Pulmonary edema pathophysiology: Difference between revisions
Usama Talib (talk | contribs) |
Usama Talib (talk | contribs) No edit summary |
||
| Line 18: | Line 18: | ||
The flux of fluid across the capillary wall is controlled by a balance between [[hydrostatic]] pressure and [[osmotic]] pressure gradients between the [[capillaries]] and [[interstitial space]] that can be calculated via [[Starling equation]]: | The flux of fluid across the capillary wall is controlled by a balance between [[hydrostatic]] pressure and [[osmotic]] pressure gradients between the [[capillaries]] and [[interstitial space]] that can be calculated via [[Starling equation]]: | ||
JV =K.S.([Pmv-Ppmv]-σd[πmv-πpmv]) | JV = K.S.([Pmv-Ppmv]-σd[πmv-πpmv]) | ||
where: | where: | ||
| Line 40: | Line 40: | ||
*** It is understood that postobstructive pulmonary edema is caused by highly negative intrathoracic pressure that create by forceful attempts to inhale against an obstruction, this causes elevated venous return, declined cardiac output and fluid transudation into the alveolar space. | *** It is understood that postobstructive pulmonary edema is caused by highly negative intrathoracic pressure that create by forceful attempts to inhale against an obstruction, this causes elevated venous return, declined cardiac output and fluid transudation into the alveolar space. | ||
====== Altered alveolar-capillary membrane permeability(acute respiratory distress syndrome) ====== | ====== Altered alveolar-capillary membrane permeability (acute respiratory distress syndrome) ====== | ||
* In noncardiogenic pulmonary edema, the most common mechanism for a rise in transcapillary filtration is an increase in capillary [[permeability]]. | Following are a few important aspects about altered alveolar capillary membrane permeability leading to pulmonary edema: | ||
* In noncardiogenic pulmonary edema, the most common mechanism for a rise in transcapillary filtration is an increase in capillary [[permeability]]. | |||
* This increase in permeability damages the alveolar-capillary membrane, causing increased movement of water and proteins from the intravascular space to the [[interstitial space]]. | |||
* In most cases of noncardiogenic pulmonary edema, the concentration of protein in the interstitium exceeds 60 percent of the plasma value, compared to less than 45 percent in cardiogenic pulmonary edema. | |||
[[Acute respiratory distress syndrome|ARDS]] can be seen in a number of disorders: | |||
* [[Sepsis]] | |||
* Acute pulmonary infection | |||
* Non-thoracic trauma | |||
* [[Disseminated intravascular coagulation]] | |||
* [[Aspiration]] | |||
====== Lymphatic insufficiency ====== | ====== Lymphatic insufficiency ====== | ||
Lymphatic insufficiency may follow: | |||
* After [[lung transplant]] | * After [[lung transplant]] | ||
* Lymphangitic carcinomatosis | * Lymphangitic carcinomatosis | ||
* Fibrosing [[lymphangitis]] (e.g., [[silicosis]]) | * Fibrosing [[lymphangitis]] (e.g., [[silicosis]]) | ||
====== | ====== Other factors ====== | ||
Various other factors contributing to the development of pulmonary edema include: | |||
* High-altitude pulmonary edema | * High-altitude pulmonary edema | ||
** It is understood that high-altitude pulmonary edema is caused by [[hypoxic]] pulmonary [[vasoconstriction]] at altitudes above 12,000 to 13,000 feet (3600 to 3900 m).<ref name="pmid27645688">{{cite journal |vauthors=Dunham-Snary KJ, Wu D, Sykes EA, Thakrar A, Parlow LR, Mewburn JD, Parlow JL, Archer SL |title=Hypoxic Pulmonary Vasoconstriction: From Molecular Mechanisms to Medicine |journal=Chest |volume=151 |issue=1 |pages=181–192 |year=2017 |pmid=27645688 |pmc=5310129 |doi=10.1016/j.chest.2016.09.001 |url=}}</ref> | ** It is understood that high-altitude pulmonary edema is caused by [[hypoxic]] pulmonary [[vasoconstriction]] at altitudes above 12,000 to 13,000 feet (3600 to 3900 m).<ref name="pmid27645688">{{cite journal |vauthors=Dunham-Snary KJ, Wu D, Sykes EA, Thakrar A, Parlow LR, Mewburn JD, Parlow JL, Archer SL |title=Hypoxic Pulmonary Vasoconstriction: From Molecular Mechanisms to Medicine |journal=Chest |volume=151 |issue=1 |pages=181–192 |year=2017 |pmid=27645688 |pmc=5310129 |doi=10.1016/j.chest.2016.09.001 |url=}}</ref> | ||
Revision as of 15:44, 16 February 2018
|
Pulmonary edema Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pulmonary edema pathophysiology On the Web |
|
Risk calculators and risk factors for Pulmonary edema pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Pulmonary edema is due to either failure of the heart to remove fluid from the lung circulation ("cardiogenic pulmonary edema"), or due to a direct injury to the lung parenchyma or increased permeability or leakiness of the capillaries ("noncardiogenic pulmonary edema").
