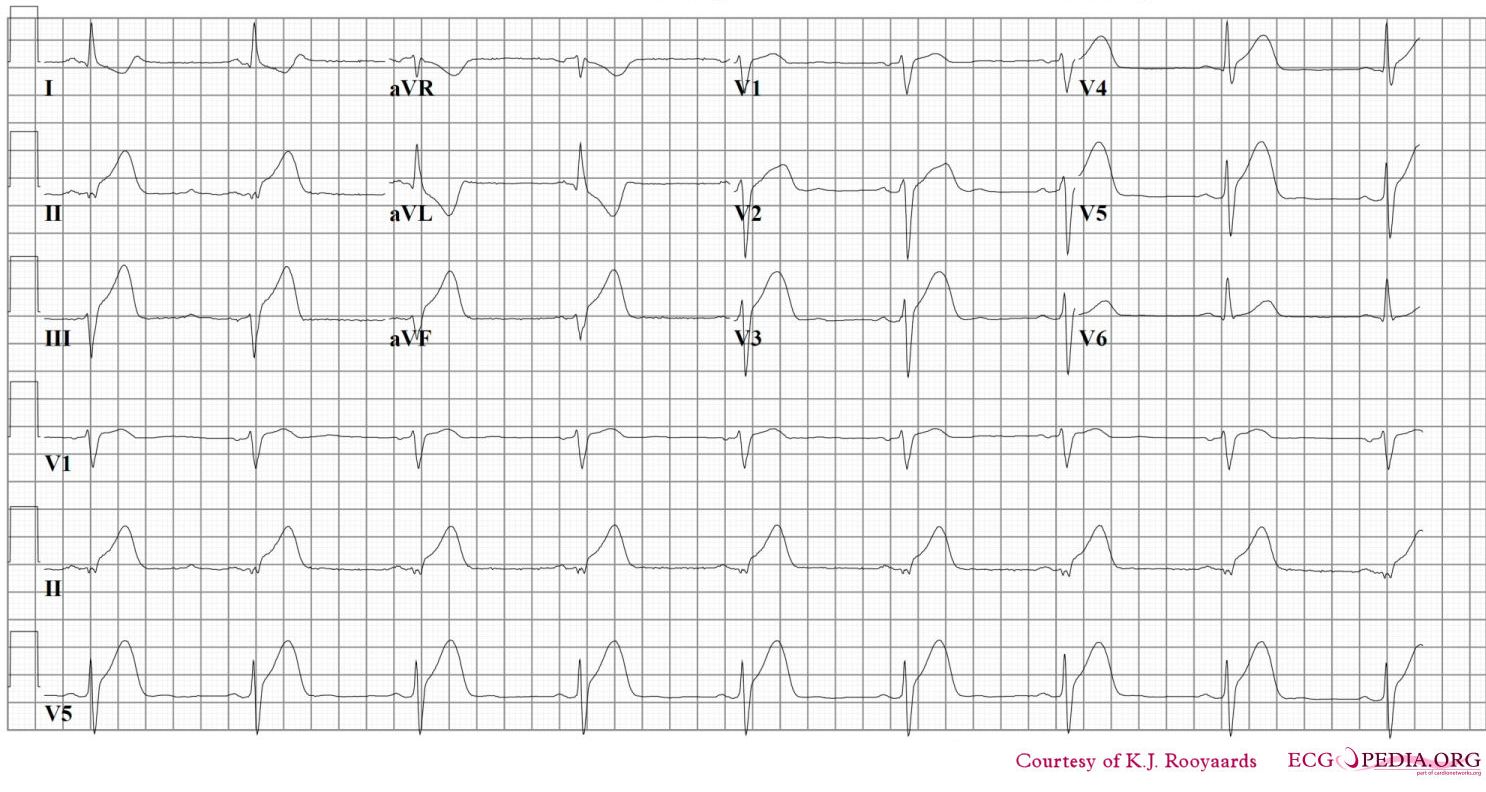
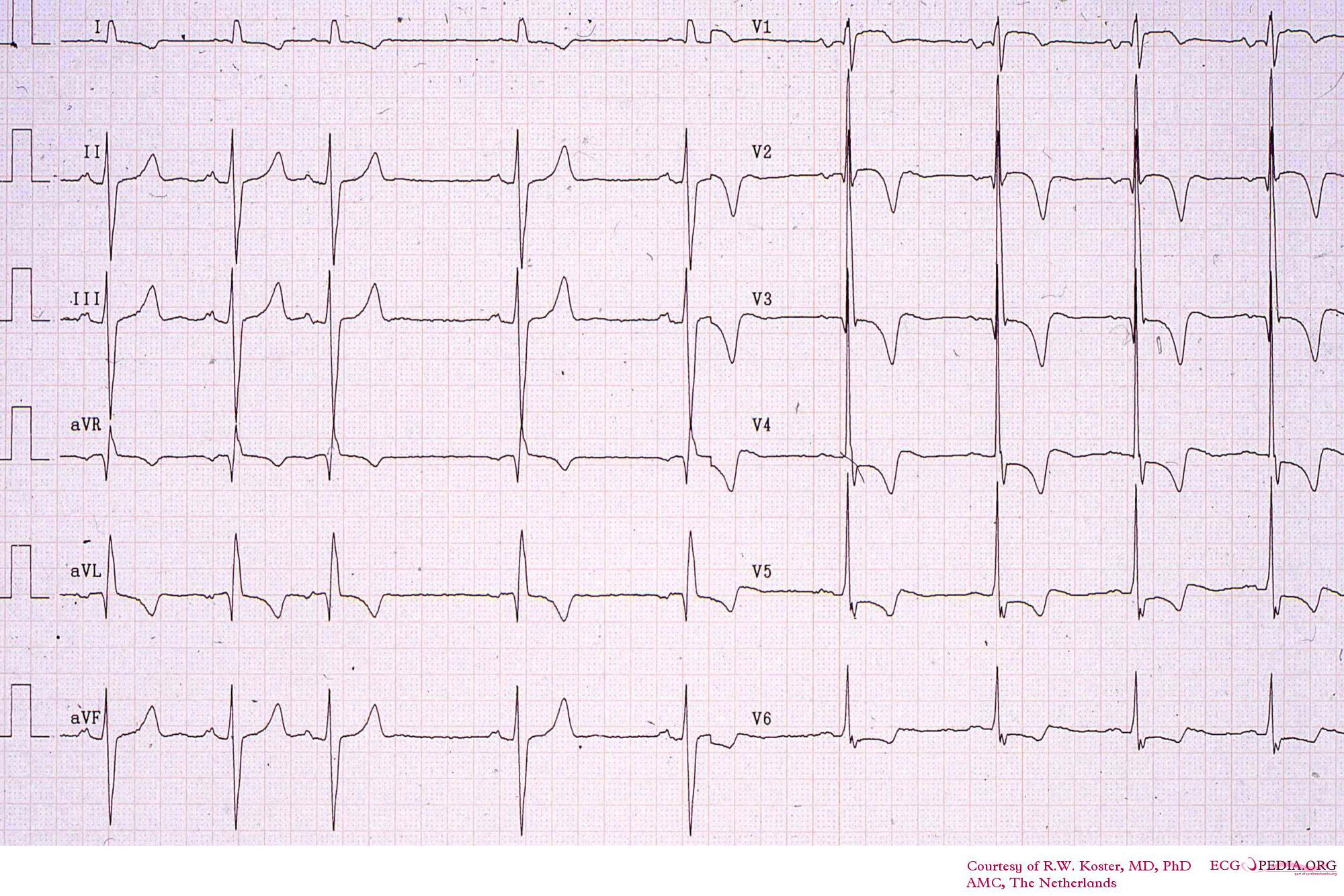
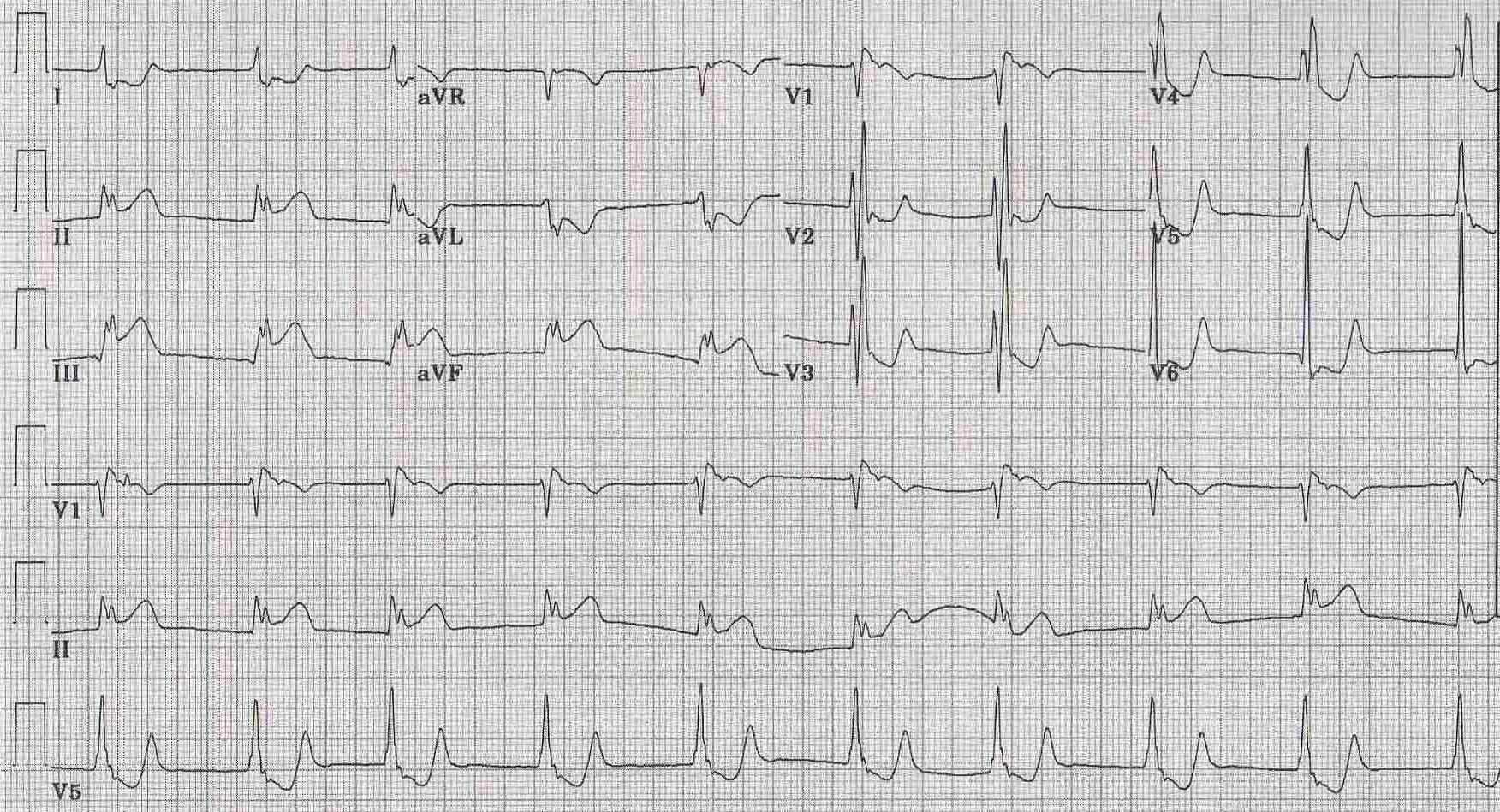
Electrocardiogram
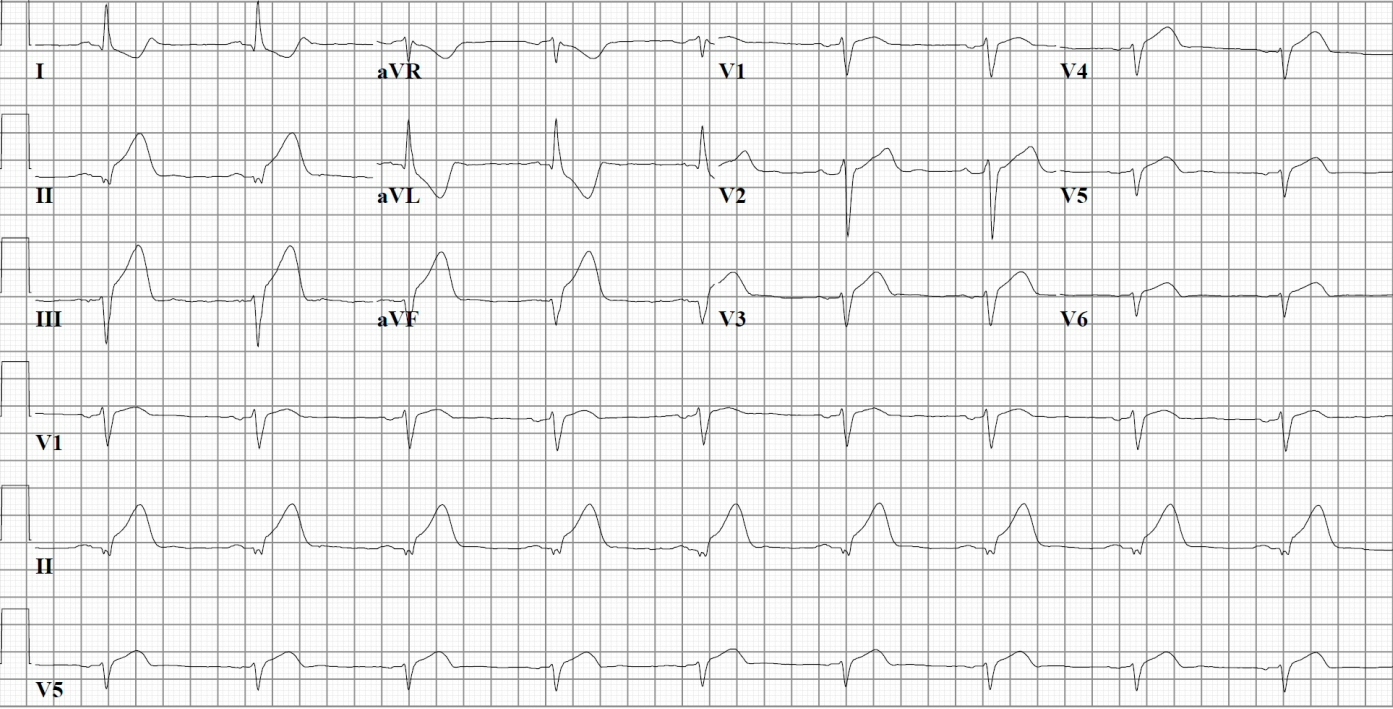
- In addition to evidence of an acute inferior or inferoposterior myocardial infarction, the ECG may demonstrate > or =1 mm of doming ST elevation in the right sided precordial leads V4R to V6R. Right sided ST elevation, particularly in V4R, is indicative of acute right ventricular injury [31] [32] [33] and correlates closely with occlusion of the proximal right coronary artery. In one report of patients with acute inferior