Prostate cancer pathophysiology
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Syed Musadiq Ali M.B.B.S.[2]
|
Prostate cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Prostate cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Prostate cancer pathophysiology |
|
Risk calculators and risk factors for Prostate cancer pathophysiology |
Overview
On microscopic histopathological analysis, increased gland density, small circular glands, basal cells lacking, and cytological abnormalities are characteristic findings of prostate cancer.
Pathogenesis
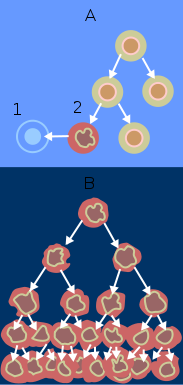
- Prostate cancers can be lethal because they heterogeneously contain both androgen-dependent and androgen-independent malignant cells[1]
- For those cells that are androgen dependent, a critical level of androgen is required to activate a sufficient number of androgen receptors (ARs) so that transcription of death-signaling genes is expressed
- Androgens are capable of both stimulating proliferation as well as inhibiting the rate of the glandular epithelial cell death
- Androgen withdrawal triggers the programmed cell death pathway in both normal prostate glandular epithelia and androgen-dependent prostate cancer cells
- Androgen-independent prostate cancer cells do not initiate the programmed cell death pathway upon androgen ablation; however, they do retain the cellular machinery necessary to activate the programmed cell death cascade when sufficiently damaged by exogenous agents
Inherited Prostate-Cancer–Susceptibility Genes
- Rare autosomal dominant alleles account for a substantial proportion of cases of inherited, early-onset prostate cancer (defined as cancer occurring before 55 years of age)[2]
- In families with men in whom prostate cancer is diagnosed at an older age, an X-linked allele may be responsible [3]
- The first molecular genetic study of familial prostate cancer in which polymorphic markers were used identified several regions of linkage; the chromosomal region 1q24–25, designated the locus of the hereditary prostate cancer (HPC1) gene, has been the most thoroughly investigated[4]
- Some analyses have confirmed a link between HPC1 and prostate cancer, but others have failed to detect an association[5]
RNASEL
- The RNASEL gene encodes a widely expressed latent endoribonuclease that participates in an interferon-inducible RNA-decay pathway that is thought to degrade viral and cellular RNA[6]
- RNASEL has been linked to HPC1. In one family, four brothers with prostate cancer carried a disabling mutation of RNASEL, and in another family, four of six brothers with prostate cancer carried a base substitution affecting the RNASEL initiator methionine codon[7]
MSR1
- The macrophage-scavenger receptor 1 (MSR1) gene, located at 8p22, has also emerged as a candidate prostate-cancer–susceptibility gene[8]
- It encodes subunits of a macrophage-scavenger receptor that is capable of binding a variety of ligands, including bacterial lipopolysaccharide and lipoteichoic acid, and oxidized high-density lipoprotein and low-density lipoprotein in the serum[9]
- Germ-line MSR1 mutations have been linked to prostate cancer in some families with hereditary prostate cancer, and one mutant MSR1 allele has been detected in approximately 3 percent of men with non-hereditary prostate cancer but only 0.4 percent of unaffected men (P=0.05)[10]
AR, CYP17, AND SRD5A2
- Polymorphic variants of three genes involved in androgen action, the androgen-receptor (AR) gene, the cytochrome P-450c17 (CYP17) gene, and the steroid-5-α-reductase type II (SRD5A2) gene, have been implicated in modifying the risk of prostate cancer in genetic epidemiologic studies. In the case of AR, which encodes the androgen receptor, polymorphic polyglutamine (CAG) repeats have been described[11]
- Functional studies have suggested that shorter polyglutamine repeats may be associated with increased androgen-receptor transcriptional transactivation activity[12]
