Naldemedine: Difference between revisions
No edit summary |
No edit summary |
||
| Line 300: | Line 300: | ||
|PK=(Description) | |PK=(Description) | ||
|nonClinToxic=(Description) | |nonClinToxic=(Description) | ||
|clinicalStudies= | |clinicalStudies=*SYMPROIC was evaluated in two replicate, 12-week, randomized, double-blind, placebo-controlled trials (Study 1 and Study 2) in which SYMPROIC was used without laxatives in patients with OIC and chronic non-cancer pain. | ||
*Patients receiving a stable opioid morphine equivalent daily dose of at least 30 mg for at least 4 weeks before enrollment and self-reported OIC were eligible for clinical trial participation. | |||
*Patients with evidence of significant structural abnormalities of the GI tract were not enrolled in these trials. | |||
*In Studies 1 and 2, patients had to either be not using laxatives or willing to discontinue laxative use at the time of screening and willing to use only the provided rescue laxatives during the screening and treatment periods. | |||
*In Studies 1 and 2, OIC was confirmed through a two-week run in period and was defined as no more than 4 spontaneous bowel movements (SBMs) total over 14 consecutive days and less than 3 SBMs in a given week with at least 25% of the SBMs associated with one or more of the following conditions: (1) straining; (2) hard or lumpy stools; (3) having a sensation of incomplete evacuation; and (4) having a sensation of anorectal obstruction/blockage. | |||
*An SBM was defined as a bowel movement (BM) without rescue laxative taken within the past 24 hours. Patients with no BMs over the 7 consecutive days prior to and during the 2 week screening period or patients who have never taken laxatives were excluded. | |||
*In the screening and treatment periods, bisacodyl was used as rescue laxative if patients had not had a BM for 72 hours and were allowed one-time use of an enema, if after 24 hours of taking bisacodyl they still had not had a BM. | |||
*A total of 547 patients in Study 1 and 553 patients in Study 2 were randomized in a 1:1 ratio to receive SYMPROIC 0.2 mg once daily or placebo for 12 weeks. Study medication was administered without regard to meals. | |||
*The mean age of subjects in Studies 1 and 2 was 54 years; 59% were women; and 80% were white. The most common types of pain in Studies 1 and 2 were back or neck pain (61%). The mean baseline number of SBMs was 1.3 and 1.2 per week for Studies 1 and 2, respectively. | |||
*Prior to enrollment, patients were using their current opioid for a mean duration of approximately 5 years. A wide range of types of opioids were used. The mean baseline opioid morphine equivalent daily dosage was 132 mg and 121 mg per day for Studies 1 and 2, respectively. | |||
*The efficacy of SYMPROIC was assessed in Studies 1 and 2 using a responder analysis. A responder was defined as a patient who had at least 3 SBMs per week and a change from baseline of at least 1 SBM per week for at least 9 out of the 12 weeks and 3 out of the last 4 weeks in Studies 1 and 2. | |||
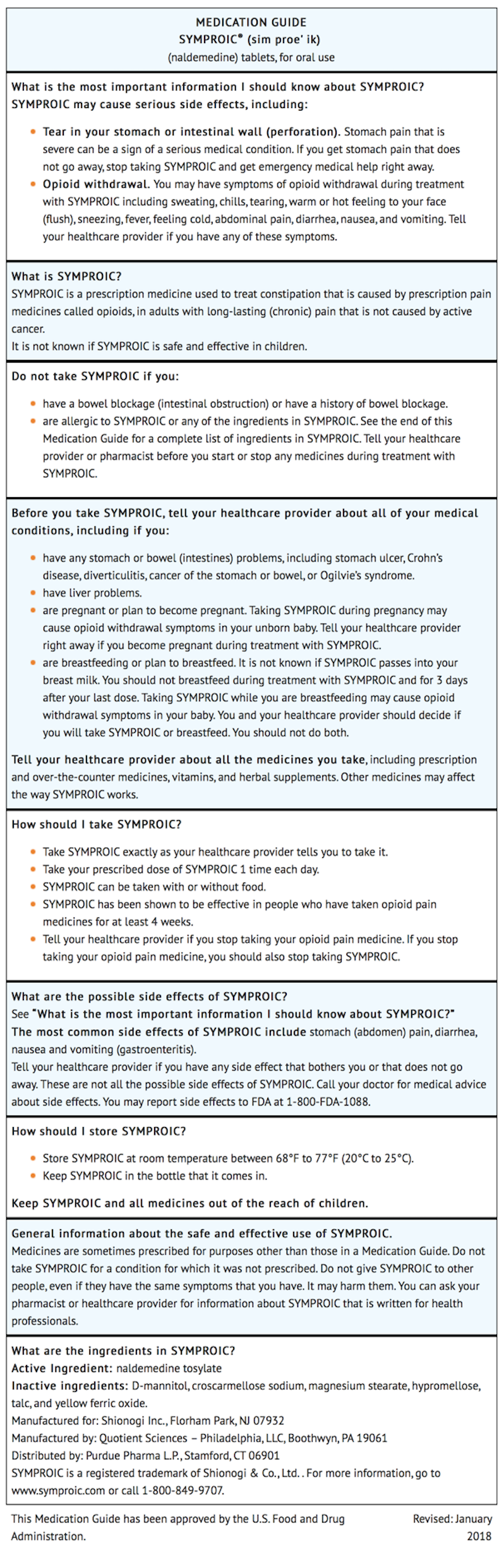
*The responder rates in Studies 1 and 2 are shown in Table 4. | |||
[[image:Naldemedine_Clinical_Studies_Table.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
*In Studies 1 and 2, the mean increase in frequency of SBMs per week from baseline to the last 2 weeks of the 12-week treatment period was 3.1 for SYMPROIC vs. 2.0 for placebo (difference 1.0, 95% CI 0.6, 1.5), and 3.3 for SYMPROIC vs. 2.1 for placebo (difference 1.2, 95% CI 0.8, 1.7), respectively. | |||
*During week 1 of the treatment period, the mean increase in frequency of SBMs per week from baseline was 3.3 for SYMPROIC vs. 1.3 for placebo (difference 2.0, 95% CI 1.5, 2.5) in Study 1 and 3.7 for SYMPROIC vs. 1.6 for placebo (difference 2.1, 95% CI 1.5, 2.6) in Study 2. | |||
