Peptic ulcer pathophysiology: Difference between revisions
| Line 65: | Line 65: | ||
===Role of NSAIDS=== | ===Role of NSAIDS=== | ||
*NSAID's are more commonly responsible for gasrtic ulcers than duodenal ulcers | |||
*NSAID's inhibit systemic prostaglandins production and cause ulcers<ref name="pmid1882793">{{cite journal |vauthors=Borody TJ, George LL, Brandl S, Andrews P, Ostapowicz N, Hyland L, Devine M |title=Helicobacter pylori-negative duodenal ulcer |journal=Am. J. Gastroenterol. |volume=86 |issue=9 |pages=1154–7 |year=1991 |pmid=1882793 |doi= |url=}}</ref> | *NSAID's inhibit systemic prostaglandins production and cause ulcers<ref name="pmid1882793">{{cite journal |vauthors=Borody TJ, George LL, Brandl S, Andrews P, Ostapowicz N, Hyland L, Devine M |title=Helicobacter pylori-negative duodenal ulcer |journal=Am. J. Gastroenterol. |volume=86 |issue=9 |pages=1154–7 |year=1991 |pmid=1882793 |doi= |url=}}</ref> | ||
*Inhibition of prostaglandins results in decreased blood flow and decreased mucus production resulting in mucosal damage | *Inhibition of prostaglandins results in decreased blood flow and decreased mucus production resulting in mucosal damage.<ref name="pmid11809181">{{cite journal |vauthors=Huang JQ, Sridhar S, Hunt RH |title=Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: a meta-analysis |journal=Lancet |volume=359 |issue=9300 |pages=14–22 |year=2002 |pmid=11809181 |doi=10.1016/S0140-6736(02)07273-2 |url=}}</ref><ref name="pmid1855677">{{cite journal |vauthors=Holvoet J, Terriere L, Van Hee W, Verbist L, Fierens E, Hautekeete ML |title=Relation of upper gastrointestinal bleeding to non-steroidal anti-inflammatory drugs and aspirin: a case-control study |journal=Gut |volume=32 |issue=7 |pages=730–4 |year=1991 |pmid=1855677 |pmc=1378985 |doi= |url=}}</ref> | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | | | A01 | | | | | |A01=NSAIDs}} | {{familytree | | | | | | | | | A01 | | | | | |A01=NSAIDs}} | ||
Revision as of 16:05, 24 November 2017
|
Peptic ulcer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
2017 ACG Guidelines for Peptic Ulcer Disease |
|
Guidelines for the Indications to Test for, and to Treat, H. pylori Infection |
|
Guidlines for factors that predict the successful eradication when treating H. pylori infection |
|
Guidelines to document H. pylori antimicrobial resistance in the North America |
|
Guidelines for evaluation and testing of H. pylori antibiotic resistance |
|
Guidelines for when to test for treatment success after H. pylori eradication therapy |
|
Guidelines for penicillin allergy in patients with H. pylori infection |
|
Peptic ulcer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Peptic ulcer pathophysiology |
|
Risk calculators and risk factors for Peptic ulcer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ;Associate Editor(s)-in-Chief: Manpreet Kaur, MD [2]
Overview
A major causative factor (60% of gastric and 90% of duodenal ulcers) is chronic inflammation due to Helicobacter pylori that colonize the antral mucosa. The immune system is unable to clear the infection, despite the appearance of antibodies. Thus, the bacterium can cause a chronic active gastritis (type B gastritis), resulting in a defect in the regulation of gastrin production and gastrin secretion is increased. Gastrin stimulates the production of gastric acid by parietal cells. The acid erodes the mucosa and causes the ulcer. Another major cause is the use of NSAIDs The gastric mucosa protects itself from gastric acid with a layer of mucus, the secretion of which is stimulated by certain prostaglandins. NSAIDs block the function of cyclooxygenase 1 (cox-1), which is essential for the production of these prostaglandins.
Pathophysiology
Peptic ulcer occurs due to distruption of muscularis mucosa which occurs due to loss of defensive mechanism of gastric mucosa
Defensive mechanism of gastric mucosa
Mucosal barrier
- Mucosal barrier consists of three protective components which include:[1][2][3][4]
- Layer of epithelial cell lining:bound by tight junctions that repel fluids
- Layer of mucus, secreted by surface epithelial cells and foveolar cells:Forms a protective gel-like coating over the entire gastric mucosal surface
- Layer of bicarbonate ions, secreted by the surface epithelial cells:Neutralize acids
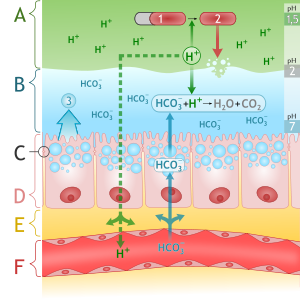
Source:Wikimedia Commons [5]
The two most important etiological factors in the development of PUD are:[6][7][8]
Role of Helicobacter pylori
- Helicobacter pylori is gram-negative, spiral-shaped, motile , urease positive bacteria.