Pathophysiology
It is understood that pulmonary edema is the abnormal increase in extravascular lung water (EVLW). Pulmonary edema is caused by either:[1][2][3]
- Imbalance of staling force
- Altered valvular capillary membrane permeability
- Lymphatic insufficiency
- Other factors
These factors have been described bellow:
Imbalance of starling force
The flux of fluid across the capillary wall is controlled by a balance between hydrostatic pressure and osmotic pressure gradients between the capillaries and interstitial space that can be calculated via Starling equation:
JV = K.S.([Pmv-Ppmv]-σd[πmv-πpmv])
where:
- JV = volume flow across the capillary bed
- K = filtration coefficient of the capillary wall
- S = surface area of the capillary bed
- Pmv = microvascular hydrostatic pressure
- Ppmv = perimicrovascular (interstitial) hydrostatic pressure
- πmv = plasma colloid osmotic pressure
- πpmv = perimicrovascular (interstitial) colloid osmotic pressure
- σd = protein reflection coefficient
- Increase pulmonary capillary pressure
- In cardiogenic pulmonary edema, the most common mechanism for a rise in transcapillary filtration is an increase in pulmonary capillary pressure.
- Left ventricular failure
- Left ventricular outflow obstruction
- Mitral stenosis
- In cardiogenic pulmonary edema, the most common mechanism for a rise in transcapillary filtration is an increase in pulmonary capillary pressure.
- Increase negative interstitial pressure
- Negative-pressure pulmonary edema (NPPE) or postobstructive pulmonary edema[4]
- It is understood that postobstructive pulmonary edema is caused by highly negative intrathoracic pressure that create by forceful attempts to inhale against an obstruction, this causes elevated venous return, declined cardiac output and fluid transudation into the alveolar space.
- Negative-pressure pulmonary edema (NPPE) or postobstructive pulmonary edema[4]
Altered alveolar-capillary membrane permeability (acute respiratory distress syndrome)
Following are a few important aspects about altered alveolar capillary membrane permeability leading to pulmonary edema:
- In noncardiogenic pulmonary edema, the most common mechanism for a rise in transcapillary filtration is an increase in capillary permeability.
- This increase in permeability damages the alveolar-capillary membrane, causing increased movement of water and proteins from the intravascular space to the interstitial space.
- In most cases of noncardiogenic pulmonary edema, the concentration of protein in the interstitium exceeds 60 percent of the plasma value, compared to less than 45 percent in cardiogenic pulmonary edema.
