Ondansetron (injection): Difference between revisions
No edit summary |
No edit summary |
||
| Line 82: | Line 82: | ||
Pediatric Use: Rates of adverse reactions were similar in both the ondansetron and placebo groups in pediatric patients receiving ondansetron (a single 0.1-mg/kg dose for pediatric patients weighing 40 kg or less, or 4 mg for pediatric patients weighing more than 40 kg) administered intravenously over at least 30 seconds. Diarrhea was seen more frequently in patients taking Ondansetron (2%) compared to placebo (<1%) in the 1 month to 24 month age group. These patients were receiving multiple concomitant perioperative and postoperative medications. | Pediatric Use: Rates of adverse reactions were similar in both the ondansetron and placebo groups in pediatric patients receiving ondansetron (a single 0.1-mg/kg dose for pediatric patients weighing 40 kg or less, or 4 mg for pediatric patients weighing more than 40 kg) administered intravenously over at least 30 seconds. Diarrhea was seen more frequently in patients taking Ondansetron (2%) compared to placebo (<1%) in the 1 month to 24 month age group. These patients were receiving multiple concomitant perioperative and postoperative medications. | ||
|postmarketing=The following adverse reactions have been identified during post-approval use of ondansetron. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The reactions have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to ondansetron. | |postmarketing=The following adverse reactions have been identified during post-approval use of ondansetron. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The reactions have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to ondansetron. | ||
| Line 101: | Line 99: | ||
Eye Disorders: Cases of transient blindness, predominantly during intravenous administration, have been reported. These cases of transient blindness were reported to resolve within a few minutes up to 48 hours. Transient blurred vision, in some cases associated with abnormalities of accommodation, have also been reported. | Eye Disorders: Cases of transient blindness, predominantly during intravenous administration, have been reported. These cases of transient blindness were reported to resolve within a few minutes up to 48 hours. Transient blurred vision, in some cases associated with abnormalities of accommodation, have also been reported. | ||
|drugInteractions=7.1 Drugs Affecting Cytochrome P-450 Enzymes | |||
Ondansetron does not appear to induce or inhibit the cytochrome P-450 drug-metabolizing enzyme system of the liver. Because ondansetron is metabolized by hepatic cytochrome P-450 drug-metabolizing enzymes (CYP3A4, CYP2D6, CYP1A2), inducers or inhibitors of these enzymes may change the clearance and, hence, the half-life of ondansetron [see Clinical Pharmacology (12.3)]. On the basis of limited available data, no dosage adjustment is recommended for patients on these drugs. | |||
7.2 Apomorphine | |||
Based on reports of profound hypotension and loss of consciousness when apomorphine was administered with ondansetron, concomitant use of apomorphine with ondansetron is contraindicated [see Contraindications (4)]. | |||
7.3 Phenytoin, Carbamazepine, and Rifampin | |||
In patients treated with potent inducers of CYP3A4 (i.e., phenytoin, carbamazepine, and rifampin), the clearance of ondansetron was significantly increased and ondansetron blood concentrations were decreased. However, on the basis of available data, no dosage adjustment for ondansetron is recommended for patients on these drugs [see Clinical Pharmacology (12.3)]. | |||
7.4 Tramadol | |||
Although there are no data on pharmacokinetic drug interactions between ondansetron and tramadol, data from two small studies indicate that concomitant use of ondansetron may result in reduced analgesic activity of tramadol. Patients on concomitant ondansetron self administered tramadol more frequently in these studies, leading to an increased cumulative dose in patient controlled administration (PCA) of tramadol. | |||
7.5 Serotonergic Drugs | |||
Serotonin syndrome (including altered mental status, autonomic instability, and neuromuscular symptoms) has been described following the concomitant use of 5-HT3 receptor antagonists and other serotonergic drugs, including selective serotonin reuptake inhibitors (SSRIs) and serotonin and noradrenaline reuptake inhibitors (SNRIs) [see Warnings and Precautions (5.3)]. | |||
7.6 Chemotherapy | |||
In humans, carmustine, etoposide, and cisplatin do not affect the pharmacokinetics of ondansetron. | |||
In a crossover study in 76 pediatric patients, intravenous ondansetron did not increase blood levels of high-dose methotrexate. | |||
