Pancreatic trauma
| Pancreatic trauma |
|
WikiDoc Resources for Pancreatic trauma |
|
Articles |
|---|
|
Most recent articles on Pancreatic trauma Most cited articles on Pancreatic trauma |
|
Media |
|
Powerpoint slides on Pancreatic trauma |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Pancreatic trauma |
|
Clinical Trials |
|
Ongoing Trials on Pancreatic trauma at Clinical Trials.gov Trial results on Pancreatic trauma Clinical Trials on Pancreatic trauma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Pancreatic trauma NICE Guidance on Pancreatic trauma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Pancreatic trauma Discussion groups on Pancreatic trauma Patient Handouts on Pancreatic trauma Directions to Hospitals Treating Pancreatic trauma Risk calculators and risk factors for Pancreatic trauma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Pancreatic trauma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Contributors: Cafer Zorkun M.D., PhD.
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
- In the acute setting, pancreatic injuries may result in death due to associated vascular injuries.
- Delayed morbidity and mortality are usually caused by complications resulting from disruption of the pancreatic duct.
- Duct injury may lead to complications such as abscess, pancreatic pseudocyst, fistula, and pancreatitis.
- The pancreas is vulnerable to crushing injury in blunt trauma due to impact against the adjacent vertebral column.
- Two-thirds of pancreatic injuries occur in the pancreatic body, and the remainder occur equally in the head, neck, and tail.
- Isolated pancreatic injuries are rare, and associated injuries, especially to the liver, stomach, duodenum, and spleen, occur in over 90% of cases.
- In adults, over 75% of blunt injuries to the pancreas are due to motor vehicle collisions.
- In children, bicycle injuries are common, and child abuse may result in pancreatic injuries in infants.
Diagnosis
- Pancreatic injuries may be difficult to diagnose clinically.
Diagnostic Findings
CT
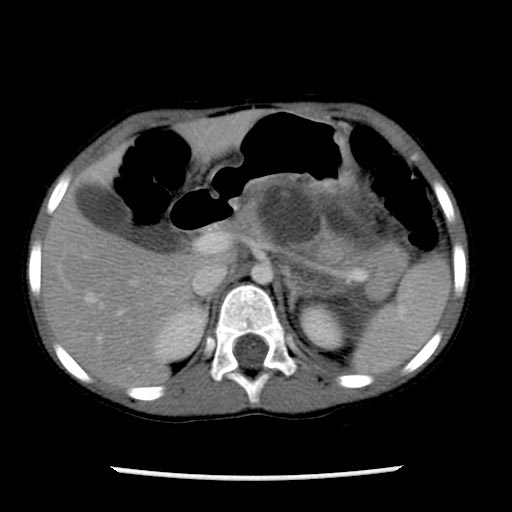
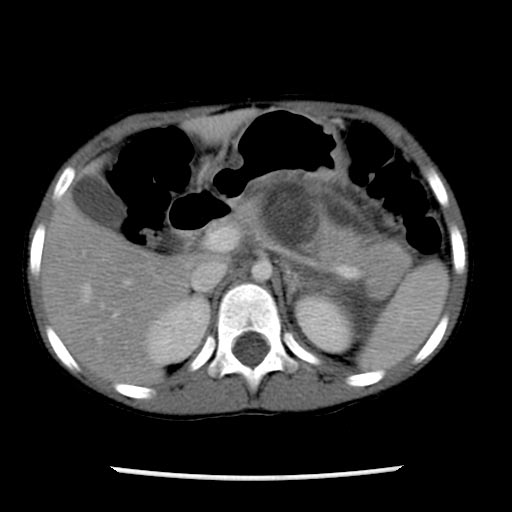
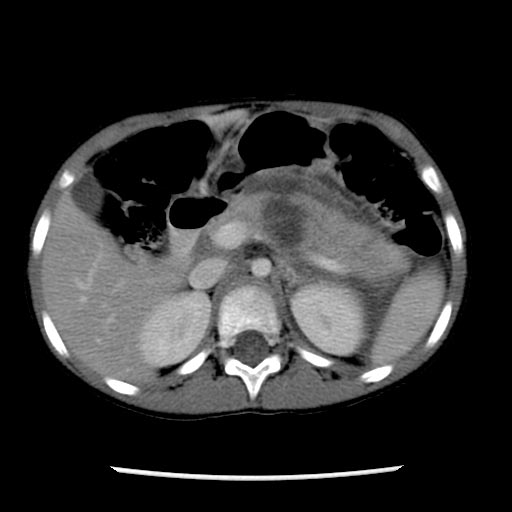
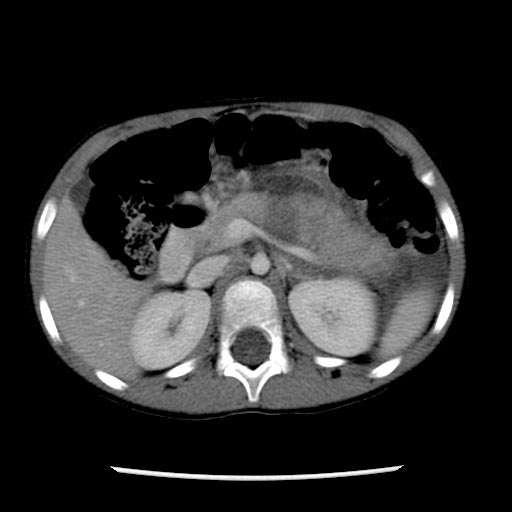
- Direct signs of pancreatic injury include pancreatic laceration, transection, and comminution. [1]
- Fluid collections, such as hematomas, pseudocysts, and abscesses, are often seen communicating with the pancreas at the site of fracture or transection.
- Focal enlargement of the pancreas and peripancreatic fluid are suggestive of pancreatic injury.
- Peripancreatic fat stranding, hemorrhage, and fluid between the splenic vein and pancreas are useful secondary signs.
-
A patient with pancreatic transection and pseudocyst formation from motor vehicle accident
-
-
-
-
-
Treatment
Disruption of the pancreatic duct is treated surgically or by therapeutic endoscopy with stent placement, while injuries without duct involvement are usually treated nonsurgically.
Prognosis
- Although uncommon, early diagnosis is crucial, since delayed complications such as fistula, abscess, sepsis, and hemorrhage may lead to significant mortality, occurring in up to 20% of cases.
- Death due to delayed complications is usually due to sepsis and multiorgan failure.
- The main source of delayed morbidity and mortality from pancreatic trauma is disruption of the pancreatic duct. Injuries that spare the pancreatic duct rarely result in morbidity or death.
References
- ↑ Avneesh Gupta, Joshua W. Stuhlfaut, Keith W. Fleming, Brian C. Lucey, and Jorge A. Soto. Blunt Trauma of the Pancreas and Biliary Tract: A Multimodality Imaging Approach to Diagnosis. RadioGraphics 2004 24: 1381-1395.
External Links
Template:Skin and subcutaneous tissue symptoms and signs Template:Nervous and musculoskeletal system symptoms and signs Template:Urinary system symptoms and signs Template:Cognition, perception, emotional state and behaviour symptoms and signs Template:Speech and voice symptoms and signs Template:General symptoms and signs