Prostate cancer pathophysiology: Difference between revisions
| Line 7: | Line 7: | ||
==Pathogenesis== | ==Pathogenesis== | ||
*Prostate cancers can be lethal because they heterogeneously contain both androgen-dependent and androgen-independent malignant cells<ref name="pmid8602401">{{cite journal |vauthors=Denmeade SR, Lin XS, Isaacs JT |title=Role of programmed (apoptotic) cell death during the progression and therapy for prostate cancer |journal=Prostate |volume=28 |issue=4 |pages=251–65 |date=April 1996 |pmid=8602401 |doi=10.1002/(SICI)1097-0045(199604)28:4<251::AID-PROS6>3.0.CO;2-G |url=}}</ref> | |||
*For those cells that are androgen dependent, a critical level of androgen is required to activate a sufficient number of androgen receptors (ARs) so that transcription of death-signaling genes is expressed | *For those cells that are androgen dependent, a critical level of androgen is required to activate a sufficient number of androgen receptors (ARs) so that transcription of death-signaling genes is expressed | ||
*Androgens are capable of both stimulating proliferation as well as inhibiting the rate of the glandular epithelial cell death | *Androgens are capable of both stimulating proliferation as well as inhibiting the rate of the glandular epithelial cell death | ||
Revision as of 17:14, 21 December 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Syed Musadiq Ali M.B.B.S.[2]
|
Prostate cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Prostate cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Prostate cancer pathophysiology |
|
Risk calculators and risk factors for Prostate cancer pathophysiology |
Overview
On microscopic histopathological analysis, increased gland density, small circular glands, basal cells lacking, and cytological abnormalities are characteristic findings of prostate cancer.
Pathogenesis
- Prostate cancers can be lethal because they heterogeneously contain both androgen-dependent and androgen-independent malignant cells[1]
- For those cells that are androgen dependent, a critical level of androgen is required to activate a sufficient number of androgen receptors (ARs) so that transcription of death-signaling genes is expressed
- Androgens are capable of both stimulating proliferation as well as inhibiting the rate of the glandular epithelial cell death
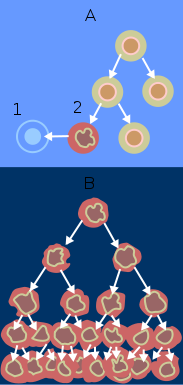
- Androgen withdrawal triggers the programmed cell death pathway in both normal prostate glandular epithelia and androgen-dependent prostate cancer cells
- Androgen withdrawal triggers the programmed cell death pathway in both normal prostate glandular epithelia and androgen-dependent prostate cancer cells
- Androgen-independent prostate cancer cells do not initiate the programmed cell death pathway upon androgen ablation; however, they do retain the cellular machinery necessary to activate the programmed cell death cascade when sufficiently damaged by exogenous agents
- Prostate cancer is classified as an adenocarcinoma, or glandular cancer. The region of prostate gland where the adenocarcinoma is most common is the peripheral zone.[2]
- Initially, small clumps of cancer cells remain confined to otherwise normal prostate glands, a condition known as carcinoma in situ or prostatic intraepithelial neoplasia (PIN).[3]
- Although there is no proof that PIN is a cancer precursor, it is closely associated with cancer. Over time these cancer cells begin to multiply and spread to the surrounding prostate tissue (the stroma) forming a tumor.[3]
- Eventually, the tumor may grow large enough to invade nearby organs such as the seminal vesicles or the rectum, or the tumor cells may develop the ability to travel in the blood stream and lymphatic system.[3]
- Prostate cancer is considered a malignant tumor because it is a mass of cells which can invade other parts of the body. This invasion of other organs is called metastasis. Prostate cancer most commonly metastasizes to the bones, lymph nodes, rectum, and bladder.[3]
- Prostate gland is a zinc-accumulating, citrate-producing organ[4]
- The protein ZIP1 is required for the active transport of zinc into prostate cells
- Zinc have important role to change the metabolism of the cell in order to produce citrate, an important component of semen
- The process of zinc accumulation and citrate production is energy inefficient and prostate cells sacrifice enormous of energy (ATP) in order to complete this task.