7.7 Temazepam | |||
The coadministration of ondansetron had no effect on the pharmacokinetics and pharmacodynamics of temazepam. | |||
7.8 Alfentanil and Atracurium | |||
Ondansetron does not alter the respiratory depressant effects produced by alfentanil or the degree of neuromuscular blockade produced by atracurium. Interactions with general or local anesthetics have not been studied. | |||
|FDAPregCat=B | |||
|useInPregnancyFDA=Reproduction studies have been performed in pregnant rats and rabbits at intravenous doses up to 4 mg/kg per day (approximately 1.4 and 2.9 times the recommended human intravenous dose of 0.15 mg/kg given three times a day, respectively, based on body surface area) and have revealed no evidence of impaired fertility or harm to the fetus due to ondansetron. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed. | |||
|useInNursing=Ondansetron is excreted in the breast milk of rats. It is not known whether ondansetron is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when ondansetron is administered to a nursing woman. | |||
|useInPed=Little information is available about the use of ondansetron in pediatric surgical patients younger than 1 month of age. [See Clinical Studies (14.2)]. Little information is available about the use of ondansetron in pediatric cancer patients younger than 6 months of age. [See Clinical Studies (14.1), Dosage and Administration (2)]. | |||
The clearance of ondansetron in pediatric patients 1 month to 4 months of age is slower and the half-life is ~2.5 fold longer than patients who are > 4 to 24 months of age. As a precaution, it is recommended that patients less than 4 months of age receiving this drug be closely monitored. [See Clinical Pharmacology (12.3)]. | |||
Ondansetron Prefilled Syringe: REQUIRES NO DILUTION FOR ADMINISTRATION FOR POSTOPERATIVE NAUSEA AND VOMITING. CAUTION: For pediatric patients less than 40 kg, a full 4 mg dose should NOT be given [see Dosage and Administration (2.2)]. | |||
|useInGeri=Of the total number of subjects enrolled in cancer chemotherapy-induced and postoperative nausea and vomiting in US- and foreign-controlled clinical trials, 862 were 65 years of age and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Dosage adjustment is not needed in patients over the age of 65. | |||
|useInRenalImpair=Although plasma clearance is reduced in patients with severe renal impairment (creatinine clearance < 30 mL/min), no dosage adjustment is recommended [see Clinical Pharmacology (12.3)]. | |||
|useInHepaticImpair=In patients with severe hepatic impairment (Child-Pugh score of 10 or greater), clearance is reduced and apparent volume of distribution is increased with a resultant increase in plasma half-life [see Clinical Pharmacology (12.3)]. In such patients, a total daily dose of 8 mg should not be exceeded. | |||
|overdose=There is no specific antidote for ondansetron overdose. Patients should be managed with appropriate supportive therapy. Individual intravenous doses as large as 150 mg and total daily intravenous doses as large as 252 mg have been inadvertently administered without significant adverse events. These doses are more than 10 times the recommended daily dose. | |||
In addition to the adverse reactions listed above, the following events have been described in the setting of ondansetron overdose: “Sudden blindness” (amaurosis) of 2 to 3 minutes' duration plus severe constipation occurred in one patient that was administered 72 mg of ondansetron intravenously as a single dose. Hypotension (and faintness) occurred in another patient that took 48 mg of ondansetron hydrochloride tablets. Following infusion of 32 mg over only a 4-minute period, a vasovagal episode with transient second-degree heart block was observed. In all instances, the events resolved completely. | |||
Pediatric cases consistent with serotonin syndrome have been reported after inadvertent oral overdoses of ondansetron (exceeding estimated ingestion of 5 mg/kg) in young children. Reported symptoms included somnolence, agitation, tachycardia, tachypnea, hypertension, flushing, mydriasis, diaphoresis, myoclonic movements, horizontal nystagmus, hyperreflexia, and seizure. Patients required supportive care, including intubation in some cases, with complete recovery without sequelae within 1 to 2 days. | |||
|alcohol=Alcohol-Ondansetron (injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |alcohol=Alcohol-Ondansetron (injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
}} | }} | ||
