Mycophenolate
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Deepika Beereddy, MBBS [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: EMBRYOFETAL TOXICITY, MALIGNANCIES AND SERIOUS INFECTIONS
See full prescribing information for complete Boxed Warning.
Embryofetal toxicity, Malignancies and Serious infections:
|
Overview
Mycophenolate is an antibiotic, anti-neoplastic agent that is FDA approved for the prophylaxis of organ rejection in patients receiving allogeneic renal, cardiac or hepatic transplants. There is a Black Box Warning for this drug as shown here. Common adverse reactions include diarrhea, leukopenia, sepsis, vomiting, opportunistic infections.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Renal, Cardiac, and Hepatic Transplant- Organ rejection; Prophylaxis
- Mycophenolate mofetil is indicated for the prophylaxis of organ rejection in patients receiving allogeneic renal, cardiac or hepatic transplants. Mycophenolate mofetil should be used concomitantly with cyclosporine and corticosteroids.
- Mycophenolate mofetil intravenous is an alternative dosage form to mycophenolate mofetil capsules, tablets and oral suspension. Mycophenolate mofetil intravenous should be administered within 24 hours following transplantation. Mycophenolate mofetil intravenous can be administered for up to 14 days; patients should be switched to oral mycophenolate mofetil as soon as they can tolerate oral medication.
- Dosing Information
- Renal Transplantation
Adults A dose of 1 g administered orally twice a day (daily dose of 2 g) is recommended for use in renal transplant patients. Although a dose of 1.5 g administered twice daily (daily dose of 3 g) was used in clinical trials and was shown to be safe and effective, no efficacy advantage could be established for renal transplant patients. Patients receiving 2 g/day of mycophenolate mofetil demonstrated an overall better safety profile than did patients receiving 3 g/day of mycophenolate mofetil.
Cardiac Transplantation
Adults
A dose of 1.5 g bid oral (daily dose of 3 g) is recommended for use in adult cardiac transplant patients.
Hepatic Transplantation
Adults
A dose of 1.5 g bid oral (daily dose of 3 g) is recommended for use in adult hepatic transplant patients.
Mycophenolate Mofetil Capsules, Tablets, and Oral Suspension
The initial oral dose of mycophenolate mofetil should be given as soon as possible following renal, cardiac or hepatic transplantation. Food had no effect on MPA AUC, but has been shown to decrease MPA Cmax by 40%. Therefore, it is recommended that mycophenolate mofetil be administered on an empty stomach. However, in stable renal transplant patients, mycophenolate mofetil may be administered with food if necessary.
Patients should be instructed to take a missed dose as soon as they remember, except if it is near the next scheduled dose, and then continue to take mycophenolate mofetil at the usual times.
Note
If required, mycophenolate mofetil oral suspension can be administered via a nasogastric tube with a minimum size of 8 French (minimum 1.7 mm interior diameter).
Patients With Hepatic Impairment
No dose adjustments are recommended for renal patients with severe hepatic parenchymal disease. However, it is not known whether dose adjustments are needed for hepatic disease with other etiologies (see CLINICAL PHARMACOLOGY: Pharmacokinetics).
No data are available for cardiac transplant patients with severe hepatic parenchymal disease.
Geriatrics
The recommended oral dose of 1 g bid for renal transplant patients, 1.5 g bid for cardiac transplant patients, and 1 g bid administered intravenously or 1.5 g bid administered orally in hepatic transplant patients is appropriate for elderly patients (see PRECAUTIONS: Geriatric Use).
Dosage Adjustments
In renal transplant patients with severe chronic renal impairment (GFR <25 mL/min/1.73 m2) outside the immediate posttransplant period, doses of mycophenolate mofetil greater than 1 g administered twice a day should be avoided. These patients should also be carefully observed. No dose adjustments are needed in renal transplant patients experiencing delayed graft function postoperatively (see CLINICAL PHARMACOLOGY: Pharmacokinetics and PRECAUTIONS: Patients with Renal Impairment).
No data are available for cardiac or hepatic transplant patients with severe chronic renal impairment. Mycophenolate mofetil may be used for cardiac or hepatic transplant patients with severe chronic renal impairment if the potential benefits outweigh the potential risks.
If neutropenia develops (ANC <1.3× 103/µL), dosing with mycophenolate mofetil should be interrupted or the dose reduced, appropriate diagnostic tests performed, and the patient managed appropriately (see WARNINGS: Neutropenia, ADVERSE REACTIONS, and PRECAUTIONS: Laboratory Tests).
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Condition1
- Developed by:
- Class of Recommendation:
- Strength of Evidence:
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Guideline-Supported Use of Mycophenolate in adult patients.