ARDS can be seen in a number of disorders:
- Sepsis
- Acute pulmonary infection
- Non-thoracic trauma
- Disseminated intravascular coagulation
- Aspiration
Lymphatic insufficiency
Lymphatic insufficiency may follow:
- After lung transplant
- Lymphangitic carcinomatosis
- Fibrosing lymphangitis (e.g., silicosis)
Other factors
Various other factors contributing to the development of pulmonary edema include:
- High-altitude pulmonary edema
- It is understood that high-altitude pulmonary edema is caused by hypoxic pulmonary vasoconstriction at altitudes above 12,000 to 13,000 feet (3600 to 3900 m).[5]
- Neurogenic pulmonary edema
- It is understood that neurogenic pulmonary edema is caused by sympathetic overreactivity with massive catecholamine surges that shifts blood from the systemic to the pulmonary circulation.[6]
- Narcotic overdose
- The exact pathogenesis of narcotic overdose pulmonary edema is not fully understood. Proposed mechanisms include combination of direct toxicity of the drug, hypoxia, and acidosis secondary to hypoventilation and/or cerebral edema.[7]
- Pulmonary embolism
- It is understood that pulmonary embolism can cause pulmonary edema by damaging the pulmonary and nearby pleural systemic circulations, increasing hydrostatic pressures in pulmonary and/or systemic veins, and decreasing pleural pressure due to atelectasis.[8]
- Re-expansion pulmonary edema
- The exact pathogenesis of re-expansion pulmonary edema is not fully understood. Direct injury from surfactant dysfunction in chronic atelectatic lung, elevated transpleural pressures, or indirect injury from reperfusion has been proposed.[9]
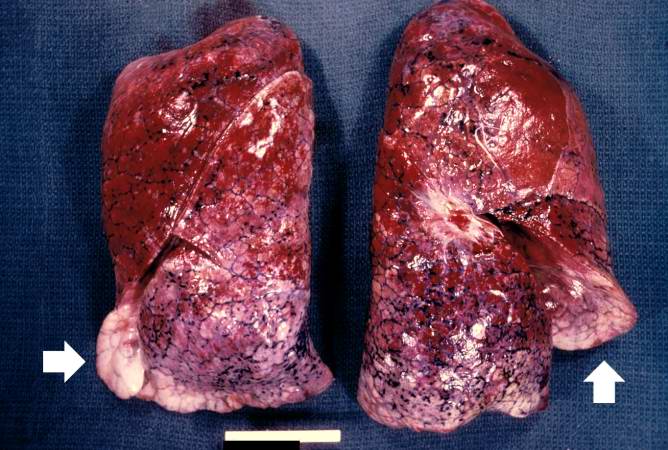
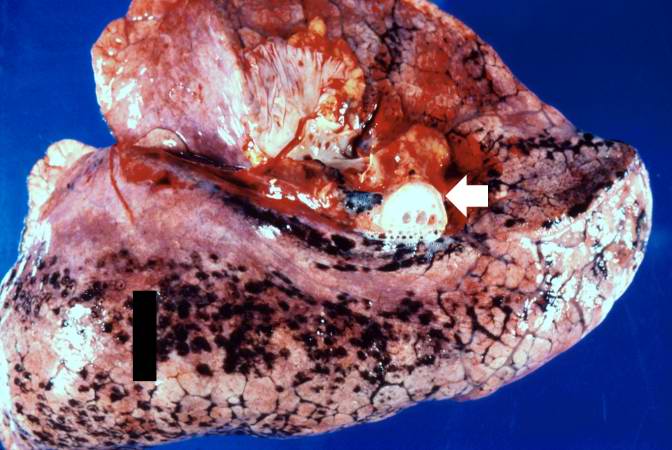
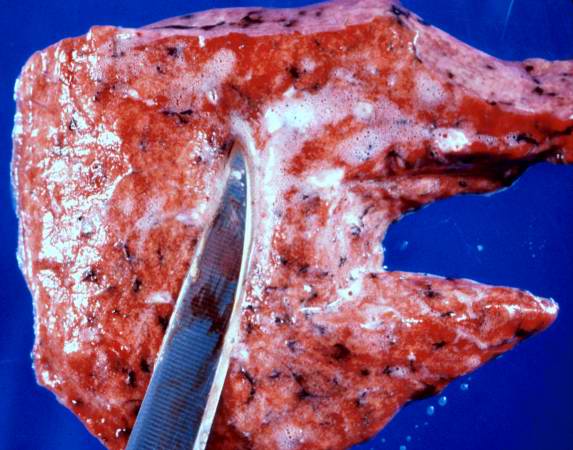
Gross Pathology
-
This is a gross photograph of lungs that are distended and red. The reddish coloration of the tissue is due to congestion. Some normal pink lung tissue is seen at the edges of the lungs (arrows).