Revision as of 14:23, 19 May 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Turky Alkathery, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Ondansetron (injection) is a 5-HT3 receptor antagonist that is FDA approved for the prevention of nausea and vomiting associated with initial and repeat courses of emetogenic cancer chemotherapy. Common adverse reactions include diarrhea, headache, and fever.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
1.1 Prevention of Nausea and Vomiting Associated with Initial and Repeat Courses of Emetogenic Cancer Chemotherapy Ondansetron Injection is indicated for the prevention of nausea and vomiting associated with initial and repeat courses of emetogenic cancer chemotherapy, including high-dose cisplatin [see Clinical Studies (14.1)]. 1.2 Prevention of Postoperative Nausea and Vomiting Ondansetron Injection is indicated for the prevention of postoperative nausea and/or vomiting. As with other antiemetics, routine prophylaxis is not recommended for patients in whom there is little expectation that nausea and/or vomiting will occur postoperatively. In patients in whom nausea and/or vomiting must be avoided postoperatively, Ondansetron Injection is recommended even when the incidence of postoperative nausea and/or vomiting is low. For patients who do not receive prophylactic Ondansetron Injection and experience nausea and/or vomiting postoperatively, Ondansetron Injection may be given to prevent further episodes [see Clinical Studies (14.3)].
Dosage
2.1 Prevention of Nausea and Vomiting Associated with Initial and Repeat Courses of Emetogenic Chemotherapy Ondansetron Injection should be diluted in 50 mL of 5% Dextrose Injection or 0.9% Sodium Chloride Injection before administration.
2.2 Prevention of Postoperative Nausea and Vomiting Ondansetron Injection should not be mixed with solutions for which physical and chemical compatibility have not been established. In particular, this applies to alkaline solutions as a precipitate may form.
Adults: The recommended adult intravenous dosage of Ondansetron is 4 mg undiluted administered intravenously in not less than 30 seconds, preferably over 2 to 5 minutes, immediately before induction of anesthesia, or postoperatively if the patient did not receive prophylactic antiemetics and experiences nausea and/or vomiting occurring within 2 hours after surgery. Alternatively, 4 mg undiluted may be administered intramuscularly as a single injection for adults. While recommended as a fixed dose for patients weighing more than 40 kg, few patients above 80 kg have been studied. In patients who do not achieve adequate control of postoperative nausea and vomiting following a single, prophylactic, preinduction, intravenous dose of ondansetron 4 mg, administration of a second intravenous dose of 4 mg ondansetron postoperatively does not provide additional control of nausea and vomiting.
Adults: The recommended adult intravenous dosage of Ondansetron is three 0.15-mg/kg doses up to a maximum of 16 mg per dose [see Clinical Pharmacology (12.2)]. The first dose is infused over 15 minutes beginning 30 minutes before the start of emetogenic chemotherapy. Subsequent doses (0.15 mg/kg up to a maximum of 16 mg per dose) are administered 4 and 8 hours after the first dose of Ondansetron.
2.3 Stability and Handling After dilution, do not use beyond 24 hours. Although Ondansetron Injection, USP is chemically and physically stable when diluted as recommended, sterile precautions should be observed because diluents generally do not contain preservative.
Ondansetron Injection, USP is stable at room temperature under normal lighting conditions for 48 hours after dilution with the following intravenous fluids: 0.9% Sodium Chloride Injection, 5% Dextrose Injection, 5% Dextrose and 0.9% Sodium Chloride Injection, 5% Dextrose and 0.45% Sodium Chloride Injection, and 3% Sodium Chloride Injection.
Note: Parenteral drug products should be inspected visually for particulate matter and discoloration before administration whenever solution and container permit.
2.4 Dosage Adjustment for Patients with Impaired Hepatic Function In patients with severe hepatic impairment (Child-Pugh score of 10 or greater), a single maximal daily dose of 8 mg infused over 15 minutes beginning 30 minutes before the start of the emetogenic chemotherapy is recommended. There is no experience beyond first-day administration of ondansetron in these patients.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Ondansetron (injection) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Ondansetron (injection) FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Ondansetron (injection) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Ondansetron (injection) in pediatric patients.
