Nivolumab
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
Title
See full prescribing information for complete Boxed Warning.
ConditionName:
|
Overview
Nivolumab is a that is FDA approved for the {{{indicationType}}} of patients with unresectable or metastatic melanoma and disease progression following ipilimumab and, if BRAF V600 mutation positive, a BRAF inhibitor. There is a Black Box Warning for this drug as shown here. Common adverse reactions include .
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Metastatic Melanoma
- Nivolumab ® (nivolumab) is indicated for the treatment of patients with unresectable or metastatic melanoma and disease progression following ipilimumab and, if BRAF V600 mutation positive, a BRAF inhibitor .
- This indication is approved under accelerated approval based on tumor response rate and durability of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
Recommended Dosage
- The recommended dose of Nivolumab is 3 mg/kg administered as an intravenous infusion over 60 minutes every 2 weeks until disease progression or unacceptable toxicity.
Dose Modifications
- There are no recommended dose modifications for hypothyroidism or hyperthyroidism.
- Withhold Nivolumab for any of the following:
- Grade 2 pneumonitis
- Grade 2 or 3 colitis
- Aspartate aminotransferase (AST) or alanine aminotransferase (ALT) greater than 3 and up to 5 times upper limit of normal (ULN) or total bilirubin greater than 1.5 and up to 3 times ULN
- Creatinine greater than 1.5 and up to 6 times ULN or greater than 1.5 times baseline
- Any other severe or Grade 3 treatment-related adverse reactions
- Resume Nivolumab in patients whose adverse reactions recover to Grade 0-1.
- Permanently discontinue Nivolumab for any of the following:
- Any life-threatening or Grade 4 adverse reaction
- Grade 3 or 4 pneumonitis
- Grade 4 colitis
- AST or ALT greater than 5 times ULN or total bilirubin greater than 3 times ULN
- Creatinine greater than 6 times ULN
- Any severe or Grade 3 treatment-related adverse reaction that recurs
- Inability to reduce corticosteroid dose to 10 mg or less of prednisone or equivalent per day within 12 weeks
- Persistent Grade 2 or 3 treatment-related adverse reactions that do not recover to Grade 0-1 within 12 weeks after last dose of Nivolumab
Preparation and Administration
- Visually inspect drug product solution for particulate matter and discoloration prior to administration. Nivolumab is a clear to opalescent, colorless to pale-yellow solution. Discard the vial if the solution is cloudy, is discolored, or contains extraneous particulate matter other than a few translucent-to-white, proteinaceous particles. Do not shake the vial.
Preparation
- Withdraw the required volume of Nivolumab and transfer into an intravenous container.
- Dilute Nivolumab with either 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP, to prepare an infusion with a final concentration ranging from 1 mg/mL to 10 mg/mL.
- Mix diluted solution by gentle inversion. Do not shake.
- Discard partially used vials or empty vials of Nivolumab .
Storage of Infusion
- The product does not contain a preservative.
- After preparation, store the Nivolumab infusion either:
- at room temperature for no more than 4 hours from the time of preparation. This includes room temperature storage of the infusion in the IV container and time for administration of the infusion or
- under refrigeration at 2°C to 8°C (36°F-46°F) for no more than 24 hours from the time of infusion preparation.
- Do not freeze.
Administration
- Administer the infusion over 60 minutes through an intravenous line containing a sterile, non-pyrogenic, low protein binding in-line filter (pore size of 0.2 micrometer to 1.2 micrometer).
- Do not coadminister other drugs through the same intravenous line.
- Flush the intravenous line at end of infusion.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Nivolumab in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Nivolumab in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
- The safety and effectiveness of Nivolumab have not been established in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
- The safety and effectiveness of Nivolumab have not been established in pediatric patients.
Non–Guideline-Supported Use
- The safety and effectiveness of Nivolumab have not been established in pediatric patients.
Contraindications
- None.
Warnings
|
Title
See full prescribing information for complete Boxed Warning.
ConditionName:
|
Immune-Mediated Pneumonitis
- Severe pneumonitis or interstitial lung disease, including fatal cases, occurred with Nivolumab treatment. Across the clinical trial experience in 574 patients with solid tumors, fatal immune-mediated pneumonitis occurred in 0.9% (5/574) of patients receiving Nivolumab . No cases of fatal pneumonitis occurred in Trial 1; all five fatal cases occurred in a dose-finding study with Nivolumab doses of 1 mg/kg (two patients), 3 mg/kg (two patients), and 10 mg/kg (one patient).