-
This is a gross photograph of lung demonstrating acute pulmonary congestion and edema. A frothy exudate fills the bronchus (arrow).
-
This gross photograph demonstrates the frothy exudate that is being extruded from the lung tissue.
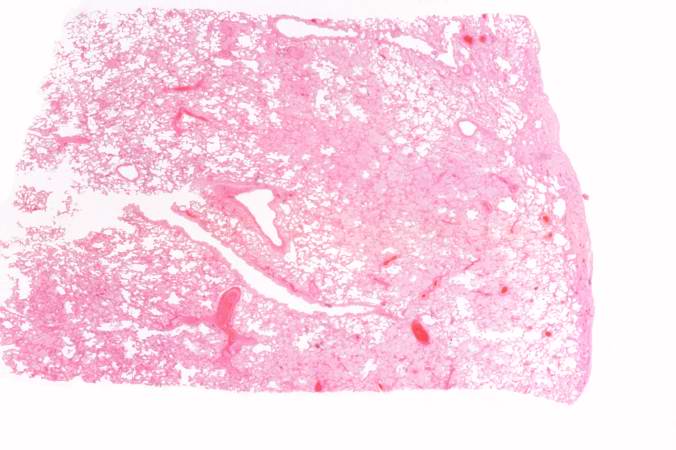
Microscopic Pathology
-
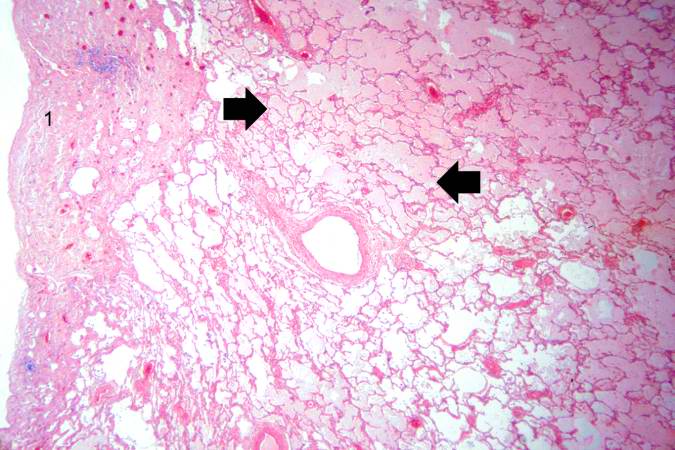
This is a low-power photomicrograph of lung from this case. The lung section has a pale-red color indicating proteinaceous material within the lung.
-
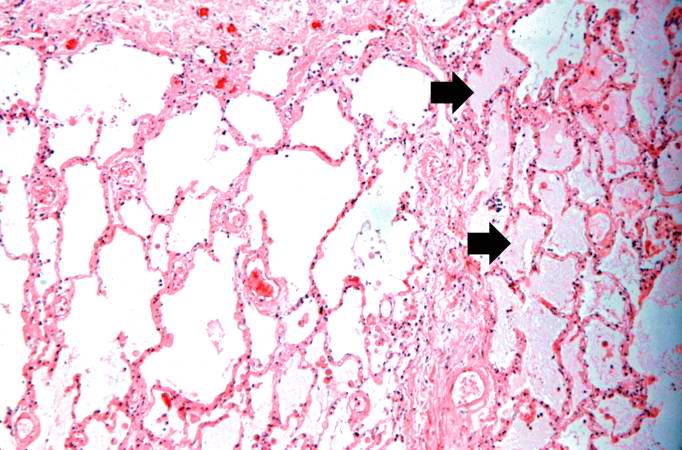
This is a higher-power photomicrograph of lung. The edema fluid within the alveoli is visible at this higher magnification (arrows). The thickened pleura (1) is on the left.