Contraindications
Ondansetron Injection, USP is contraindicated for patients known to have hypersensitivity (e.g., anaphylaxis) to this product or any of its components. Anaphylactic reactions have been reported in patients taking ondansetron. [See Adverse Reactions (6.2)].
The concomitant use of apomorphine with ondansetron is contraindicated based on reports of profound hypotension and loss of consciousness when apomorphine was administered with ondansetron.
Warnings
5.1 Hypersensitivity Reactions Hypersensitivity reactions, including anaphylaxis and bronchospasm, have been reported in patients who have exhibited hypersensitivity to other selective 5-HT3 receptor antagonists.
5.2 QT Prolongation Ondansetron prolongs the QT interval in a dose-dependent manner [see Clinical Pharmacology (12.2)]. In addition, post-marketing cases of Torsade de Pointes have been reported in patients using ondansetron. Avoid Ondansetron in patients with congenital long QT syndrome. ECG monitoring is recommended in patients with electrolyte abnormalities (e.g., hypokalemia or hypomagnesemia), congestive heart failure, bradyarrhythmias, or patients taking other medicinal products that lead to QT prolongation.
5.3 Serotonin Syndrome The development of serotonin syndrome has been reported with 5-HT3 receptor antagonists. Most reports have been associated with concomitant use of serotonergic drugs (e.g., selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors, mirtazapine, fentanyl, lithium, tramadol, and intravenous methylene blue). Some of the reported cases were fatal. Serotonin syndrome occurring with overdose of Ondansetron alone has also been reported. The majority of reports of serotonin syndrome related to 5-HT3 receptor antagonist use occurred in a post-anesthesia care unit or an infusion center.
Symptoms associated with serotonin syndrome may include the following combination of signs and symptoms: mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, with or without gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be monitored for the emergence of serotonin syndrome, especially with concomitant use of Ondansetron and other serotonergic drugs. If symptoms of serotonin syndrome occur, discontinue Ondansetron and initiate supportive treatment. Patients should be informed of the increased risk of serotonin syndrome, especially if Ondansetron is used concomitantly with other serotonergic drugs [see Drug Interactions (7.5), Overdosage (10), Patient Counseling Information (17)].
5.4 Masking of Progressive Ileus and Gastric Distension The use of Ondansetron in patients following abdominal surgery or in patients with chemotherapy-induced nausea and vomiting may mask a progressive ileus and gastric distention.
5.5 Effect on Peristalsis Ondansetron is not a drug that stimulates gastric or intestinal peristalsis. It should not be used instead of nasogastric suction.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
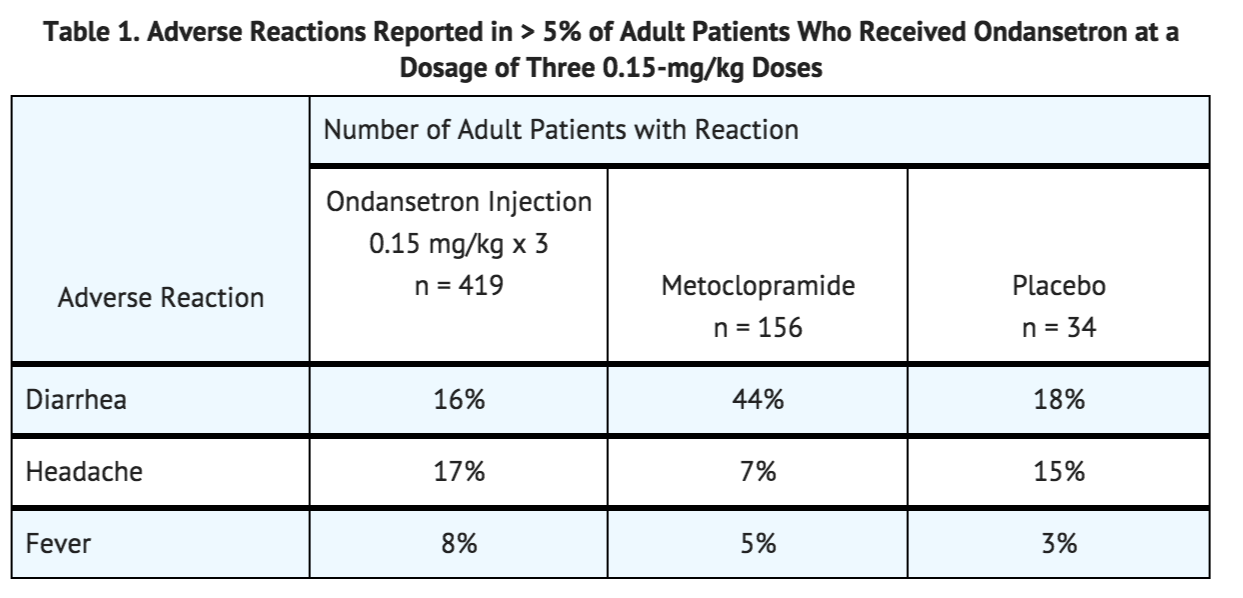
The following adverse reactions have been reported in clinical trials of adult patients treated with ondansetron, the active ingredient of intravenous Ondansetron across a range of dosages. A causal relationship to therapy with Ondansetron was unclear in many cases.