- In Trial 1, pneumonitis, including interstitial lung disease, occurred in 3.4% (9/268) of patients receiving Nivolumab and none of the 102 patients receiving chemotherapy. Immune-mediated pneumonitis, defined as requiring use of corticosteroids and no clear alternate etiology, occurred in 2.2% (6/268) of patients receiving Nivolumab : one with Grade 3 and five with Grade 2 pneumonitis. The median time to onset for the six cases was 2.2 months (range: 25 days-3.5 months). In two patients, pneumonitis was diagnosed after discontinuation of Nivolumab for other reasons, and Grade 2 pneumonitis led to interruption or permanent discontinuation of Nivolumab in the remaining four patients. All six patients received high-dose corticosteroids (at least 40 mg prednisone equivalents per day); immune-mediated pneumonitis improved to Grade 0 or 1 with corticosteroids in all six patients. There were two patients with Grade 2 pneumonitis that completely resolved (defined as improved to Grade 0 with completion of corticosteroids) and Nivolumab was restarted without recurrence of pneumonitis.
- Monitor patients for signs and symptoms of pneumonitis. Administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents for Grade 2 or greater pneumonitis, followed by corticosteroid taper. Permanently discontinue Nivolumab for severe (Grade 3) or life-threatening (Grade 4) pneumonitis and withhold Nivolumab until resolution for moderate (Grade 2) pneumonitis.
Immune-Mediated Colitis
- In Trial 1, diarrhea or colitis occurred in 21% (57/268) of patients receiving Nivolumab and 18% (18/102) of patients receiving chemotherapy. Immune-mediated colitis, defined as requiring use of corticosteroids with no clear alternate etiology, occurred in 2.2% (6/268) of patients receiving Nivolumab : five patients with Grade 3 and one patient with Grade 2 colitis. The median time to onset of immune-mediated colitis from initiation of Nivolumab was 2.5 months (range: 1-6 months). In three patients, colitis was diagnosed after discontinuation of Nivolumab for other reasons, and Grade 2 or 3 colitis led to interruption or permanent discontinuation of Nivolumab in the remaining three patients. Five of these six patients received high-dose corticosteroids (at least 40 mg prednisone equivalents) for a median duration of 1.4 months (range: 3 days-2.4 months) preceding corticosteroid taper. The sixth patient continued on low-dose corticosteroids started for another immune-mediated adverse reaction. Immune-mediated colitis improved to Grade 0 with corticosteroids in five patients, including one patient with Grade 3 colitis retreated after complete resolution (defined as improved to Grade 0 with completion of corticosteroids) without additional events of colitis. Grade 2 colitis was ongoing in one patient.
- Monitor patients for immune-mediated colitis. Administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents followed by corticosteroid taper for severe (Grade 3) or life-threatening (Grade 4) colitis. Administer corticosteroids at a dose of 0.5 to 1 mg/kg/day prednisone equivalents followed by corticosteroid taper for moderate (Grade 2) colitis of more than 5 days duration; if worsening or no improvement occurs despite initiation of corticosteroids, increase dose to 1 to 2 mg/kg/day prednisone equivalents. Withhold Nivolumab for Grade 2 or 3 immune-mediated colitis. Permanently discontinue Nivolumab for Grade 4 colitis or for recurrent colitis upon restarting Nivolumab .
Immune-Mediated Hepatitis
- In Trial 1, there was an increased incidence of liver test abnormalities in the Nivolumab -treated group as compared to the chemotherapy-treated group, with increases in AST (28% vs. 12%), alkaline phosphatase (22% vs. 13%), ALT (16% vs. 5%), and total bilirubin (9% vs. 0). Immune-mediated hepatitis, defined as requirement for corticosteroids and no clear alternate etiology, occurred in 1.1% (3/268) of patients receiving Nivolumab : two patients with Grade 3 and one patient with Grade 2 hepatitis. The time to onset was 97, 113, and 86 days after initiation of Nivolumab . In one patient, hepatitis was diagnosed after discontinuation of Nivolumab for other reasons. In two patients, Nivolumab was withheld. All three patients received high-dose corticosteroids (at least 40 mg prednisone equivalents). Liver tests improved to Grade 1 within 4-15 days of initiation of corticosteroids. Immune-mediated hepatitis resolved and did not recur with continuation of corticosteroids in two patients; the third patient died of disease progression with persistent hepatitis. The two patients with Grade 3 hepatitis that resolved restarted Nivolumab and, in one patient, Grade 3 immune-mediated hepatitis recurred resulting in permanent discontinuation of Nivolumab .