Non–Guideline-Supported Use
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Non–Guideline-Supported Use of Mycophenolate in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Organ rejection; Prophylaxis
- Dosing Information
- Renal Transplantation
Pediatrics (3 months to 18 years of age)
The recommended dose of mycophenolate mofetil oral suspension is 600 mg/m2 administered twice daily (up to a maximum daily dose of 2 g/10 mL oral suspension). Patients with a body surface area of 1.25 m2 to 1.5 m2 may be dosed with mycophenolate mofetil capsules at a dose of 750 mg twice daily (1.5 g daily dose). Patients with a body surface area >1.5 m2 may be dosed with mycophenolate mofetil capsules or tablets at a dose of 1 g twice daily (2 g daily dose).
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition1
- Developed by:
- Class of Recommendation:
- Strength of Evidence:
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Guideline-Supported Use of Mycophenolate in pediatric patients.
Non–Guideline-Supported Use
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Non–Guideline-Supported Use of Mycophenolate in pediatric patients.
Contraindications
- Condition1
Warnings
|
WARNING: EMBRYOFETAL TOXICITY, MALIGNANCIES AND SERIOUS INFECTIONS
See full prescribing information for complete Boxed Warning.
Embryofetal toxicity, Malignancies and Serious infections:
|
- Description
Precautions
- Description
Adverse Reactions
Clinical Trials Experience
There is limited information regarding Clinical Trial Experience of Mycophenolate in the drug label.
Body as a Whole
Cardiovascular
Digestive
Endocrine
Hematologic and Lymphatic
Metabolic and Nutritional
Musculoskeletal
Neurologic
Respiratory
Skin and Hypersensitivy Reactions
Special Senses
Urogenital
Miscellaneous
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Mycophenolate in the drug label.
Body as a Whole
Cardiovascular
Digestive
Endocrine
Hematologic and Lymphatic
Metabolic and Nutritional
Musculoskeletal
Neurologic
Respiratory
Skin and Hypersensitivy Reactions
Special Senses
Urogenital
Miscellaneous
Drug Interactions
- Drug
- Description
Use in Specific Populations
Pregnancy
- Pregnancy Category
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Mycophenolate in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Mycophenolate during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Mycophenolate with respect to nursing mothers.
Pediatric Use
There is no FDA guidance on the use of Mycophenolate with respect to pediatric patients.
Geriatic Use
There is no FDA guidance on the use of Mycophenolate with respect to geriatric patients.
Gender
There is no FDA guidance on the use of Mycophenolate with respect to specific gender populations.
Race
There is no FDA guidance on the use of Mycophenolate with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Mycophenolate in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Mycophenolate in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Mycophenolate in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Mycophenolate in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
- Intravenous
Monitoring
There is limited information regarding Monitoring of Mycophenolate in the drug label.
- Description
IV Compatibility
There is limited information regarding IV Compatibility of Mycophenolate in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- Description
Management
- Description
Chronic Overdose
There is limited information regarding Chronic Overdose of Mycophenolate in the drug label.
Pharmacology
Mechanism of Action
Mycophenolate mofetil has been demonstrated in experimental animal models to prolong the survival of allogeneic transplants (kidney, heart, liver, intestine, limb, small bowel, pancreatic islets, and bone marrow).
Mycophenolate mofetil has also been shown to reverse ongoing acute rejection in the canine renal and rat cardiac allograft models. Mycophenolate mofetil also inhibited proliferative arteriopathy in experimental models of aortic and cardiac allografts in rats, as well as in primate cardiac xenografts. Mycophenolate mofetil was used alone or in combination with other immunosuppressive agents in these studies. Mycophenolate mofetil has been demonstrated to inhibit immunologically mediated inflammatory responses in animal models and to inhibit tumor development and prolong survival in murine tumor transplant models.
Mycophenolate mofetil is rapidly absorbed following oral administration and hydrolyzed to form MPA, which is the active metabolite. MPA is a potent, selective, uncompetitive, and reversible inhibitor of inosine monophosphate dehydrogenase (IMPDH), and therefore inhibits the de novo pathway of guanosine nucleotide synthesis without incorporation into DNA. Because T- and B-lymphocytes are critically dependent for their proliferation on de novo synthesis of purines, whereas other cell types can utilize salvage pathways, MPA has potent cytostatic effects on lymphocytes. MPA inhibits proliferative responses of T- and B-lymphocytes to both mitogenic and allospecific stimulation. Addition of guanosine or deoxyguanosine reverses the cytostatic effects of MPA on lymphocytes. MPA also suppresses antibody formation by B-lymphocytes. MPA prevents the glycosylation of lymphocyte and monocyte glycoproteins that are involved in intercellular adhesion to endothelial cells and may inhibit recruitment of leukocytes into sites of inflammation and graft rejection. Mycophenolate mofetil did not inhibit early events in the activation of human peripheral blood mononuclear cells, such as the production of interleukin-1 (IL-1) and interleukin-2 (IL-2), but did block the coupling of these events to DNA synthesis and proliferation.