*The mean increase in the frequency of complete SBM (CSBM) per week from baseline to the last 2 weeks of 12-week treatment period was 2.3 for SYMPROIC vs. 1.5 for placebo (difference 0.8, 95% CI 0.4, 1.2) in Study 1 and 2.6 for SYMPROIC vs. 1.6 for placebo (difference 1.1, 95% CI 0.6, 1.5) in Study 2. A CSBM was defined as a SBM that was associated with a sense of complete evacuation. | |||
*The change in the frequency of SBMs without straining per week from baseline to the last 2 weeks of the treatment period was 1.3 for SYMPROIC vs. 0.7 for placebo (difference 0.6, 95% CI 0.2, 0.9) in Study 1 and 1.8 for SYMPROIC vs. 1.1 for placebo (difference 0.7, 95% CI 0.3, 1.2) in Study 2. | |||
|howSupplied=*SYMPROIC is supplied as 0.2 mg naldemedine tablets in: | |howSupplied=*SYMPROIC is supplied as 0.2 mg naldemedine tablets in: | ||
Revision as of 12:05, 20 July 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yashasvi Aryaputra[2];
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Naldemedine is a Acetylcholine release inhibitor, Adrenergic receptor agonist that is FDA approved for the (type of indication of drug) of a list of indications, separated by commas.. Common adverse reactions include a list of adverse reactions, separated by commas..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Contraindications
CONTRAINDICATIONS
Warnings
Conidition 1
(Description)
Conidition 2
(Description)
Conidition 3
(Description)
Adverse Reactions
Clinical Trials Experience
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Condition 2
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Postmarketing Experience
(Description)
Drug Interactions
- Drug 1
- Drug 2
- Drug 3
- Drug 4
- Drug 5
Drug 1
(Description)
Drug 2
(Description)
Drug 3
(Description)
Drug 4
(Description)
Drug 5
(Description)
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
(Description)
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Naldemedine in women who are pregnant.
Labor and Delivery
(Description)
Nursing Mothers
(Description)g
Pediatric Use
(Description)
Geriatic Use
(Description)
Gender
(Description)
Race
(Description)
Renal Impairment
(Description)
Hepatic Impairment
(Description)
Females of Reproductive Potential and Males
(Description)
Immunocompromised Patients
(Description)
Others
(Description)
Administration and Monitoring
Administration
(Oral/Intravenous/etc)
Monitoring
Condition 1
(Description regarding monitoring, from Warnings section)
Condition 2
(Description regarding monitoring, from Warnings section)
Condition 3
(Description regarding monitoring, from Warnings section)
IV Compatibility
There is limited information regarding the compatibility of Naldemedine and IV administrations.
Overdosage
Acute Overdose
Signs and Symptoms
(Description)
Management
(Description)
Chronic Overdose
Signs and Symptoms
(Description)
Management
(Description)
Pharmacology
Naldemedine
| |
| Systematic (IUPAC) name | |
| ? | |
| Identifiers | |
| CAS number | ? |
| ATC code | ? |
| PubChem | ? |
| Chemical data | |
| Formula | ? |
| Mol. mass | ? |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
Mechanism of Action
(Description)
Structure
(Description with picture)
Pharmacodynamics
(Description)
Pharmacokinetics
(Description)
Nonclinical Toxicology
(Description)
Clinical Studies
- SYMPROIC was evaluated in two replicate, 12-week, randomized, double-blind, placebo-controlled trials (Study 1 and Study 2) in which SYMPROIC was used without laxatives in patients with OIC and chronic non-cancer pain.
- Patients receiving a stable opioid morphine equivalent daily dose of at least 30 mg for at least 4 weeks before enrollment and self-reported OIC were eligible for clinical trial participation.
- Patients with evidence of significant structural abnormalities of the GI tract were not enrolled in these trials.