- Monitor patients for abnormal liver tests prior to and periodically during treatment. Administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents for Grade 2 or greater transaminase elevations, with or without concomitant elevation in total bilirubin. Withhold Nivolumab for moderate (Grade 2) and permanently discontinue Nivolumab for severe (Grade 3) or life-threatening (Grade 4) immune-mediated hepatitis .
Immune-Mediated Nephritis and Renal Dysfunction
- In Trial 1, there was an increased incidence of elevated creatinine in the Nivolumab -treated group as compared to the chemotherapy-treated group (13% vs. 9%). Grade 2 or 3 immune-mediated nephritis or renal dysfunction (defined as ≥ Grade 2 increased creatinine, requirement for corticosteroids, and no clear alternate etiology) occurred in 0.7% (2/268) of patients at 3.5 and 6 months after Nivolumab initiation, respectively. Nivolumab was permanently discontinued in both patients; both received high-dose corticosteroids (at least 40 mg prednisone equivalents). Immune-mediated nephritis resolved and did not recur with continuation of corticosteroids in one patient. Renal dysfunction was ongoing in one patient.
- Monitor patients for elevated serum creatinine prior to and periodically during treatment. Administer corticosteroids at a dose of 1 to 2 mg/kg/day prednisone equivalents followed by corticosteroid taper for life-threatening (Grade 4) serum creatinine elevation and permanently discontinue Nivolumab . For severe (Grade 3) or moderate (Grade 2) serum creatinine elevation, withhold Nivolumab and administer corticosteroids at a dose of 0.5 to 1 mg/kg/day prednisone equivalents followed by corticosteroid taper; if worsening or no improvement occurs, increase dose of corticosteroids to 1 to 2 mg/kg/day prednisone equivalents and permanently discontinue Nivolumab .
Immune-Mediated Hypothyroidism and Hyperthyroidism
- In Trial 1, where patients were evaluated at baseline and during the trial for thyroid function, Grade 1 or 2 hypothyroidism occurred in 8% (21/268) of patients receiving Nivolumab and none of the 102 patients receiving chemotherapy. The median time to onset was 2.5 months (range: 24 days-11.7 months). Seventeen of the 21 patients with hypothyroidism received levothyroxine. Fifteen of 17 patients received subsequent Nivolumab dosing while continuing to receive levothyroxine.
- Grade 1 or 2 hyperthyroidism occurred in 3% (8/268) of patients receiving Nivolumab and 1% (1/102) of patients receiving chemotherapy. The median time to onset in Nivolumab -treated patients was 1.6 months (range: 0-3.3 months). Four of five patients with Grade 1 hyperthyroidism and two of three patients with Grade 2 hyperthyroidism had documented resolution of hyperthyroidism; all three patients received medical management for Grade 2 hyperthyroidism.
- Monitor thyroid function prior to and periodically during treatment. Administer hormone replacement therapy for hypothyroidism. Initiate medical management for control of hyperthyroidism. There are no recommended dose adjustments of Nivolumab for hypothyroidism or hyperthyroidism.
Other Immune-Mediated Adverse Reactions
- Other clinically significant immune-mediated adverse reactions can occur. Immune-mediated adverse reactions may occur after discontinuation of Nivolumab therapy.
- The following clinically significant, immune-mediated adverse reactions occurred in less than 1% of Nivolumab -treated patients in Trial 1: pancreatitis, uveitis, demyelination, autoimmune neuropathy, adrenal insufficiency, and facial and abducens nerve paresis.
- Across clinical trials of Nivolumab administered at doses of 3 mg/kg and 10 mg/kg the following additional clinically significant, immune-mediated adverse reactions were identified: hypophysitis, diabetic ketoacidosis, hypopituitarism, Guillain-Barré syndrome, and myasthenic syndrome.