- Factors help in penetration and growth of Helicobacter pylori are :[9][10]
- Bicarbonate-mediated chemotactic motility of Helicobacter pylori facilitates its penetration
- Neutral pH favors the growth of helicobacter pylori.
Immunological response
Factors responsible for immunological response of Helicobacter pylori are :
- Helicobacter pylori infection triggers local production various proinflammatory mediators (cytokines, neutrophil infiltration, specific T- and B- cells).
- Of all the cytotoxins and virulence factors Cag A, VacA, and OipA play a key role in the pathogenesis of Helicobacter pylori infection.
- Cag A, VacA, and OipA not only helps in the colonization of Helicobacter pylori but and also modulates host's immune system.
- Bacterial factors and complement activation leads to neutrophilic activation including reactive oxygen,release of leukocytes enzymes and leukotriens lead to mucosal injury [11] [12][13][14][7]
- Helicobacter pylori secretes various enzyme :Urease,Phospholipases,Alcohol dehydrogenase and Catalases- causes damage the host gastric muscosa by generating toxic metabolities[15][16][17]
| Helicobacter pylori infection | |||||||||||||||||||||||||||||||||||||
| Inflammatory response secretes IL-8 ,IL-1b | Production of alkaline ammonia | Production of urease bacterial phospholipase A | |||||||||||||||||||||||||||||||||||
| Infux of neutophils and macrophages release of lysosomal enzymes leukotrienes (LT)and reactive oxygen | inhibition of D-cells leads to inappropriate release of somatostatin and hypergastrinemia | Production of urease ,phospholipase A and C release toxic metabolities | |||||||||||||||||||||||||||||||||||
| Mucosal injury | |||||||||||||||||||||||||||||||||||||
Role of Helicobacter pylori in causing gastric ulcer
- Colonzation:
- The colonization of virulent CagA-positive H. pylori strains leads to the degeneration of surface epithelial cells.
- This degeneration results in increased exfoliation of surface epithelial cells.
- The exfoliation mediated compensatory cell proliferation leads to the movement of immature cells to the foveolae and surface.
- Immature cells leads to impaired mucin and bicarbonate production and the integrity of the mucous barrier may be compromised.
- All of above factors lead to activation of complement via the alternative pathway and the release of chemical mediators by mast cells and activated polymorphs may lead to microvascular disturbances and focal ischemic damage to the surface epithelium
- H. pylori infection down-regulates E-cadherin expression in gastric epithelial cells which affect the resistance of the mucosa to acid attack
- Decreased mucus production, release of chemical mediators and down-regulation of E- cadherin leads to mucosal damage leads to ulcer formation[18][19][20]
Role of Helicobacter pylori in causing duodenal ulcer
- Factors responsible for ulcer formation:
Role of NSAIDS
- NSAID's are more commonly responsible for gasrtic ulcers than duodenal ulcers
- NSAID's inhibit systemic prostaglandins production and cause ulcers[26]
- Inhibition of prostaglandins results in decreased blood flow and decreased mucus production resulting in mucosal damage.[27][28]
| NSAIDs | |||||||||||||||||||||||||||||||||||||
| COX-1 inhibitor | Topical irritation | COX-2 inhibitor | |||||||||||||||||||||||||||||||||||
| Decreased blood flow | Epithelial damage | Leucocyte adhesion | |||||||||||||||||||||||||||||||||||
| Mucosal injury | |||||||||||||||||||||||||||||||||||||
Other factors
Other factors responsible for peptic ulcer disease:
Smoking
- Smoking decreases the production of prostaglandins in fundic and antral part of stomach and results in mucosal damage similar to NSAID's[29]
- Smoking is also triggers reflux of bile acids into the duodenum which results in alteration of blood flow leading to ischaemia .[30]
Severe stress
- Severe stress eg: brain injury, burns causes increase in production of gastric acid and increases the risk of ulcer formation
Genetics
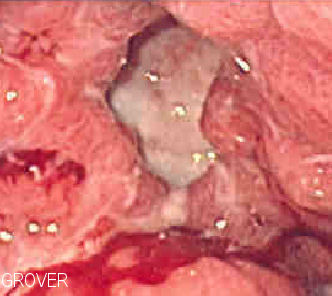
Gross Pathology
- Gastric ulcers are most often localized on the lesser curvature of the stomach.