- In Studies 1 and 2, patients had to either be not using laxatives or willing to discontinue laxative use at the time of screening and willing to use only the provided rescue laxatives during the screening and treatment periods.
- In Studies 1 and 2, OIC was confirmed through a two-week run in period and was defined as no more than 4 spontaneous bowel movements (SBMs) total over 14 consecutive days and less than 3 SBMs in a given week with at least 25% of the SBMs associated with one or more of the following conditions: (1) straining; (2) hard or lumpy stools; (3) having a sensation of incomplete evacuation; and (4) having a sensation of anorectal obstruction/blockage.
- An SBM was defined as a bowel movement (BM) without rescue laxative taken within the past 24 hours. Patients with no BMs over the 7 consecutive days prior to and during the 2 week screening period or patients who have never taken laxatives were excluded.
- In the screening and treatment periods, bisacodyl was used as rescue laxative if patients had not had a BM for 72 hours and were allowed one-time use of an enema, if after 24 hours of taking bisacodyl they still had not had a BM.
- A total of 547 patients in Study 1 and 553 patients in Study 2 were randomized in a 1:1 ratio to receive SYMPROIC 0.2 mg once daily or placebo for 12 weeks. Study medication was administered without regard to meals.
- The mean age of subjects in Studies 1 and 2 was 54 years; 59% were women; and 80% were white. The most common types of pain in Studies 1 and 2 were back or neck pain (61%). The mean baseline number of SBMs was 1.3 and 1.2 per week for Studies 1 and 2, respectively.
- Prior to enrollment, patients were using their current opioid for a mean duration of approximately 5 years. A wide range of types of opioids were used. The mean baseline opioid morphine equivalent daily dosage was 132 mg and 121 mg per day for Studies 1 and 2, respectively.
- The efficacy of SYMPROIC was assessed in Studies 1 and 2 using a responder analysis. A responder was defined as a patient who had at least 3 SBMs per week and a change from baseline of at least 1 SBM per week for at least 9 out of the 12 weeks and 3 out of the last 4 weeks in Studies 1 and 2.
- The responder rates in Studies 1 and 2 are shown in Table 4.

- In Studies 1 and 2, the mean increase in frequency of SBMs per week from baseline to the last 2 weeks of the 12-week treatment period was 3.1 for SYMPROIC vs. 2.0 for placebo (difference 1.0, 95% CI 0.6, 1.5), and 3.3 for SYMPROIC vs. 2.1 for placebo (difference 1.2, 95% CI 0.8, 1.7), respectively.
- During week 1 of the treatment period, the mean increase in frequency of SBMs per week from baseline was 3.3 for SYMPROIC vs. 1.3 for placebo (difference 2.0, 95% CI 1.5, 2.5) in Study 1 and 3.7 for SYMPROIC vs. 1.6 for placebo (difference 2.1, 95% CI 1.5, 2.6) in Study 2.
- The mean increase in the frequency of complete SBM (CSBM) per week from baseline to the last 2 weeks of 12-week treatment period was 2.3 for SYMPROIC vs. 1.5 for placebo (difference 0.8, 95% CI 0.4, 1.2) in Study 1 and 2.6 for SYMPROIC vs. 1.6 for placebo (difference 1.1, 95% CI 0.6, 1.5) in Study 2. A CSBM was defined as a SBM that was associated with a sense of complete evacuation.
- The change in the frequency of SBMs without straining per week from baseline to the last 2 weeks of the treatment period was 1.3 for SYMPROIC vs. 0.7 for placebo (difference 0.6, 95% CI 0.2, 0.9) in Study 1 and 1.8 for SYMPROIC vs. 1.1 for placebo (difference 0.7, 95% CI 0.3, 1.2) in Study 2.
How Supplied
- SYMPROIC is supplied as 0.2 mg naldemedine tablets in:
- bottle of 30 tablets - NDC 59011-523-30
- bottle of 90 tablets - NDC 59011-523-90
Storage
- Store SYMPROIC in light resistant container at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Images
Drug Images
{{#ask: Page Name::Naldemedine |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel




{{#ask: Label Page::Naldemedine |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Administration
- Advise patients to discontinue SYMPROIC if treatment with the opioid pain medication is also discontinued.
Gastrointestinal Perforation
- Advise patients to discontinue SYMPROIC and to promptly seek medical attention if they develop unusually severe, persistent or worsening abdominal pain.
Opioid Withdrawal
- Advise patients that clusters of symptoms consistent with opioid withdrawal may occur while taking SYMPROIC and to contact their healthcare provider if these symptoms occur.
Pregnancy
- Advise females of reproductive potential, who become pregnant or are planning to become pregnant, that the use of SYMPROIC during pregnancy may precipitate opioid withdrawal in a fetus due to the undeveloped blood-brain barrier.
Lactation
- Advise women that breastfeeding is not recommended during treatment with SYMPROIC and for 3 days after the final dose.
Precautions with Alcohol
Alcohol-Naldemedine interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Symproic
Look-Alike Drug Names
There is limited information regarding Naldemedine Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.