- For any suspected immune-mediated adverse reactions, exclude other causes. Based on the severity of the adverse reaction, withhold Nivolumab , administer high-dose corticosteroids, and if appropriate, initiate hormone-replacement therapy. Upon improvement to Grade 1 or less, initiate corticosteroid taper and continue to taper over at least 1 month. Consider restarting Nivolumab after completion of corticosteroid taper based on the severity of the event
Embryofetal Toxicity
- Based on its mechanism of action and data from animal studies, Nivolumab can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, administration of nivolumab to cynomolgus monkeys from the onset of organogenesis through delivery resulted in increased abortion and premature infant death. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with Nivolumab and for at least 5 months after the last dose of Nivolumab
Adverse Reactions
Clinical Trials Experience
- The following adverse reactions are discussed in greater detail in other sections of the labeling.
- Immune-Mediated Pneumonitis
- Immune-Mediated Colitis
- Immune-Mediated Hepatitis
- Immune-Mediated Nephritis and Renal Dysfunction
- Immune-Mediated Hypothyroidism and Hyperthyroidism
- Other Immune-Mediated Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
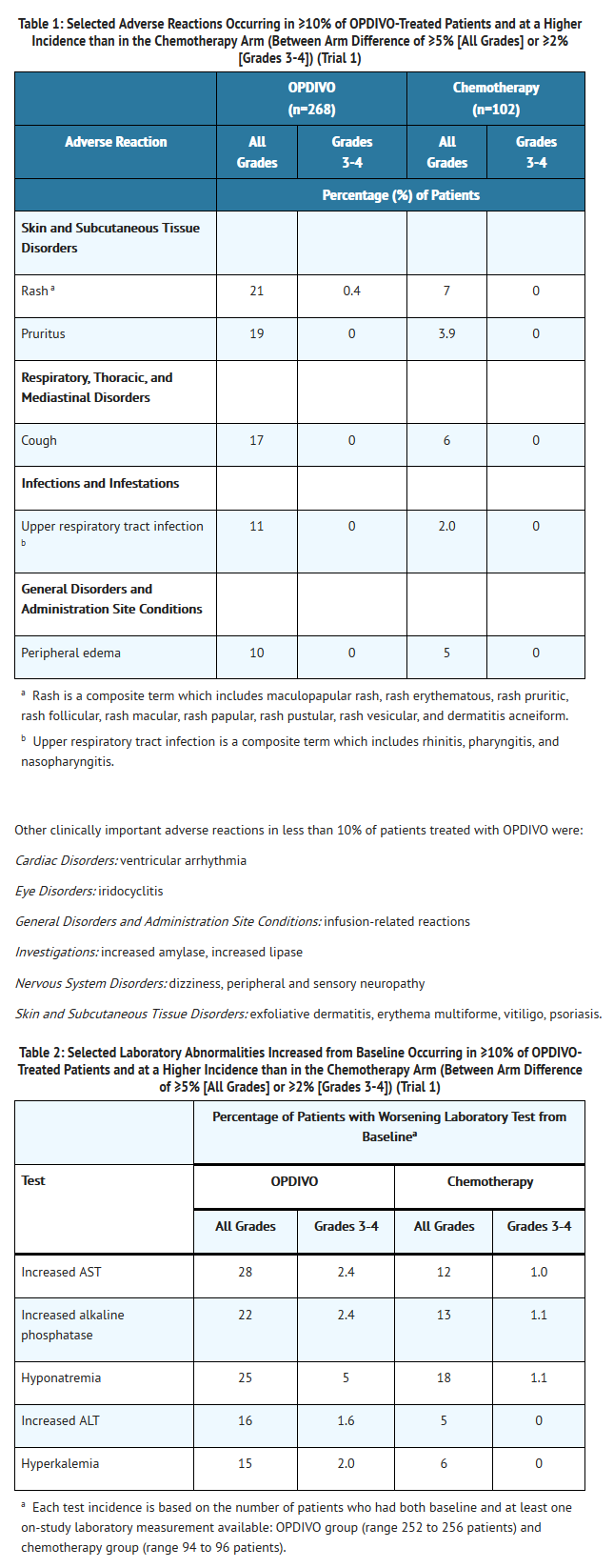
- The data described in the WARNINGS section and below reflect exposure to Nivolumab in Trial 1, a randomized, open-label trial in which 370 patients with unresectable or metastatic melanoma received Nivolumab 3 mg/kg every 2 weeks (n=268) or investigator’s choice of chemotherapy (n=102), either dacarbazine 1000 mg/m2 every 3 weeks or the combination of carboplatin AUC 6 every 3 weeks plus paclitaxel 175 mg/m2 every 3 weeks. The median duration of exposure was 5.3 months (range: 1 day-13.8+ months) with a median of eight doses (range: 1 to 31) in Nivolumab -treated patients and was 2 months (range: 1 day-9.6+ months) in chemotherapy treated patients. In this ongoing trial, 24% of patients received Nivolumab for greater than 6 months and 3% of patients received Nivolumab for greater than 1 year.