infarction, for example, ST elevation in V4R had 88 percent sensitivity and 78 percent specificity for concurrent right ventricular infarction [34]
Pulmonary embolism, pericarditis, and |anteroseptal myocardial infarction also cause elevation of the ST segment in the right-sided precordial leads. As a result, an electrocardiographic diagnosis of right ventricular infarction cannot be made when one of these conditions is present [35] [36]
-
12 lead ECG shows Inferior MI + Right ventricular MI
-
ST elevation at V4R on same patient's EKG (obtained from right precordial leads).
Echocardiography
- Echocardiography may be limited in right ventricular infarction by suboptimal views of the right ventricle. In addition, interpretation of right ventricular function may be affected by coexistent pulmonary disease (such as obstructive lung disease or pulmonary embolism).
- Despite these limitations, echocardiography is often a useful test that can be performed at the bedside when the diagnosis of right ventricular infarction is suspected. Right ventricular size and function and the degree (if any) of tricuspid insufficiency can all be evaluated [37] Useful information concerning left-sided structures and function can also be obtained [38][39]
- Right ventricular peak systolic pressure may be estimated from the Doppler signal of tricuspid insufficiency using the modified Bernoulli equation:
- Right ventricular peak systolic pressure = RAP + 4V(2)
- Where RAP equals the estimated right atrial pressure based upon examination of the jugular neck veins, V is the velocity of the tricuspid insufficiency jet by Doppler ultrasonography, and V(2) refers to V squared. A right ventricular peak systolic pressure above 30 mmHg is considered elevated. Mild elevation is 30 to 45 mmHg, moderate 45 to 60 mmHg, and severe is greater than 60 mmHg.