- Duodenal ulcers are more located at bulb of duodenum.
- Characteristic findings of a peptic ulcer on gross pathology include:
- Round to oval
- 2 to 4 cm diameter
- Smooth base with perpendicular borders.
- Parietal scarring with radial folds may be evident in the surrounding mucosa.


Microscopic Pathology
- A peptic ulcer is a mucosal defect produced by acid-pepsin aggression which penetrates the muscularis mucosae and muscularis propria
- There is increased plasma cells, neutrophilic infiltrate, villous blunting
- The surface epithelium usually shows mucous cell (pseudopyloric) metaplasia
- During the active phase, the base of the ulcer shows 4 zones:
- Inflammatory exudate: polymorphonuclear infiltration which along with bacterial products stimulate the production of IL 8 and tumor necrosis factor alpha (TNF-α) and IL-1 released by macrophages in response to bacterial lipopolysaccharide
- Fibrinoid necrosis
- Granulation tissue
- Fibrous tissue. The fibrous base of the ulcer may contain vessels with thickened wall or with thrombosis.[33]
References
- ↑ Butler BD, Lichtenberger LM |title=Gastric mucosal barrier: hydrophobic lining to the lumen of the stomach |journal=Am. J. Physiol. |volume=244 |issue=5 |pages=G561–8 |year=1983 |pmid=6846549 |doi= |url=}}
- ↑ Clamp JR, Ene D (1989). "The gastric mucosal barrier". Methods Find Exp Clin Pharmacol. 11 Suppl 1: 19–25. PMID 2657286.
- ↑ Werther JL (2000). "The gastric mucosal barrier". Mt. Sinai J. Med. 67 (1): 41–53. PMID 10677782.
- ↑ Forssell H (1988). "Gastric mucosal defence mechanisms: a brief review". Scand. J. Gastroenterol. Suppl. 155: 23–8. PMID 3072665.
- ↑ By M•Komorniczak(http://creativecommons.org/licenses/by/3.0)
- ↑ url=http://www.nejm.org/doi/full/10.1056/NEJM199003293221307 |title=Pathogenesis of Peptic Ulcer and Implications for Therapy — NEJM |format= |work= |accessdate=}}
- ↑ 7.0 7.1 "Pathogenesis of Peptic Ulcer and Implications for Therapy — NEJM".
- ↑ Hawkey CJ (1999). "Personal review: Helicobacter pylori, NSAIDs and cognitive dissonance". Aliment. Pharmacol. Ther. 13 (6): 695–702. PMID 10383497.
- ↑ Kusters JG, van Vliet AH, Kuipers EJ (2006). "Pathogenesis of Helicobacter pylori infection". Clin. Microbiol. Rev. 19 (3): 449–90. doi:10.1128/CMR.00054-05. PMC 1539101. PMID 16847081.
- ↑ Huang JQ, Sridhar S, Hunt RH (2002). "Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: a meta-analysis". Lancet. 359 (9300): 14–22. doi:10.1016/S0140-6736(02)07273-2. PMID 11809181.
- ↑ url=http://www.nejm.org/doi/full/10.1056/NEJM199003293221307 |title=Pathogenesis of Peptic Ulcer and Implications for Therapy — NEJM |format= |work= |accessdate=}}
- ↑ Logan RP (1996). "Adherence of Helicobacter pylori". Aliment. Pharmacol. Ther. 10 Suppl 1: 3–15. PMID 8730255.
- ↑ Crabtree JE (1996). "Gastric mucosal inflammatory responses to Helicobacter pylori". Aliment. Pharmacol. Ther. 10 Suppl 1: 29–37. PMID 8730257.
- ↑ Ernst PB, Jin Y, Reyes VE, Crowe SE (1994). "The role of the local immune response in the pathogenesis of peptic ulcer formation". Scand. J. Gastroenterol. Suppl. 205: 22–8. PMID 7863238.
- ↑ Mobley HL (1996). "The role of Helicobacter pylori urease in the pathogenesis of gastritis and peptic ulceration". Aliment. Pharmacol. Ther. 10 Suppl 1: 57–64. PMID 8730260.
- ↑ Nilius M, Malfertheiner P (1996). "Helicobacter pylori enzymes". Aliment. Pharmacol. Ther. 10 Suppl 1: 65–71. PMID 8730261.