- Clinically significant adverse reactions were also evaluated in 574 patients with solid tumors enrolled in two clinical trials receiving Nivolumab at doses of 0.1 to 10 mg/kg every 2 weeks, supplemented by immune-mediated adverse reaction reports across ongoing clinical trials.
- In Trial 1, patients had documented disease progression following treatment with ipilimumab and, if BRAF V600 mutation positive, a BRAF inhibitor. The trial excluded patients with autoimmune disease, prior ipilimumab-related Grade 4 adverse reactions (except for endocrinopathies) or Grade 3 ipilimumab-related adverse reactions that had not resolved or were inadequately controlled within 12 weeks of the initiating event, patients with a condition requiring chronic systemic treatment with corticosteroids (>10 mg daily prednisone equivalent) or other immunosuppressive medications, a positive test for hepatitis B or C, and a history of HIV.
- The study population characteristics in the Nivolumab group and the chemotherapy group were similar: 66% male, median age 59.5 years, 98% white, baseline ECOG performance status 0 (59%) or 1 (41%), 74% with M1c stage disease, 73% with cutaneous melanoma, 11% with mucosal melanoma, 73% received two or more prior therapies for advanced or metastatic disease, and 18% had brain metastasis. There were more patients in the Nivolumab group with elevated LDH at baseline (51% vs. 38%).
- Nivolumab was discontinued for adverse reactions in 9% of patients. Twenty-six percent of patients receiving Nivolumab had a drug delay for an adverse reaction. Serious adverse reactions occurred in 41% of patients receiving Nivolumab . Grade 3 and 4 adverse reactions occurred in 42% of patients receiving Nivolumab . The most frequent Grade 3 and 4 adverse reactions reported in 2% to less than 5% of patients receiving Nivolumab were abdominal pain, hyponatremia, increased aspartate aminotransferase, and increased lipase.
- Table 1 summarizes the adverse reactions that occurred in at least 10% of Nivolumab -treated patients. The most common adverse reaction (reported in at least 20% of patients) was rash.
Immunogenicity
- As with all therapeutic proteins, there is a potential for immunogenicity.
- Of 281 patients who were treated with Nivolumab 3 mg/kg every 2 weeks and evaluable for the presence of anti-product antibodies, 24 patients (8.5%) tested positive for treatment-emergent anti-product antibodies by an electrochemiluminescent (ECL) assay. Neutralizing antibodies were detected in two patients (0.7%). There was no evidence of altered pharmacokinetic profile or toxicity profile with anti-product binding antibody development based on the population pharmacokinetic and exposure-response analyses.
- The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of incidence of antibodies to Nivolumab with the incidences of antibodies to other products may be misleading.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Nivolumab in the drug label.
Drug Interactions
- No formal pharmacokinetic drug-drug interaction studies have been conducted with Nivolumab .
Use in Specific Populations
Pregnancy
Risk Summary
- Based on its mechanism of action and data from animal studies, Nivolumab can cause fetal harm when administered to a pregnant woman . In animal reproduction studies, administration of nivolumab to cynomolgus monkeys from the onset of organogenesis through delivery resulted in increased abortion and premature infant death [see DATA]. Human IgG4 is known to cross the placental barrier and nivolumab is an immunoglobulin G4 (IgG4); therefore, nivolumab has the potential to be transmitted from the mother to the developing fetus. The effects of Nivolumab are likely to be greater during the second and third trimesters of pregnancy. There are no available human data informing the drug-associated risk. Advise pregnant women of the potential risk to a fetus.