Chemotherapy-Induced Nausea and Vomiting:
Cardiovascular: Rare cases of angina (chest pain), electrocardiographic alterations, hypotension, and tachycardia have been reported.
Gastrointestinal: Constipation has been reported in 11% of chemotherapy patients receiving multiday ondansetron.
Hepatic: In comparative trials in cisplatin chemotherapy patients with normal baseline values of aspartate transaminase (AST) and alanine transaminase (ALT), these enzymes have been reported to exceed twice the upper limit of normal in approximately 5% of patients. The increases were transient and did not appear to be related to dose or duration of therapy. On repeat exposure, similar transient elevations in transaminase values occurred in some courses, but symptomatic hepatic disease did not occur.
Integumentary: Rash has occurred in approximately 1% of patients receiving ondansetron.
Neurological: There have been rare reports consistent with, but not diagnostic of, extrapyramidal reactions in patients receiving Ondansetron injection, and rare cases of grand mal seizure.
Other: Rare cases of hypokalemia have been reported.
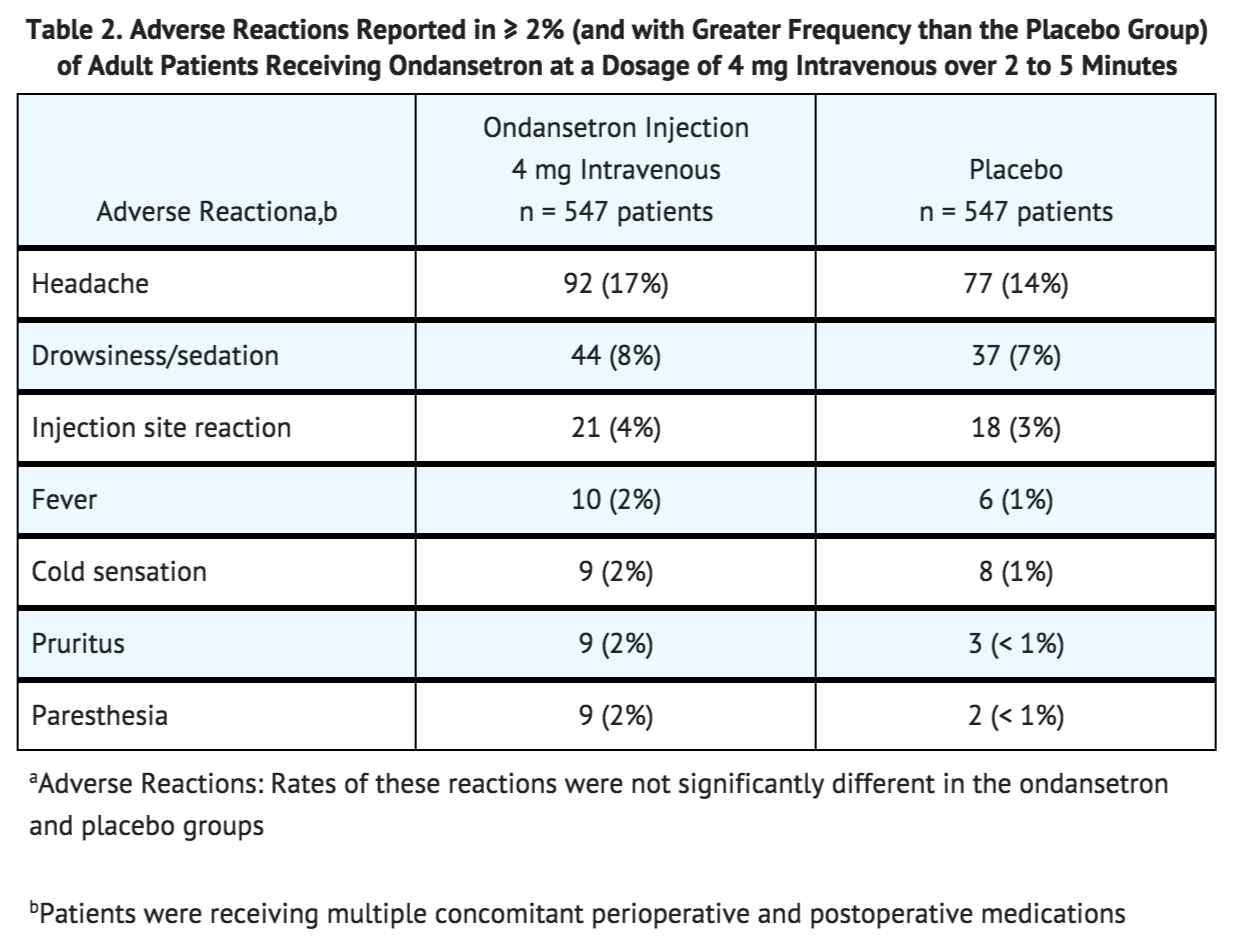
Postoperative Nausea and Vomiting: The adverse reactions in TABLE 2 have been reported in ≥ 2% of adults receiving ondansetron at a dosage of 4 mg intravenous over 2 to 5 minutes in clinical trials.
Pediatric Use: Rates of adverse reactions were similar in both the ondansetron and placebo groups in pediatric patients receiving ondansetron (a single 0.1-mg/kg dose for pediatric patients weighing 40 kg or less, or 4 mg for pediatric patients weighing more than 40 kg) administered intravenously over at least 30 seconds. Diarrhea was seen more frequently in patients taking Ondansetron (2%) compared to placebo (<1%) in the 1 month to 24 month age group. These patients were receiving multiple concomitant perioperative and postoperative medications.