- Black Americans, who have a relatively high risk of prostate cancer, tend to have shorter androgen-receptor polyglutamine repeats, whereas Asians, who have a relatively low risk of prostate cancer, tend to have longer androgen-receptor polyglutamine repeats. Several genetic epidemiologic studies have shown a correlation between an increased risk of prostate cancer and the presence of short androgen-receptor polyglutamine repeats, but other studies have failed to detect such a correlation[13]
- Polymorphic polyglycine (GGC) repeats are also characteristic of AR and may also influence the risk of prostate cancer.76,79-81
- CYP17 encodes cytochrome P-450c17α, an enzyme that catalyzes key reactions in sex-steroid biosynthesis. A variant CYP17 allele has been subjected to both population and genetic-linkage analyses to determine its association with prostate cancer, with inconsistent results.75,82-88 However, linkage data suggest that another variant CYP17 allele is associated with prostate cancer.89
- SRD5A2 encodes the predominant isozyme of 5-α-reductase in the prostate, an enzyme that converts testosterone to the more potent dihydrotestosterone. Two common polymorphic variant SRD5A2 alleles have been described.90,91
- The alleles that encode enzymes with increased activity have been associated with an increased risk of prostate cancer and with a poor prognosis for men with prostate cancer.90,92
- In addition to AR, CYP17, and SRD5A2, polymorphic variants of a number of other genes have been proposed as possible contributors to the risk of prostate cancer.93
GENETIC SUSCEPTIBILITY TO PROSTATE CANCER
- As we have seen, the genetics of the prostate have proved difficult to study. Prostate cancer, once generally diagnosed at an advanced stage in older men, is now more often detected at an early stage in younger men as a consequence of more widespread screening for the disease. This trend toward earlier diagnosis of prostate cancer has most likely changed the definition of a “case” of cancer, since many men who would have qualified as controls in previous genetic and epidemiologic studies are now known to have prostate cancer as a result of PSA screening. Despite these limitations, genetic studies have provided remarkable clues to the causes of prostate cancer. For example, in addition to the expected role of androgens in facilitating the development of prostate cancer, the possibility that viral or bacterial infections might lead to prostate cancer has been raised with the identification of RNASEL and MSR1 as familial prostate-cancer genes — an insight that will profoundly affect future studies of the etiology of prostate cancer and may ultimately lead to new approaches to the prevention of prostate cancer (Table 1).61,66,67,94
- Prostate cancer is classified as an adenocarcinoma, or glandular cancer. The region of prostate gland where the adenocarcinoma is most common is the peripheral zone.[14]
- Initially, small clumps of cancer cells remain confined to otherwise normal prostate glands, a condition known as carcinoma in situ or prostatic intraepithelial neoplasia (PIN).[15]
- Although there is no proof that PIN is a cancer precursor, it is closely associated with cancer. Over time these cancer cells begin to multiply and spread to the surrounding prostate tissue (the stroma) forming a tumor.[15]
- Eventually, the tumor may grow large enough to invade nearby organs such as the seminal vesicles or the rectum, or the tumor cells may develop the ability to travel in the blood stream and lymphatic system.[15]
- Prostate cancer is considered a malignant tumor because it is a mass of cells which can invade other parts of the body. This invasion of other organs is called metastasis. Prostate cancer most commonly metastasizes to the bones, lymph nodes, rectum, and bladder.[15]
- Prostate gland is a zinc-accumulating, citrate-producing organ[16]
- The protein ZIP1 is required for the active transport of zinc into prostate cells
- Zinc have important role to change the metabolism of the cell in order to produce citrate, an important component of semen
- The process of zinc accumulation and citrate production is energy inefficient and prostate cells sacrifice enormous of energy (ATP) in order to complete this task.