- The background risk of major birth defects and miscarriage for the indicated population is unknown; however, the background risk in the U.S. general population of major birth defects is 2-4% and of miscarriage is 15-20% of clinically recognized pregnancies.
Data
Animal Data
- A central function of the PD-1/PD-L1 pathway is to preserve pregnancy by maintaining maternal immune tolerance to the fetus. Blockade of PD-L1 signaling has been shown in murine models of pregnancy to disrupt tolerance to the fetus and to increase fetal loss. The effects of nivolumab on prenatal and postnatal development were evaluated in monkeys that received nivolumab twice weekly from the onset of organogenesis through delivery, at exposure levels of between 9 and 42 times higher than those observed at the clinical dose of 3 mg/kg of nivolumab (based on AUC). Nivolumab administration resulted in a non-dose-related increase in spontaneous abortion and increased neonatal death. Based on its mechanism of action, fetal exposure to nivolumab may increase the risk of developing immune-mediated disorders or altering the normal immune response and immune-mediated disorders have been reported in PD-1 knockout mice. In surviving infants (18 of 32 compared to 11 of 16 vehicle-exposed infants) of cynomolgus monkeys treated with nivolumab, there were no apparent malformations and no effects on neurobehavioral, immunological, or clinical pathology parameters throughout the 6-month postnatal period.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Nivolumab in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Nivolumab during labor and delivery.
Nursing Mothers
Risk Summary
- It is not known whether Nivolumab is present in human milk. Because many drugs, including antibodies are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Nivolumab , advise women to discontinue breastfeeding during treatment with Nivolumab .
Pediatric Use
- The safety and effectiveness of Nivolumab have not been established in pediatric patients.
Geriatic Use
- Clinical studies of Nivolumab did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently from younger patients. Of the 272 patients randomized to Nivolumab in Trial 1, 35% of patients were 65 years or older and 15% were 75 years or older.
Gender
There is no FDA guidance on the use of Nivolumab with respect to specific gender populations.
Race
There is no FDA guidance on the use of Nivolumab with respect to specific racial populations.
Renal Impairment
- Based on a population pharmacokinetic analysis, no dose adjustment is recommended in patients with renal impairment
Hepatic Impairment
- Based on a population pharmacokinetic analysis, no dose adjustment is recommended for patients with mild hepatic impairment. Nivolumab has not been studied in patients with moderate or severe hepatic impairment
Females of Reproductive Potential and Males
Contraception
- Based on its mechanism of action, Nivolumab can cause fetal harm when administered to a pregnant woman . Advise females of reproductive potential to use effective contraception during treatment with Nivolumab and for at least 5 months following the last dose of Nivolumab .
Immunocompromised Patients
There is no FDA guidance one the use of Nivolumab in patients who are immunocompromised.
Administration and Monitoring
Administration
- Intravenous
Monitoring
There is limited information regarding Monitoring of Nivolumab in the drug label.
- Description
IV Compatibility
There is limited information regarding IV Compatibility of Nivolumab in the drug label.
Overdosage
- There is no information on overdosage with Nivolumab .
Pharmacology
Mechanism of Action
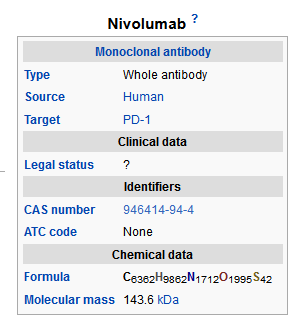
- Binding of the PD-1 ligands, PD-L1 and PD-L2, to the PD-1 receptor found on T cells, inhibits T-cell proliferation and cytokine production. Upregulation of PD-1 ligands occurs in some tumors and signaling through this pathway can contribute to inhibition of active T-cell immune surveillance of tumors. Nivolumab is a human immunoglobulin G4 (IgG4) monoclonal antibody that binds to the PD-1 receptor and blocks its interaction with PD-L1 and PD-L2, releasing PD-1 pathway-mediated inhibition of the immune response, including the anti-tumor immune response. In syngeneic mouse tumor models, blocking PD-1 activity resulted in decreased tumor growth.
Structure
- Nivolumab is a human monoclonal antibody that blocks the interaction between PD-1 and its ligands, PD-L1 and PD-L2. Nivolumab is an IgG4 kappa immunoglobulin that has a calculated molecular mass of 146 kDa.