- Right ventricular peak systolic pressure = RAP + 4V(2)
- In the absence of pulmonary stenosis (which is rare), right ventricular systolic pressure is equal to the pulmonary artery systolic pressure. As a result, this equation is useful for estimating the presence and severity of pulmonary hypertension. When significant pulmonary artery hypertension (>45 to 50 mmHg) complicates right ventricular infarction, the failing right ventricle may be unable to pump blood from the right heart into the left heart. In this setting, a positive inotropic agent such as dobutamine may be effective in augmenting forward flow while also decreasing pulmonary vascular resistance and right ventricular overload (see below)
Other Imaging Findings
- Radionuclide ventriculography and technetium-99m-pyrophosphate scanning
- These techniques have acceptable sensitivities and specificities for making a diagnosis of right ventricular infarction [40] [41] [42] [43] Radionuclide angiography can detect wall motion abnormalities and hypoperfusion in the affected right ventricle. It can also be used to quantitate both left and right ventricular ejection fractions. Technetium scanning, on the other hand, is particularly useful for late diagnosis, as it shows areas of necrotic or dying myocardium.
- However, both methods are cumbersome and time consuming. They are also frequently difficult to perform at the bedside, particularly when the patient is unstable in the intensive care unit and nuclear cardiology equipment is not readily portable. Thus, these tests are best performed later in the course to further quantify the degree of right ventricular infarction and dysfunction.
Risk Stratification
- The presence of right ventricular infarction adversely affects the early prognosis. One study, for example, evaluated 200 consecutive patients with acute inferior myocardial infarction [44] Those with ST elevation in V4R had an almost eight-fold increase in in-hospital mortality (31 versus 6 percent) and morbidity when compared to those without changes in V4R.
- Elderly patients who have right ventricular involvement with an inferior wall myocardial infarction are at particularly high risk. In a study of 198 patients ≥75 years of age, right ventricular involvement was associated with an in-hospital mortality of 47 percent compared to a 10 percent mortality in the absence of right ventricular involvement [45]
- For patients who survive an acute right ventricular infarction, however, the prognosis is generally good. As an example, among 522 patients with an inferior wall infarction who were treated with a thrombolytic agent and hirudin or heparin in the HIT-4 study, 32 percent had right ventricular involvement and these patients had a higher 30 day mortality when compared to those without right ventricular involvement (5.9 versus 2.5 percent) [46] However, this was related to a larger infarct size rather than right ventricular involvement; right ventricular involvement was not an independent predictor of survival.
- The right ventricle frequently recovers the majority of its function, probably due at least in part to decreased oxygen demand of the thin-walled right ventricle [47] [48]. These patients may, however, have a more frequent requirement for a permanent pacemaker. [49]
Treatment
- Therapy in symptomatic patients is aimed at reversing the decreased filling and right-sided stroke volume and at improving right ventricular function.
- Aggressive fluid resuscitation
- Intravenous fluid, usually isotonic saline, should be given to raise the central filling pressure in an attempt to maximize forward flow out of the right ventricle, thereby preventing inappropriate low left-sided filling pressures [50] [51] In most cases, several liters of saline are infused rapidly until there is an increase in the pulmonary capillary wedge pressure to approximately 15 mmHg. If central hemodynamic monitoring in not available, one to two liters of saline can be infused while closely following the blood pressure and urine output and examining the patient for signs of pulmonary congestion.
- Avoid drugs which decrease preload
- Systemic cardiac output is dependent upon filling of the left ventricle. In the setting of right ventricular dysfunction and decreased contractility, reduced preload results sequentially in diminished right sided stroke volume, reduced flow to the left heart, and a fall in cardiac output. As a result, any medication (such as diuretics or nitrates) or maneuver which decreases preload should be avoided. Even an increase in vagal tone caused by insertion of a bladder catheter can acutely decrease preload and lead to cardiogenic shock.
- Inotropic stimulation
- When fluid resuscitation is insufficient, inotropic and chronotropic stimulation with dobutamine may increase forward flow and augment cardiac output. Dobutamine may also act by reducing pulmonary vascular resistance and therefore right ventricular afterload. The usual starting dose is 5 µg/kg per min. The dose is titrated up to 20 µg/kg per min depending upon the clinical response. However, frequent ventricular ectopy and ventricular tachycardia may limit the use of doses above 10 µg/kg per min. Additionally, since dobutamine decreases peripheral vascular resistance, higher doses may cause hypotension as a result of an inadequate rise in cardiac output to match the decrease in systemic vascular resistance.