Postmarketing Experience
The following adverse reactions have been identified during post-approval use of ondansetron. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The reactions have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to ondansetron.
Cardiovascular: Arrhythmias (including ventricular and supraventricular tachycardia, premature ventricular contractions, and atrial fibrillation), bradycardia, electrocardiographic alterations (including second-degree heart block, QT/QTc interval prolongation, and ST segment depression), palpitations, and syncope. Rarely and predominantly with intravenous ondansetron, transient ECG changes including QT/QTc interval prolongation have been reported [see Warnings and Precautions (5.2)].
General: Flushing. Rare cases of hypersensitivity reactions, sometimes severe (e.g., anaphylactic reactions, angioedema, bronchospasm, cardiopulmonary arrest, hypotension, laryngeal edema, laryngospasm, shock, shortness of breath, stridor) have also been reported. A positive lymphocyte transformation test to ondansetron has been reported, which suggests immunologic sensitivity to ondansetron.
Hepatobiliary: Liver enzyme abnormalities have been reported. Liver failure and death have been reported in patients with cancer receiving concurrent medications including potentially hepatotoxic cytotoxic chemotherapy and antibiotics.
Local Reactions: Pain, redness, and burning at site of injection.
Lower Respiratory: Hiccups
Neurological: Oculogyric crisis, appearing alone, as well as with other dystonic reactions. Transient dizziness during or shortly after intravenous infusion.
Skin: Urticaria, Stevens-Johnson syndrome, and toxic epidermal necrolysis.