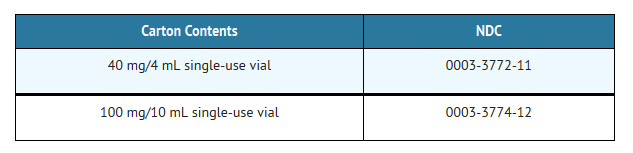
- Nivolumab is a sterile, preservative-free, non-pyrogenic, clear to opalescent, colorless to pale-yellow liquid that may contain light (few) particles. Nivolumab injection for intravenous infusion is supplied in single-use vials. Each mL of Nivolumab solution contains nivolumab 10 mg, mannitol (30 mg), pentetic acid (0.008 mg), polysorbate 80 (0.2 mg), sodium chloride (2.92 mg), sodium citrate dihydrate (5.88 mg), and Water for Injection, USP. May contain hydrochloric acid and/or sodium hydroxide to adjust pH to 6.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Nivolumab in the drug label.
Pharmacokinetics
- The pharmacokinetics (PK) of nivolumab was studied in patients over a dose range of 0.1 to 20 mg/kg administered as a single dose or as multiple doses of Nivolumab every 2 or 3 weeks. Based on a population pharmacokinetic (PK) analysis using data from 909 patients, the geometric mean (% coefficient of variation [CV%]) clearance (CL) is 9.5 mL/h (49.7%), geometric mean volume of distribution at steady state (Vss) is 8.0 L (30.4%), and geometric mean elimination half-life (t1/2) is 26.7 days (101%). Steady-state concentrations of nivolumab were reached by 12 weeks when administered at 3 mg/kg every 2 weeks, and systemic accumulation was approximately 3-fold. The exposure to nivolumab increased dose proportionally over the dose range of 0.1 to 10 mg/kg administered every 2 weeks.
- Specific Populations: Based on a population PK analysis using data from 909 patients, the clearance of nivolumab increased with increasing body weight supporting a weight-based dose. The population PK analysis suggested that the following factors had no clinically important effect on the clearance of nivolumab: age (29 to 87 years), gender, race, baseline LDH, PD-L1 expression, tumor type, tumor size, renal impairment, and mild hepatic impairment.
- Renal Impairment: The effect of renal impairment on the clearance of nivolumab was evaluated by a population PK analysis in patients with mild (eGFR 60 to 89 mL/min/1.73 m2; n=313), moderate (eGFR 30 to 59 mL/min/1.73 m2; n=140), or severe (eGFR 15 to 29 mL/min/1.73 m2; n=3) renal impairment. No clinically important differences in the clearance of nivolumab were found between patients with renal impairment and patients with normal renal function [see USE IN SPECIFIC POPULATIONS (8.6)].
- Hepatic Impairment: The effect of hepatic impairment on the clearance of nivolumab was evaluated by population PK analyses in patients with mild hepatic impairment (total bilirubin [TB] less than or equal to the upper limit of normal [ULN] and AST greater than ULN or TB less than 1 to 1.5 times ULN and any AST; n=92). No clinically important differences in the clearance of nivolumab were found between patients with mild hepatic impairment and patients with normal hepatic function. Nivolumab has not been studied in patients with moderate (TB greater than 1.5 to 3 times ULN and any AST) or severe hepatic impairment (TB greater than 3 times ULN and any AST)
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- No studies have been performed to assess the potential of nivolumab for carcinogenicity or genotoxicity. Fertility studies have not been performed with nivolumab. In 1-month and 3-month repeat-dose toxicology studies in monkeys, there were no notable effects in the male and female reproductive organs; however, most animals in these studies were not sexually mature.
Animal Toxicology and/or Pharmacology
- In animal models, inhibition of PD-1 signaling increased the severity of some infections and enhanced inflammatory responses. M. tuberculosis-infected PD-1 knockout mice exhibit markedly decreased survival compared with wild-type controls, which correlated with increased bacterial proliferation and inflammatory responses in these animals. PD-1 knockout mice have also shown decreased survival following infection with lymphocytic choriomeningitis virus.