- Pacing
- Right ventricular pacing may be necessary if the infarction results in complete heart block or loss of AV synchrony.
- Reperfusion
- Early reperfusion using either thrombolytic therapy or direct angioplasty is useful for preserving both right and left ventricular function and results in decreased mortality and morbidity [52] [53] [54] [55]
The indications for these modalities are similar to those in left ventricular infarction. Patients in whom reperfusion is achieved typically show a dramatic improvement in the hemodynamic profile within 24 hours [56] [57]
- As an example, one study of 53 patients reported that primary angioplasty resulted in normal flow in the right coronary artery and its major right ventricular branches in 77 percent of patients; reperfusion was associated with prompt and striking recovery of right ventricular function at three days [58] Failure to reperfuse resulted in lack of functional recovery, persistent hypotension, low cardiac output, and a higher mortality rate (58 versus 2 percent for those with successful reperfusion, p=0.001).
References
- ↑ Anderson, HR, Falk, E, Nielsen, D. Right ventricular infarction: Frequency, size, and topography in coronary heart disease. J Am Coll Cardiol 1987; 10:1223. PMID 3680789
- ↑ Anderson, HR, Falk, E, Nielsen, D. Right ventricular infarction: Frequency, size, and topography in coronary heart disease. J Am Coll Cardiol 1987; 10:1223. PMID 3680789
- ↑ Isner, JM, Roberts, WC. Right ventricular infarction complicating left ventricular infarction secondary to coronary artery disease: frequency, location, associated findings and significance from analysis of 236 necropsy patients with acute or healed myocardial infarction. Am J Cardiol 1978; 42:885. PMID 153103
- ↑ Isner, JM. Right ventricular myocardial infarction. JAMA 1988; 259:712. PMID 3275819
- ↑ Williams, JF. Right ventricular infarction. Clin Cardiol 1990; 13:309. PMID 2189611
- ↑ Cabin, HS, Clubb, S, Wackers FJ, et al. Right ventricular myocardial infarction with anterior wall left ventricular infarction: an autopsy study. Am Heart J 1987; 113:16. PMID 3799430
- ↑ Kinch, JW, Ryan, TJ. Right ventricular infarction. N Engl J Med 1994; 330:1211. PMID 8139631
- ↑ Setaro, JF, Cabin, HS. Right ventricular infarction. Cardiol Clin 1992; 10:69. PMID 1739961
- ↑ Cohn, JN. Right ventricular infarction revisited. Am J Cardiol 1979; 43:666. PMID 420117
- ↑ Wackers, FJ, Lie, KI, Sokole, EB, et al. Prevalence of right ventricular involvement in inferior wall infarction associated with myocardial imaging with thallium-201 and technetium-99m pyrophosphate. Am J Cardiol 1978; 42:358. PMID 210648
- ↑ Zeymer, U, Neuhaus, K-L, Wegscheider, K, et al. Effects of thrombolytic therapy in acute inferior myocardial infarction with and without right ventricular involvement. J Am Coll Cardiol 1998; 32:876. PMID 9768705
- ↑ Shiraki, H, Yoshikawa, T, Anzai, T, et al. Association between preinfarction angina and a lower risk of right ventricular infarction. N Engl J Med 1998; 338:941. PMID 9521981
- ↑ Isner, JM, Roberts, WC. Right ventricular infarction complicating left ventricular infarction secondary to coronary artery disease: frequency, location, associated findings and significance from analysis of 236 necropsy patients with acute or healed myocardial infarction. Am J Cardiol 1978; 42:885.PMID 153103
- ↑ Isner, JM. Right ventricular myocardial infarction. JAMA 1988; 259:712. PMID 3275819
- ↑ Williams, JF. Right ventricular infarction. Clin Cardiol 1990; 13:309. PMID 2189611
- ↑ Cabin, HS, Clubb, S, Wackers FJ, et al. Right ventricular myocardial infarction with anterior wall left ventricular infarction: an autopsy study. Am Heart J 1987; 113:16. PMID 3799430
- ↑ Wackers, FJ, Lie, KI, Sokole, EB, et al. Prevalence of right ventricular involvement in inferior wall infarction associated with myocardial imaging with thallium-201 and technetium-99m pyrophosphate. Am J Cardiol 1978; 42:358. PMID 210648
- ↑ Brookes, C, Ravn, H, White, P, et al. Acute right ventricular dilatation in response to ischemia significantly impairs left ventricular systolic performance. Circulation 1999; 100:761. PMID 10449700.
