Pancoast tumor other diagnostic studies
|
Pancoast tumor Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pancoast tumor other diagnostic studies On the Web |
|
American Roentgen Ray Society Images of Pancoast tumor other diagnostic studies |
|
Risk calculators and risk factors for Pancoast tumor other diagnostic studies |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Mazia Fatima, MBBS [2]
Overveiw
Other diagnostic studies for evaluating the spread of pancoast tumor include bone scintigraphy, PET scan, and molecular tests.
Other Diagnostic Studies
Bone Scintigraphy
A bone scan may demonstrate bone metastases.
PET scan
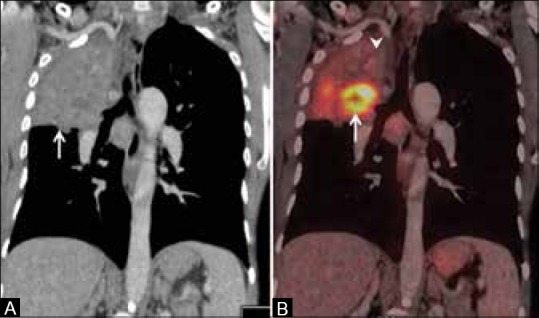
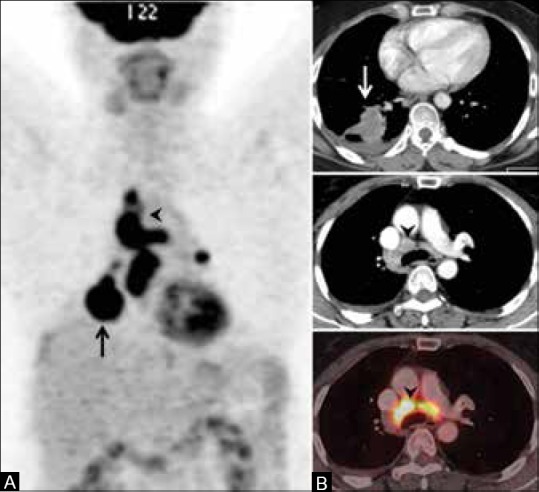
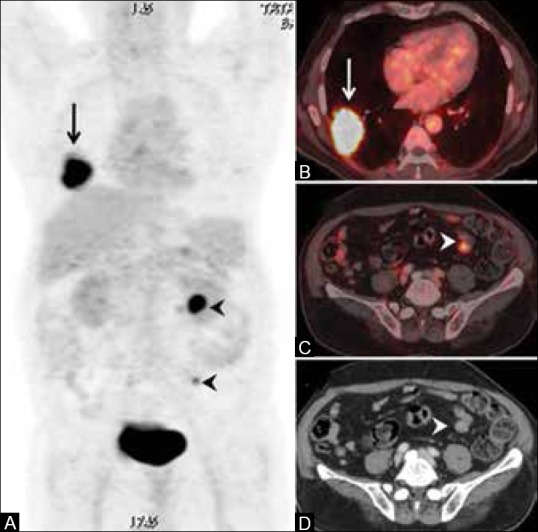
- FDG(18 F fluoro deoxyglucose) PET scans along with contrast enhanced CT may be helpful in the diagnosis of extent of lung cancer. Findings on FDGPET/CT suggestive of lung cancer include:[1]
- Solitary pulmonary nodule
- Benefits of FDGPET/CT include:[2]
- Accurate delineation of the viable tumor from surrounding atelectasis and collapse or consolidation.
- It may further lead to a change in staging and treatment options of the lung cancer.
- Provide guidance for the biopsy.[3]
 |
 |
 |
Molecular Test
Molecular tests include epidermal growth factor receptor (EGFR) mutation and anaplastic lymphoma kinase (ALK) mutation. Specific targeted agents may be administered to patients if these mutations are present.
References
- ↑ 1.0 1.1 1.2 Purandare, NilenduC; Rangarajan, Venkatesh (2015). "Imaging of lung cancer: Implications on staging and management". Indian Journal of Radiology and Imaging. 25 (2): 109. doi:10.4103/0971-3026.155831. ISSN 0971-3026.
- ↑ van Baardwijk, Angela; Baumert, Brigitta G.; Bosmans, Geert; van Kroonenburgh, Marinus; Stroobants, Sigrid; Gregoire, Vincent; Lambin, Philippe; De Ruysscher, Dirk (2006). "The current status of FDG–PET in tumour volume definition in radiotherapy treatment planning". Cancer Treatment Reviews. 32 (4): 245–260. doi:10.1016/j.ctrv.2006.02.002. ISSN 0305-7372.
- ↑ Purandare, Nilendu C.; Kulkarni, Aniruddha V.; Kulkarni, Suyash S.; Roy, Diptiman; Agrawal, Archi; Shah, Sneha; Rangarajan, Venkatesh (2013). "18F-FDG PET/CT-directed biopsy". Nuclear Medicine Communications. 34 (3): 203–210. doi:10.1097/MNM.0b013e32835c5a57. ISSN 0143-3636.
- ↑ Purandare, NilenduC; Rangarajan, Venkatesh (2015). "Imaging of lung cancer: Implications on staging and management". Indian Journal of Radiology and Imaging. 25 (2): 109. doi:10.4103/0971-3026.155831. ISSN 0971-3026.