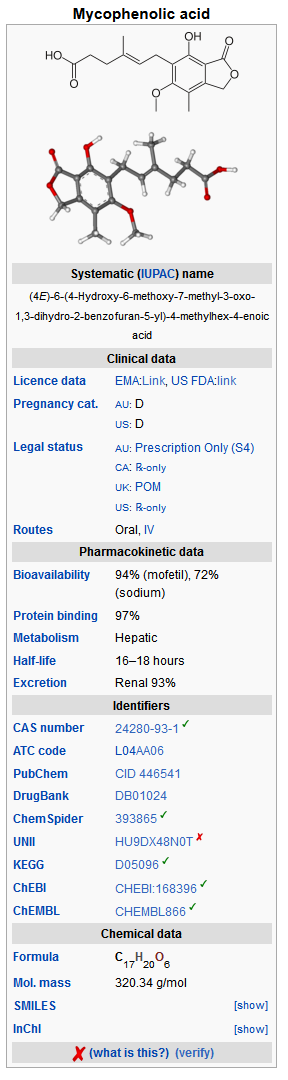
Structure
Mycophenolate mofetil is the 2-morpholinoethyl ester of mycophenolic acid (MPA), an immunosuppressive agent; inosine monophosphate dehydrogenase (IMPDH) inhibitor.
The chemical name for mycophenolate mofetil (MMF) is 2-morpholinoethyl (E)-6-(1,3-dihydro-4-hydroxy-6-methoxy-7-methyl-3-oxo-5-isobenzofuranyl)-4-methyl-4-hexenoate. It has an empirical formula of C23H31NO7, a molecular weight of 433.50, and the following structural formula:
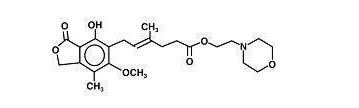
Mycophenolate mofetil is a white to off-white crystalline powder. It is slightly soluble in water (43 µg/mL at pH 7.4); the solubility increases in acidic medium (4.27 mg/mL at pH 3.6). It is freely soluble in acetone, soluble in methanol, and sparingly soluble in ethanol. The apparent partition coefficient in 1-octanol/water (pH 7.4) buffer solution is 238. The pKa values for mycophenolate mofetil are 5.6 for the morpholino group and 8.5 for the phenolic group.
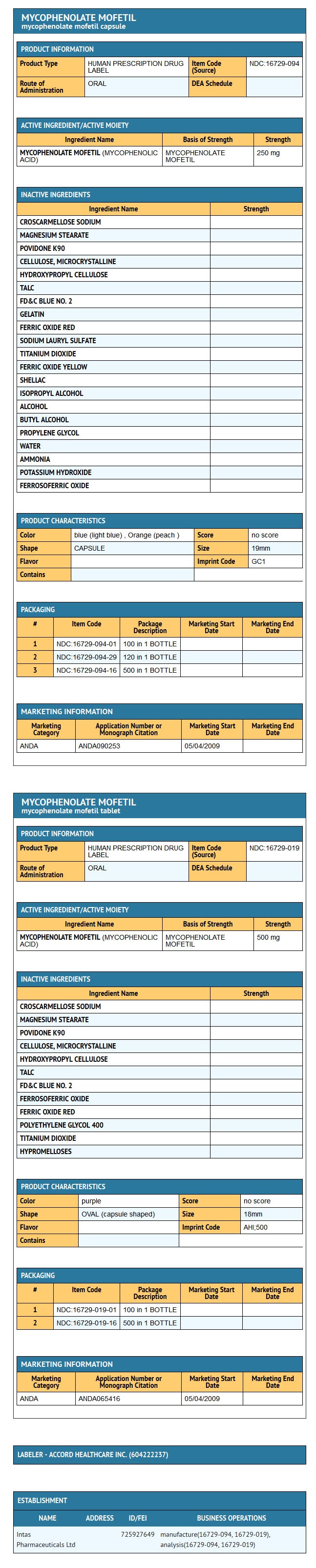
Mycophenolate mofetil is available for oral administration as capsules containing 250 mg of mycophenolate mofetil and tablets containing 500 mg of mycophenolate mofetil.