Eye Disorders: Cases of transient blindness, predominantly during intravenous administration, have been reported. These cases of transient blindness were reported to resolve within a few minutes up to 48 hours. Transient blurred vision, in some cases associated with abnormalities of accommodation, have also been reported.
Drug Interactions
7.1 Drugs Affecting Cytochrome P-450 Enzymes Ondansetron does not appear to induce or inhibit the cytochrome P-450 drug-metabolizing enzyme system of the liver. Because ondansetron is metabolized by hepatic cytochrome P-450 drug-metabolizing enzymes (CYP3A4, CYP2D6, CYP1A2), inducers or inhibitors of these enzymes may change the clearance and, hence, the half-life of ondansetron [see Clinical Pharmacology (12.3)]. On the basis of limited available data, no dosage adjustment is recommended for patients on these drugs.
7.2 Apomorphine Based on reports of profound hypotension and loss of consciousness when apomorphine was administered with ondansetron, concomitant use of apomorphine with ondansetron is contraindicated [see Contraindications (4)].
7.3 Phenytoin, Carbamazepine, and Rifampin In patients treated with potent inducers of CYP3A4 (i.e., phenytoin, carbamazepine, and rifampin), the clearance of ondansetron was significantly increased and ondansetron blood concentrations were decreased. However, on the basis of available data, no dosage adjustment for ondansetron is recommended for patients on these drugs [see Clinical Pharmacology (12.3)].
7.4 Tramadol Although there are no data on pharmacokinetic drug interactions between ondansetron and tramadol, data from two small studies indicate that concomitant use of ondansetron may result in reduced analgesic activity of tramadol. Patients on concomitant ondansetron self administered tramadol more frequently in these studies, leading to an increased cumulative dose in patient controlled administration (PCA) of tramadol.
7.5 Serotonergic Drugs Serotonin syndrome (including altered mental status, autonomic instability, and neuromuscular symptoms) has been described following the concomitant use of 5-HT3 receptor antagonists and other serotonergic drugs, including selective serotonin reuptake inhibitors (SSRIs) and serotonin and noradrenaline reuptake inhibitors (SNRIs) [see Warnings and Precautions (5.3)].
7.6 Chemotherapy In humans, carmustine, etoposide, and cisplatin do not affect the pharmacokinetics of ondansetron.
In a crossover study in 76 pediatric patients, intravenous ondansetron did not increase blood levels of high-dose methotrexate.
7.7 Temazepam The coadministration of ondansetron had no effect on the pharmacokinetics and pharmacodynamics of temazepam.
7.8 Alfentanil and Atracurium Ondansetron does not alter the respiratory depressant effects produced by alfentanil or the degree of neuromuscular blockade produced by atracurium. Interactions with general or local anesthetics have not been studied.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): B
Reproduction studies have been performed in pregnant rats and rabbits at intravenous doses up to 4 mg/kg per day (approximately 1.4 and 2.9 times the recommended human intravenous dose of 0.15 mg/kg given three times a day, respectively, based on body surface area) and have revealed no evidence of impaired fertility or harm to the fetus due to ondansetron. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Ondansetron (injection) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Ondansetron (injection) during labor and delivery.
Nursing Mothers
Ondansetron is excreted in the breast milk of rats. It is not known whether ondansetron is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when ondansetron is administered to a nursing woman.
Pediatric Use
Little information is available about the use of ondansetron in pediatric surgical patients younger than 1 month of age. [See Clinical Studies (14.2)]. Little information is available about the use of ondansetron in pediatric cancer patients younger than 6 months of age. [See Clinical Studies (14.1), Dosage and Administration (2)].
The clearance of ondansetron in pediatric patients 1 month to 4 months of age is slower and the half-life is ~2.5 fold longer than patients who are > 4 to 24 months of age. As a precaution, it is recommended that patients less than 4 months of age receiving this drug be closely monitored. [See Clinical Pharmacology (12.3)].
Ondansetron Prefilled Syringe: REQUIRES NO DILUTION FOR ADMINISTRATION FOR POSTOPERATIVE NAUSEA AND VOMITING. CAUTION: For pediatric patients less than 40 kg, a full 4 mg dose should NOT be given [see Dosage and Administration (2.2)].