-
This is a higher-power photomicrograph showing edema-filled alveoli in the right portion of this section (arrows).
-
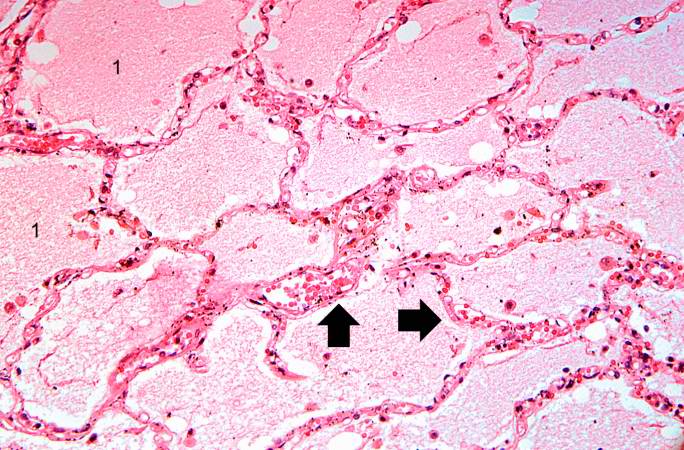
This high-power photomicrograph illustrates the edema fluid within the alveoli (1) and the congestion (RBCs) in the alveolar capillaries (arrows).
References
- ↑ Sibbald WJ, Cunningham DR, Chin DN (1983). "Non-cardiac or cardiac pulmonary edema? A practical approach to clinical differentiation in critically ill patients". Chest. 84 (4): 452–61. PMID 6617283.
- ↑ Ware LB, Matthay MA (2005). "Clinical practice. Acute pulmonary edema". N. Engl. J. Med. 353 (26): 2788–96. doi:10.1056/NEJMcp052699. PMID 16382065.
- ↑ Pena-Gil C, Figueras J, Soler-Soler J (2005). "Acute cardiogenic pulmonary edema--relevance of multivessel disease, conduction abnormalities and silent ischemia". Int. J. Cardiol. 103 (1): 59–66. doi:10.1016/j.ijcard.2004.08.029. PMID 16061125.
- ↑ Bhattacharya M, Kallet RH, Ware LB, Matthay MA (2016). "Negative-Pressure Pulmonary Edema". Chest. 150 (4): 927–933. doi:10.1016/j.chest.2016.03.043. PMID 27063348.
- ↑ Dunham-Snary KJ, Wu D, Sykes EA, Thakrar A, Parlow LR, Mewburn JD, Parlow JL, Archer SL (2017). "Hypoxic Pulmonary Vasoconstriction: From Molecular Mechanisms to Medicine". Chest. 151 (1): 181–192. doi:10.1016/j.chest.2016.09.001. PMC 5310129. PMID 27645688.
- ↑ Busl KM, Bleck TP (2015). "Neurogenic Pulmonary Edema". Crit. Care Med. 43 (8): 1710–5. doi:10.1097/CCM.0000000000001101. PMID 26066018.
- ↑ Radke JB, Owen KP, Sutter ME, Ford JB, Albertson TE (2014). "The effects of opioids on the lung". Clin Rev Allergy Immunol. 46 (1): 54–64. doi:10.1007/s12016-013-8373-z. PMID 23636734.
- ↑ Porcel JM, Light RW (2008). "Pleural effusions due to pulmonary embolism". Curr Opin Pulm Med. 14 (4): 337–42. doi:10.1097/MCP.0b013e3282fcea3c. PMID 18520269.
- ↑ Feller-Kopman D, Berkowitz D, Boiselle P, Ernst A (2007). "Large-volume thoracentesis and the risk of reexpansion pulmonary edema". Ann. Thorac. Surg. 84 (5): 1656–61. doi:10.1016/j.athoracsur.2007.06.038. PMID 17954079.