Inactive ingredients in mycophenolate mofetil 250 mg capsules include croscarmellose sodium, magnesium stearate, povidone (K-90), microcrystalline cellulose, hydroxy propyl cellulose and talc.
The capsule shells contain FD&C blue #2, gelatin, red iron oxide,sodium lauryl sulfate, titanium dioxide, and yellow iron oxide. The imprinting ink contains shellac, iron oxide black and potassium hydroxide.
Inactive ingredients in mycophenolate mofetil tablets 500 mg include iron oxide black , croscarmellose sodium, FD&C blue #2 aluminum lake, hydroxypropyl cellulose, hypromellose, magnesium stearate, microcrystalline cellulose, polyethylene glycol 400, povidone (K-90), iron oxide red, talc, and titanium dioxide
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Mycophenolate in the drug label.
Pharmacokinetics
Following oral and intravenous administration, mycophenolate mofetil undergoes rapid and complete metabolism to MPA, the active metabolite. Oral absorption of the drug is rapid and essentially complete. MPA is metabolized to form the phenolic glucuronide of MPA (MPAG) which is not pharmacologically active. The parent drug, mycophenolate mofetil, can be measured systemically during the intravenous infusion; however, shortly (about 5 minutes) after the infusion is stopped or after oral administration, MMF concentration is below the limit of quantitation (0.4 µg/mL).
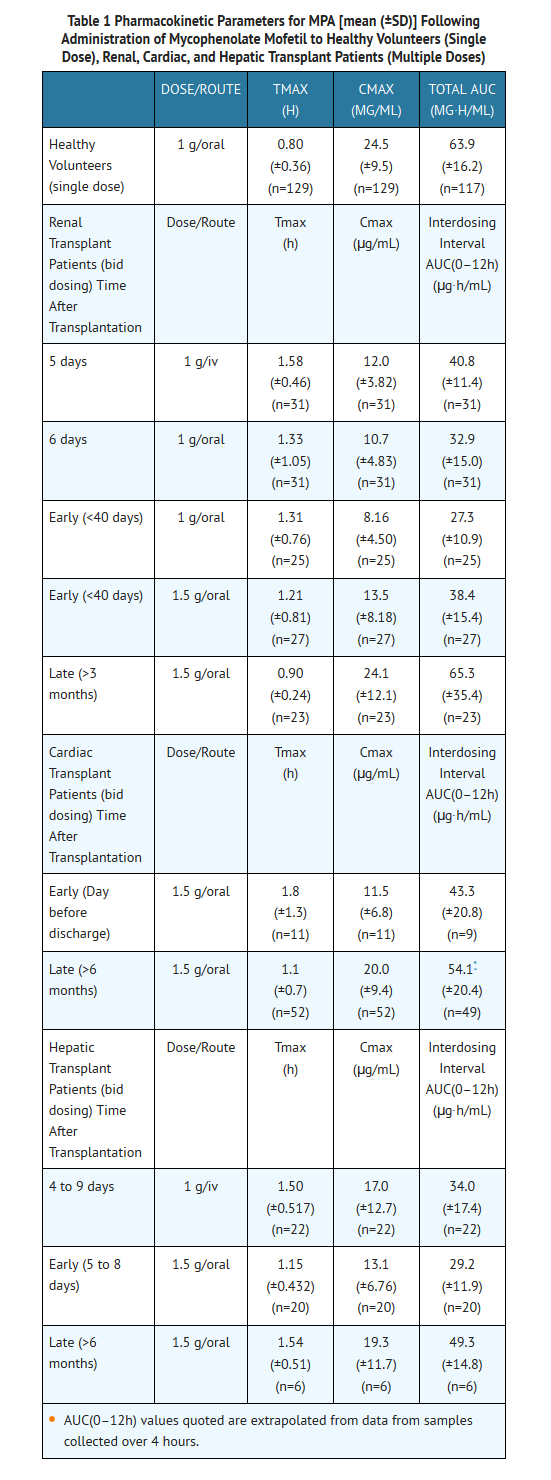
Absorption In 12 healthy volunteers, the mean absolute bioavailability of oral mycophenolate mofetil relative to intravenous mycophenolate mofetil (based on MPA AUC) was 94%. The area under the plasma-concentration time curve (AUC) for MPA appears to increase in a dose-proportional fashion in renal transplant patients receiving multiple doses of mycophenolate mofetil up to a daily dose of 3 g (see Table 1).