Geriatic Use
Of the total number of subjects enrolled in cancer chemotherapy-induced and postoperative nausea and vomiting in US- and foreign-controlled clinical trials, 862 were 65 years of age and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Dosage adjustment is not needed in patients over the age of 65.
Gender
There is no FDA guidance on the use of Ondansetron (injection) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Ondansetron (injection) with respect to specific racial populations.
Renal Impairment
Although plasma clearance is reduced in patients with severe renal impairment (creatinine clearance < 30 mL/min), no dosage adjustment is recommended [see Clinical Pharmacology (12.3)].
Hepatic Impairment
In patients with severe hepatic impairment (Child-Pugh score of 10 or greater), clearance is reduced and apparent volume of distribution is increased with a resultant increase in plasma half-life [see Clinical Pharmacology (12.3)]. In such patients, a total daily dose of 8 mg should not be exceeded.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Ondansetron (injection) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Ondansetron (injection) in patients who are immunocompromised.
Administration and Monitoring
Administration
There is limited information regarding Ondansetron (injection) Administration in the drug label.
Monitoring
There is limited information regarding Ondansetron (injection) Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Ondansetron (injection) and IV administrations.
Overdosage
There is no specific antidote for ondansetron overdose. Patients should be managed with appropriate supportive therapy. Individual intravenous doses as large as 150 mg and total daily intravenous doses as large as 252 mg have been inadvertently administered without significant adverse events. These doses are more than 10 times the recommended daily dose.
In addition to the adverse reactions listed above, the following events have been described in the setting of ondansetron overdose: “Sudden blindness” (amaurosis) of 2 to 3 minutes' duration plus severe constipation occurred in one patient that was administered 72 mg of ondansetron intravenously as a single dose. Hypotension (and faintness) occurred in another patient that took 48 mg of ondansetron hydrochloride tablets. Following infusion of 32 mg over only a 4-minute period, a vasovagal episode with transient second-degree heart block was observed. In all instances, the events resolved completely.
Pediatric cases consistent with serotonin syndrome have been reported after inadvertent oral overdoses of ondansetron (exceeding estimated ingestion of 5 mg/kg) in young children. Reported symptoms included somnolence, agitation, tachycardia, tachypnea, hypertension, flushing, mydriasis, diaphoresis, myoclonic movements, horizontal nystagmus, hyperreflexia, and seizure. Patients required supportive care, including intubation in some cases, with complete recovery without sequelae within 1 to 2 days.
Pharmacology
There is limited information regarding Ondansetron (injection) Pharmacology in the drug label.
Mechanism of Action
There is limited information regarding Ondansetron (injection) Mechanism of Action in the drug label.
Structure
There is limited information regarding Ondansetron (injection) Structure in the drug label.
Pharmacodynamics
There is limited information regarding Ondansetron (injection) Pharmacodynamics in the drug label.
Pharmacokinetics
There is limited information regarding Ondansetron (injection) Pharmacokinetics in the drug label.
Nonclinical Toxicology
There is limited information regarding Ondansetron (injection) Nonclinical Toxicology in the drug label.
Clinical Studies
There is limited information regarding Ondansetron (injection) Clinical Studies in the drug label.
How Supplied
There is limited information regarding Ondansetron (injection) How Supplied in the drug label.
Storage
There is limited information regarding Ondansetron (injection) Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Ondansetron (injection) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Ondansetron (injection) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Ondansetron (injection) Patient Counseling Information in the drug label.
Precautions with Alcohol
Alcohol-Ondansetron (injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Ondansetron (injection) Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Ondansetron (injection) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Freedman SB, Adler M, Seshadri R, Powell EC (2006). "Oral ondansetron for gastroenteritis in a pediatric emergency department". N Engl J Med. 354 (16): 1698–705. doi:10.1056/NEJMoa055119. PMID 16625009.
- ↑ Freedman SB, Powell EC, Nava-Ocampo AA, Finkelstein Y (2010). "Ondansetron dosing in pediatric gastroenteritis: a prospective cohort, dose-response study". Paediatr Drugs. 12 (6): 405–10. doi:10.2165/11537770-000000000-00000. PMID 21028919.