- ↑ Slomiany BL, Kasinathan C, Slomiany A (1989). "Lipolytic activity of Campylobacter pylori: effect of colloidal bismuth subcitrate (De-Nol)". Am. J. Gastroenterol. 84 (10): 1273–7. PMID 2801678.
- ↑ Kim JS, Jung HC, Kim JM, Song IS, Kim CY (1998). "Interleukin-8 expression by human neutrophils activated by Helicobacter pylori soluble proteins". Scand. J. Gastroenterol. 33 (12): 1249–55. PMID 9930387.
- ↑ Kimura K (1972). "Chronological transition of the fundic-pyloric border determined by stepwise biopsy of the lesser and greater curvatures of the stomach". Gastroenterology. 63 (4): 584–92. PMID 5077145.
- ↑ Malaty HM, Graham DY, Isaksson I, Engstrand L, Pedersen NL (2000). "Are genetic influences on peptic ulcer dependent or independent of genetic influences for Helicobacter pylori infection?". Arch. Intern. Med. 160 (1): 105–9. PMID 10632311.
- ↑ Wyatt JI, Rathbone BJ, Dixon MF, Heatley RV (1987). "Campylobacter pyloridis and acid induced gastric metaplasia in the pathogenesis of duodenitis". J. Clin. Pathol. 40 (8): 841–8. PMC 1141122. PMID 3654985.
- ↑ el-Omar EM, Penman ID, Ardill JE, Chittajallu RS, Howie C, McColl KE (1995). "Helicobacter pylori infection and abnormalities of acid secretion in patients with duodenal ulcer disease". Gastroenterology. 109 (3): 681–91. PMID 7657096.
- ↑ el-Omar E, Penman I, Dorrian CA, Ardill JE, McColl KE (1993). "Eradicating Helicobacter pylori infection lowers gastrin mediated acid secretion by two thirds in patients with duodenal ulcer". Gut. 34 (8): 1060–5. PMC 1374354. PMID 8174954.
- ↑ el-Omar EM, Penman ID, Ardill JE, Chittajallu RS, Howie C, McColl KE (1995). "Helicobacter pylori infection and abnormalities of acid secretion in patients with duodenal ulcer disease". Gastroenterology. 109 (3): 681–91. PMID 7657096.
- ↑ el-Omar E, Penman I, Dorrian CA, Ardill JE, McColl KE (1993). "Eradicating Helicobacter pylori infection lowers gastrin mediated acid secretion by two thirds in patients with duodenal ulcer". Gut. 34 (8): 1060–5. PMC 1374354. PMID 8174954.
- ↑ Borody TJ, George LL, Brandl S, Andrews P, Ostapowicz N, Hyland L, Devine M (1991). "Helicobacter pylori-negative duodenal ulcer". Am. J. Gastroenterol. 86 (9): 1154–7. PMID 1882793.
- ↑ Huang JQ, Sridhar S, Hunt RH (2002). "Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: a meta-analysis". Lancet. 359 (9300): 14–22. doi:10.1016/S0140-6736(02)07273-2. PMID 11809181.
- ↑ Holvoet J, Terriere L, Van Hee W, Verbist L, Fierens E, Hautekeete ML (1991). "Relation of upper gastrointestinal bleeding to non-steroidal anti-inflammatory drugs and aspirin: a case-control study". Gut. 32 (7): 730–4. PMC 1378985. PMID 1855677.
- ↑ Quimby GF, Bonnice CA, Burstein SH, Eastwood GL (1986). "Active smoking depresses prostaglandin synthesis in human gastric mucosa". Ann. Intern. Med. 104 (5): 616–9. PMID 3457547.
- ↑ Müller-Lissner SA (1986). "Bile reflux is increased in cigarette smokers". Gastroenterology. 90 (5 Pt 1): 1205–9. PMID 3956939.
- ↑ Räihä I, Kemppainen H, Kaprio J, Koskenvuo M, Sourander L (1998). "Lifestyle, stress, and genes in peptic ulcer disease: a nationwide twin cohort study". Arch. Intern. Med. 158 (7): 698–704. PMID 9554675.
- ↑ FakhreYaseri H, Shakaraby M, Bradaran HR, Soltani Arabshahi SK, Fakhre Yaseri AM (2014). "CagA and VacA genotypes in peptic ulcer disease and non-ulcer dyspepsia: a case-control study". Med J Islam Repub Iran. 28: 104. PMC 4301206. PMID 25664305.
- ↑ "ATLAS OF PATHOLOGY". Retrieved 2007-08-26.