- Prostate cancer cells are generally devoid of zinc. This allows prostate cancer cells to save energy not making citrate, and utilize the new abundance of energy to grow and spread
- The absence of zinc is thought to occur via a silencing of the gene that producing the transporter protein ZIP1
- ZIP1 is now called a tumor suppressor gene product for the gene SLC39A1.The cause of epigenetic silencing is unknown
- Zinc inhibits BF-kB pathways, Is anti- proliferative,and induces apoptosis in abnormal cells
- Unfortunately, oral ingestion of zinc is not effective because high concentrations of zinc into prostate cells is not possible without the active transporter ZIP1
- RUNX2 is a transcription factor that prevents the cancer cells from undergoing apoptosis thereby contributing to the development of prostate cancer
- The androgen receptor helps prostate cancer cells to survive and is a target for many anticancer research studies; so far, inhibiting androgen receptor
- Prostate specific membrane antigen(PSMA) stimulates the development of prostate cancer by increasing folate levels for cancer cells to use to survive and grow
- PSMA increases available folates for use by hydrolyzing glutamate folate
Gross Pathology
Prostate cancer is uncommonly apparent on gross.[17]
Microscopic Pathology
- Architecture
- Increased gland density
- Small circular glands
- In rare subtypes - large branching glands
- Basal cells lacking
- Cytological abnormalities:
Minor criteria:
- Nuclear hyperchromasia
- Wispy blue mucin
- Pink amorphous secretions
- Intraluminal crystalloid
- Amphophilic cytoplasm
- Adjacent High-grade prostatic intraepithelial neoplasia (HGPIN)
- Mitoses - quite rare
Prostate adenocarcinoma: Microscopic View
{{#ev:youtube|1SZPLS1dxTo}}
Gleason score
- See Gleason score
Prostate: Adenocarcinoma (Gleason grade 1)
{{#ev:youtube|F7V0Zl7a2FY}}
Prostate: Adenocarcinoma (Gleason grade 2)
{{#ev:youtube|YSOLiSklIXw}}
Prostate: Adenocarcinoma (Gleason grade 3)
{{#ev:youtube|TG8vR_pE7yA}}
Prostate: Adenocarcinoma (Gleason grade 4)
{{#ev:youtube|R2Cl4HScdGc}}
Prostate: Adenocarcinoma (Gleason grade 5)
{{#ev:youtube|F7V0Zl7a2FY}}
References
- ↑ Denmeade SR, Lin XS, Isaacs JT (April 1996). "Role of programmed (apoptotic) cell death during the progression and therapy for prostate cancer". Prostate. 28 (4): 251–65. doi:10.1002/(SICI)1097-0045(199604)28:4<251::AID-PROS6>3.0.CO;2-G. PMID 8602401.
- ↑ Carter BS, Beaty TH, Steinberg GD, Childs B, Walsh PC (April 1992). "Mendelian inheritance of familial prostate cancer". Proc. Natl. Acad. Sci. U.S.A. 89 (8): 3367–71. PMC 48868. PMID 1565627.
- ↑ Cui J, Staples MP, Hopper JL, English DR, McCredie MR, Giles GG (May 2001). "Segregation analyses of 1,476 population-based Australian families affected by prostate cancer". Am. J. Hum. Genet. 68 (5): 1207–18. doi:10.1086/320114. PMC 1226101. PMID 11309686.
- ↑ Smith JR, Freije D, Carpten JD, Grönberg H, Xu J, Isaacs SD, Brownstein MJ, Bova GS, Guo H, Bujnovszky P, Nusskern DR, Damber JE, Bergh A, Emanuelsson M, Kallioniemi OP, Walker-Daniels J, Bailey-Wilson JE, Beaty TH, Meyers DA, Walsh PC, Collins FS, Trent JM, Isaacs WB (November 1996). "Major susceptibility locus for prostate cancer on chromosome 1 suggested by a genome-wide search". Science. 274 (5291): 1371–4. PMID 8910276.
- ↑ Ostrander EA, Stanford JL (December 2000). "Genetics of prostate cancer: too many loci, too few genes". Am. J. Hum. Genet. 67 (6): 1367–75. doi:10.1086/316916. PMC 1287913. PMID 11067781.
- ↑ Silverman RH, Jung DD, Nolan-Sorden NL, Dieffenbach CW, Kedar VP, SenGupta DN (May 1988). "Purification and analysis of murine 2-5A-dependent RNase". J. Biol. Chem. 263 (15): 7336–41. PMID 3366783.