Clinical Studies
- Trial 1 was a multicenter, open-label trial that randomized (2:1) patients with unresectable or metastatic melanoma to receive either Nivolumab administered intravenously at 3 mg/kg every 2 weeks or investigator’s choice of chemotherapy, either single-agent dacarbazine 1000 mg/m2 every 3 weeks or the combination of carboplatin AUC 6 every 3 weeks plus paclitaxel 175 mg/m2 every 3 weeks. Patients were required to have progression of disease on or following ipilimumab treatment and, if BRAF V600 mutation positive, a BRAF inhibitor. The trial excluded patients with autoimmune disease, medical conditions requiring systemic immunosuppression, ocular melanoma, active brain metastasis, or a history of Grade 4 ipilimumab-related adverse reactions (except for endocrinopathies) or Grade 3 ipilimumab-related adverse reactions that had not resolved or were inadequately controlled within 12 weeks of the initiating event. Tumor assessments were conducted 9 weeks after randomization then every 6 weeks for the first year, and every 12 weeks thereafter.
- Efficacy was evaluated in a single-arm, non-comparative, planned interim analysis of the first 120 patients who received Nivolumab in Trial 1 and in whom the minimum duration of follow up was 6 months. The major efficacy outcome measures in this population were confirmed objective response rate (ORR) as measured by blinded independent central review using Response Evaluation Criteria in Solid Tumors (RECIST 1.1) and duration of response.
- Among the 120 patients treated with Nivolumab , the median age was 58 years (range: 25-88), 65% of patients were male, 98% were white, and the ECOG PS was 0 (58%) or 1 (42%). Disease characteristics were M1c disease (76%), BRAF V600 mutation positive (22%), elevated LDH (56%), history of brain metastases (18%), and two or more prior systemic therapies for metastatic disease (68%).
- The ORR was 32% (95% confidence interval: 23, 41), consisting of 4 complete responses and 34 partial responses in Nivolumab -treated patients. Of 38 patients with responses, 33 patients (87%) had ongoing responses with durations ranging from 2.6+ to 10+ months, which included 13 patients with ongoing responses of 6 months or longer.
- There were objective responses in patients with and without BRAF V600 mutation positive-melanoma.
How Supplied
- Nivolumab ® (nivolumab) is available as follows:
- Store Nivolumab under refrigeration at 2°C to 8°C (36°F-46°F). Protect Nivolumab from light by storing in the original package until time of use. Do not freeze or shake.
Storage
There is limited information regarding Nivolumab Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Nivolumab |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Nivolumab |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise the patient to read the FDA-approved patient labeling (MEDICATION GUIDE).
- Inform patients of the risk of immune-mediated adverse reactions that may require corticosteroid treatment and interruption or discontinuation of Nivolumab , including:
- Pneumonitis: Advise patients to contact their healthcare provider immediately for any new or worsening cough, chest pain, or shortness of breath .
- Colitis: Advise patients to contact their healthcare provider immediately for diarrhea or severe abdominal pain .
- Hepatitis: Advise patients to contact their healthcare provider immediately for jaundice, severe nausea or vomiting, pain on the right side of abdomen, lethargy, or easy bruising or bleeding
- Nephritis and Renal Dysfunction: Advise patients to contact their healthcare provider immediately for signs or symptoms of nephritis including decreased urine output, blood in urine, swelling in ankles, loss of appetite, and any other symptoms of renal dysfunction .
- Hypothyroidism and Hyperthyroidism: Advise patients to contact their healthcare provider immediately for signs or symptoms of hypothyroidism and hyperthyroidism .
- Advise patients of the importance of keeping scheduled appointments for blood work or other laboratory tests .
- Advise females of reproductive potential of the potential risk to a fetus and to inform their healthcare provider of a known or suspected pregnancy .
- Advise females of reproductive potential to use effective contraception during treatment with Nivolumab and for at least 5 months following the last dose of Nivolumab .
- Advise women not to breastfeed while taking Nivolumab
Precautions with Alcohol
- Alcohol-Nivolumab interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- ®[1]
Look-Alike Drug Names
- A® — B®[2]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Empty citation (help)
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Nivolumab |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Nivolumab |Label Name=Nivolumab04.png
}}
{{#subobject:
|Label Page=Nivolumab |Label Name=Nivolumab05.png
}}
{{#subobject:
|Label Page=Nivolumab |Label Name=Nivolumab06.png
}}