- ↑ Williams, JF. Right ventricular infarction. Clin Cardiol 1990; 13:309. PMID 2189611
- ↑ Kinch, JW, Ryan, TJ. Right ventricular infarction. N Engl J Med 1994; 330:1211. PMID 8139631
- ↑ Setaro, JF, Cabin, HS. Right ventricular infarction. Cardiol Clin 1992; 10:69. PMID 1739961
- ↑ Cohn, JN. Right ventricular infarction revisited. Am J Cardiol 1979; 43:666. PMID 420117
- ↑ Zeymer, U, Neuhaus, K-L, Wegscheider, K, et al. Effects of thrombolytic therapy in acute inferior myocardial infarction with and without right ventricular involvement. J Am Coll Cardiol 1998; 32:876. PMID 9768705
- ↑ Shiraki, H, Yoshikawa, T, Anzai, T, et al. Association between preinfarction angina and a lower risk of right ventricular infarction. N Engl J Med 1998; 338:941. PMID 9521981
- ↑ Isner, JM. Right ventricular myocardial infarction. JAMA 1988; 259:712.PMID 3275819
- ↑ Williams, JF. Right ventricular infarction. Clin Cardiol 1990; 13:309. PMID 2189611
- ↑ Kinch, JW, Ryan, TJ. Right ventricular infarction. N Engl J Med 1994; 330:1211. PMID 8139631
- ↑ Cohn, JN. Right ventricular infarction revisited. Am J Cardiol 1979; 43:666. PMID 420117
- ↑ Dell'Italia, LJ, Starling, MR, Crawford, MH, et al. Right ventricular infarction: Identification by hemodynamic measurements before and after volume loading and correlation with noninvasive techniques. J Am Coll Cardiol 1984; 4:931. PMID 6092446
- ↑ Dell'Italia, LJ, Starling, MR, Crawford, MH, et al. Right ventricular infarction: Identification by hemodynamic measurements before and after volume loading and correlation with noninvasive techniques. J Am Coll Cardiol 1984; 4:931. PMID 6092446
- ↑ Isner, JM. Right ventricular myocardial infarction. JAMA 1988; 259:712. PMID 3275819
- ↑ Kinch, JW, Ryan, TJ. Right ventricular infarction. N Engl J Med 1994; 330:1211. PMID 8139631
- ↑ Zehender, M, Kasper, W, Kauder, E, et al. Right ventricular infarction as an independent predictor of prognosis after acute inferior myocardial infarction. N Engl J Med 1993; 328:981. PMID 8450875
- ↑ Zehender, M, Kasper, W, Kauder, E, et al. Right ventricular infarction as an independent predictor of prognosis after acute inferior myocardial infarction. N Engl J Med 1993; 328:981. PMID 8450875.