- ↑ Carpten J, Nupponen N, Isaacs S, Sood R, Robbins C, Xu J, Faruque M, Moses T, Ewing C, Gillanders E, Hu P, Bujnovszky P, Makalowska I, Baffoe-Bonnie A, Faith D, Smith J, Stephan D, Wiley K, Brownstein M, Gildea D, Kelly B, Jenkins R, Hostetter G, Matikainen M, Schleutker J, Klinger K, Connors T, Xiang Y, Wang Z, De Marzo A, Papadopoulos N, Kallioniemi OP, Burk R, Meyers D, Grönberg H, Meltzer P, Silverman R, Bailey-Wilson J, Walsh P, Isaacs W, Trent J (February 2002). "Germline mutations in the ribonuclease L gene in families showing linkage with HPC1". Nat. Genet. 30 (2): 181–4. doi:10.1038/ng823. PMID 11799394.
- ↑ Xu J, Zheng SL, Komiya A, Mychaleckyj JC, Isaacs SD, Hu JJ, Sterling D, Lange EM, Hawkins GA, Turner A, Ewing CM, Faith DA, Johnson JR, Suzuki H, Bujnovszky P, Wiley KE, DeMarzo AM, Bova GS, Chang B, Hall MC, McCullough DL, Partin AW, Kassabian VS, Carpten JD, Bailey-Wilson JE, Trent JM, Ohar J, Bleecker ER, Walsh PC, Isaacs WB, Meyers DA (October 2002). "Germline mutations and sequence variants of the macrophage scavenger receptor 1 gene are associated with prostate cancer risk". Nat. Genet. 32 (2): 321–5. doi:10.1038/ng994. PMID 12244320.
- ↑ Platt N, Gordon S (September 2001). "Is the class A macrophage scavenger receptor (SR-A) multifunctional? - The mouse's tale". J. Clin. Invest. 108 (5): 649–54. doi:10.1172/JCI13903. PMC 209390. PMID 11544267.
- ↑ Dejager S, Mietus-Snyder M, Friera A, Pitas RE (August 1993). "Dominant negative mutations of the scavenger receptor. Native receptor inactivation by expression of truncated variants". J. Clin. Invest. 92 (2): 894–902. doi:10.1172/JCI116664. PMC 294928. PMID 8349824.
- ↑ Edwards A, Hammond HA, Jin L, Caskey CT, Chakraborty R (February 1992). "Genetic variation at five trimeric and tetrameric tandem repeat loci in four human population groups". Genomics. 12 (2): 241–53. PMID 1740333.
- ↑ Chamberlain NL, Driver ED, Miesfeld RL (August 1994). "The length and location of CAG trinucleotide repeats in the androgen receptor N-terminal domain affect transactivation function". Nucleic Acids Res. 22 (15): 3181–6. PMC 310294. PMID 8065934.
- ↑ Bennett CL, Price DK, Kim S, Liu D, Jovanovic BD, Nathan D, Johnson ME, Montgomery JS, Cude K, Brockbank JC, Sartor O, Figg WD (September 2002). "Racial variation in CAG repeat lengths within the androgen receptor gene among prostate cancer patients of lower socioeconomic status". J. Clin. Oncol. 20 (17): 3599–604. doi:10.1200/JCO.2002.11.085. PMID 12202660.
- ↑ "Prostate Cancer". National Cancer Institute. Retrieved 12 October 2014.
- ↑ 15.0 15.1 15.2 15.3 "Male Genitals - Prostate Neoplasms". Pathology study images. University of Virginia School of Medicine. Archived from the original on 2011-04-28. Retrieved 2011-04-28.
There are many connections between the prostatic venous plexus and the vertebral veins. The veins forming the prostatic plexus do not contain valves and it is thought that straining to urinate causes prostatic venous blood to flow in a reverse direction and enter the vertebral veins carrying malignant cells to the vertebral column.
- ↑ . doi:10.9790/0853-1506020411. Missing or empty
|title=(help) - ↑ Prostatic carcinoma.Dr Ian Bickle and Dr Saqba Farooq et al. Radiopaedia.org 2015.http://radiopaedia.org/articles/prostatic-carcinoma-1
- ↑ Humphrey PA (2007). "Diagnosis of adenocarcinoma in prostate needle biopsy tissue". J. Clin. Pathol. 60 (1): 35–42. doi:10.1136/jcp.2005.036442. PMC 1860598. PMID 17213347. Unknown parameter
|month=ignored (help) - ↑ "Prostate cancer.Libre pathology 2015".