- Prostate cancer cells are generally devoid of zinc. This allows prostate cancer cells to save energy not making citrate, and utilize the new abundance of energy to grow and spread
- The absence of zinc is thought to occur via a silencing of the gene that producing the transporter protein ZIP1
- ZIP1 is now called a tumor suppressor gene product for the gene SLC39A1.The cause of epigenetic silencing is unknown
- Zinc inhibits BF-kB pathways, Is anti- proliferative,and induces apoptosis in abnormal cells
- Unfortunately, oral ingestion of zinc is not effective because high concentrations of zinc into prostate cells is not possible without the active transporter ZIP1
- RUNX2 is a transcription factor that prevents the cancer cells from undergoing apoptosis thereby contributing to the development of prostate cancer
- The androgen receptor helps prostate cancer cells to survive and is a target for many anticancer research studies; so far, inhibiting androgen receptor
- Prostate specific membrane antigen(PSMA) stimulates the development of prostate cancer by increasing folate levels for cancer cells to use to survive and grow
- PSMA increases available folates for use by hydrolyzing glutamate folate
Gross Pathology
Prostate cancer is uncommonly apparent on gross.[5]
Microscopic Pathology
- Architecture
- Increased gland density
- Small circular glands
- In rare subtypes - large branching glands
- Basal cells lacking
- Cytological abnormalities:
Minor criteria:
- Nuclear hyperchromasia
- Wispy blue mucin
- Pink amorphous secretions
- Intraluminal crystalloid
- Amphophilic cytoplasm
- Adjacent High-grade prostatic intraepithelial neoplasia (HGPIN)
- Mitoses - quite rare
Prostate adenocarcinoma: Microscopic View
{{#ev:youtube|1SZPLS1dxTo}}
Gleason score
- See Gleason score
Prostate: Adenocarcinoma (Gleason grade 1)
{{#ev:youtube|F7V0Zl7a2FY}}
Prostate: Adenocarcinoma (Gleason grade 2)
{{#ev:youtube|YSOLiSklIXw}}
Prostate: Adenocarcinoma (Gleason grade 3)
{{#ev:youtube|TG8vR_pE7yA}}
Prostate: Adenocarcinoma (Gleason grade 4)
{{#ev:youtube|R2Cl4HScdGc}}
Prostate: Adenocarcinoma (Gleason grade 5)
{{#ev:youtube|F7V0Zl7a2FY}}
References
- ↑ Denmeade SR, Lin XS, Isaacs JT (April 1996). "Role of programmed (apoptotic) cell death during the progression and therapy for prostate cancer". Prostate. 28 (4): 251–65. doi:10.1002/(SICI)1097-0045(199604)28:4<251::AID-PROS6>3.0.CO;2-G. PMID 8602401.
- ↑ "Prostate Cancer". National Cancer Institute. Retrieved 12 October 2014.
- ↑ 3.0 3.1 3.2 3.3 "Male Genitals - Prostate Neoplasms". Pathology study images. University of Virginia School of Medicine. Archived from the original on 2011-04-28. Retrieved 2011-04-28.
There are many connections between the prostatic venous plexus and the vertebral veins. The veins forming the prostatic plexus do not contain valves and it is thought that straining to urinate causes prostatic venous blood to flow in a reverse direction and enter the vertebral veins carrying malignant cells to the vertebral column.
- ↑ . doi:10.9790/0853-1506020411. Missing or empty
|title=(help) - ↑ Prostatic carcinoma.Dr Ian Bickle and Dr Saqba Farooq et al. Radiopaedia.org 2015.http://radiopaedia.org/articles/prostatic-carcinoma-1
- ↑ Humphrey PA (2007). "Diagnosis of adenocarcinoma in prostate needle biopsy tissue". J. Clin. Pathol. 60 (1): 35–42. doi:10.1136/jcp.2005.036442. PMC 1860598. PMID 17213347. Unknown parameter
|month=ignored (help) - ↑ "Prostate cancer.Libre pathology 2015".