- ↑ Williams, JF. Right ventricular infarction. Clin Cardiol 1990; 13:309. PMID 2189611
- ↑ Kahn, JK, Bernstein, M, Bengston, JR. Isolated right ventricular myocardial infarction. Ann Intern Med 1993; 118:708. PMID 8460858
- ↑ Zehender, M, Kasper, W, Kauder, E, et al. Right ventricular infarction as an independent predictor of prognosis after acute inferior myocardial infarction. N Engl J Med 1993; 328:981. PMID 8450875
- ↑ Zehender, M, Kasper, W, Kauder, E, et al. Right ventricular infarction as an independent predictor of prognosis after acute inferior myocardial infarction. N Engl J Med 1993; 328:981. PMID 8450875
- ↑ Kahn, JK, Bernstein, M, Bengston, JR. Isolated right ventricular myocardial infarction. Ann Intern Med 1993; 118:708. PMID 8460858
- ↑ Kinch, JW, Ryan, TJ. Right ventricular infarction. N Engl J Med 1994; 330:1211. PMID 8139631
- ↑ Cohn, JN. Right ventricular infarction revisited. Am J Cardiol 1979; 43:666. PMID 420117
- ↑ Zehender, M, Kasper, W, Kauder, E, et al. Right ventricular infarction as an independent predictor of prognosis after acute inferior myocardial infarction. N Engl J Med 1993; 328:981. PMID 8450875
- ↑ Kahn, JK, Bernstein, M, Bengston, JR. Isolated right ventricular myocardial infarction. Ann Intern Med 1993; 118:708. PMID 8460858
- ↑ Zehender, M, Kasper, W, Kauder, E, et al. Right ventricular infarction as an independent predictor of prognosis after acute inferior myocardial infarction. N Engl J Med 1993; 328:981. PMID 8450875
- ↑ Bueno, H, Lopez-Palop, R, Bermejo, J, et al. In-hospital outcome of elderly patients with acute inferior myocardial infarction and right ventricular involvement. Circulation 1997; 96:436. PMID 9788824
- ↑ Zeymer, U, Neuhaus, K-L, Wegscheider, K, et al. Effects of thrombolytic therapy in acute inferior myocardial infarction with and without right ventricular involvement. J Am Coll Cardiol 1998; 32:876. PMID 9768705
- ↑ Williams, JF. Right ventricular infarction. Clin Cardiol 1990; 13:309. PMID 2189611
- ↑ Cohn, JN. Right ventricular infarction revisited. Am J Cardiol 1979; 43:666. PMID 420117
- ↑ Zehender, M, Kasper, W, Kauder, E, et al. Right ventricular infarction as an independent predictor of prognosis after acute inferior myocardial infarction. N Engl J Med 1993; 328:981. PMID 8450875
- ↑ Kinch, JW, Ryan, TJ. Right ventricular infarction. N Engl J Med 1994; 330:1211. PMID 8139631
- ↑ Dell'Italia, LJ, Starling, MR, Crawford, MH, et al. Right ventricular infarction: Identification by hemodynamic measurements before and after volume loading and correlation with noninvasive techniques. J Am Coll Cardiol 1984; 4:931. PMID 6092446
- ↑ Goldberger, JJ, Himelman, RB, Wolfe, CL, Schiller, NB. Right ventricular infarction: Recognition and assessment of its hemodynamic significance by two-dimensional echocardiography. J Am Soc Echocardiogr 1991; 4:140. PMID 2036226
- ↑ Berger, PB, Ruocco, NA, Ryan, TJ, et al. Frequency and significance of right ventricular dysfunction during inferior wall left ventricular myocardial infarction treated with thrombolytic therapy. Am J Cardiol 1993; 71:1148. PMID 8097614
- ↑ Kinn, JW, Aljuni, SC, Samyn, JG, et al. Rapid hemodynamic improvement after reperfusion during right ventricular infarction. J Am Coll Cardiol 1995; 26:1230. PMID 7594036
- ↑ Bowers, TR, O'Neill, WW, Grines, C, et al. Effect of reperfusion on biventricular function and survival after right ventricular infarction. N Engl J Med 1998; 338:933. PMID 9521980
- ↑ Kinn, JW, Aljuni, SC, Samyn, JG, et al. Rapid hemodynamic improvement after reperfusion during right ventricular infarction. J Am Coll Cardiol 1995; 26:1230. PMID 7594036
- ↑ Bowers, TR, O'Neill, WW, Grines, C, et al. Effect of reperfusion on biventricular function and survival after right ventricular infarction. N Engl J Med 1998; 338:933. PMID 9521980
- ↑ Bowers, TR, O'Neill, WW, Grines, C, et al. Effect of reperfusion on biventricular function and survival after right ventricular infarction. N Engl J Med 1998; 338:933. PMID 9521980
External links
- Risk Assessment Tool for Estimating Your 10-year Risk of Having a Heart Attack - based on information of the Framingham Heart Study, from the United States National Heart, Lung and Blood Institute
- Heart Attack - overview of resources from MedlinePlus.
- Heart Attack Warning Signals from the Heart and Stroke Foundation of Canada
- Regional PCI for STEMI Resource Center - Evidence based online resource center for the development of regional PCI networks for acute STEMI
- STEMI Systems - Articles, profiles, and reviews of the latest publications involved in STEMI care. Quarterly newsletter.
- American Heart Association's Heart Attack web site - Information and resources for preventing, recognizing and treating heart attack.