Food (27 g fat, 650 calories) had no effect on the extent of absorption (MPA AUC) of mycophenolate mofetil when administered at doses of 1.5 g bid to renal transplant patients. However, MPA Cmax was decreased by 40% in the presence of food (see DOSAGE AND ADMINISTRATION).
Distribution The mean (±SD) apparent volume of distribution of MPA in 12 healthy volunteers is approximately 3.6 (±1.5) and 4.0 (±1.2) L/kg following intravenous and oral administration, respectively. MPA, at clinically relevant concentrations, is 97% bound to plasma albumin. MPAG is 82% bound to plasma albumin at MPAG concentration ranges that are normally seen in stable renal transplant patients; however, at higher MPAG concentrations (observed in patients with renal impairment or delayed renal graft function), the binding of MPA may be reduced as a result of competition between MPAG and MPA for protein binding. Mean blood to plasma ratio of radioactivity concentrations was approximately 0.6 indicating that MPA and MPAG do not extensively distribute into the cellular fractions of blood.
In vitro studies to evaluate the effect of other agents on the binding of MPA to human serum albumin (HSA) or plasma proteins showed that salicylate (at 25 mg/dL with HSA) and MPAG (at ≥460 µg/mL with plasma proteins) increased the free fraction of MPA. At concentrations that exceeded what is encountered clinically, cyclosporine, digoxin, naproxen, prednisone, propranolol, tacrolimus, theophylline, tolbutamide, and warfarin did not increase the free fraction of MPA. MPA at concentrations as high as 100 µg/mL had little effect on the binding of warfarin, digoxin or propranolol, but decreased the binding of theophylline from 53% to 45% and phenytoin from 90% to 87%.
Metabolism Following oral and intravenous dosing, mycophenolate mofetil undergoes complete metabolism to MPA, the active metabolite. Metabolism to MPA occurs presystemically after oral dosing. MPA is metabolized principally by glucuronyl transferase to form the phenolic glucuronide of MPA (MPAG) which is not pharmacologically active. In vivo, MPAG is converted to MPA via enterohepatic recirculation. The following metabolites of the 2-hydroxyethyl-morpholino moiety are also recovered in the urine following oral administration of mycophenolate mofetil to healthy subjects: N-(2-carboxymethyl)-morpholine, N-(2-hydroxyethyl)-morpholine, and the N-oxide of N-(2-hydroxyethyl)-morpholine.
Secondary peaks in the plasma MPA concentration-time profile are usually observed 6 to 12 hours postdose. The coadministration of cholestyramine (4 g tid) resulted in approximately a 40% decrease in the MPA AUC (largely as a consequence of lower concentrations in the terminal portion of the profile). These observations suggest that enterohepatic recirculation contributes to MPA plasma concentrations.
Increased plasma concentrations of mycophenolate mofetil metabolites (MPA 50% increase and MPAG about a 3-fold to 6-fold increase) are observed in patients with renal insufficiency (see CLINICAL PHARMACOLOGY: Special Populations).
Excretion Negligible amount of drug is excreted as MPA (<1% of dose) in the urine. Orally administered radiolabeled mycophenolate mofetil resulted in complete recovery of the administered dose, with 93% of the administered dose recovered in the urine and 6% recovered in feces. Most (about 87%) of the administered dose is excreted in the urine as MPAG. At clinically encountered concentrations, MPA and MPAG are usually not removed by hemodialysis. However, at high MPAG plasma concentrations (>100 µg/mL), small amounts of MPAG are removed. Bile acid sequestrants, such as cholestyramine, reduce MPA AUC by interfering with enterohepatic circulation of the drug (see OVERDOSAGE).
Mean (±SD) apparent half-life and plasma clearance of MPA are 17.9 (±6.5) hours and 193 (±48) mL/min following oral administration and 16.6 (±5.8) hours and 177 (±31) mL/min following intravenous administration, respectively.
Pharmacokinetics in Healthy Volunteers, Renal, Cardiac, and Hepatic Transplant Patients Shown below are the mean (±SD) pharmacokinetic parameters for MPA following the administration of mycophenolate mofetil given as single doses to healthy volunteers and multiple doses to renal, cardiac, and hepatic transplant patients. In the early posttransplant period (<40 days posttransplant), renal, cardiac, and hepatic transplant patients had mean MPA AUCs approximately 20% to 41% lower and mean Cmax approximately 32% to 44% lower compared to the late transplant period (3 to 6 months posttransplant).
Mean MPA AUC values following administration of 1 g bid intravenous mycophenolate mofetil over 2 hours to renal transplant patients for 5 days were about 24% higher than those observed after oral administration of a similar dose in the immediate posttransplant phase. In hepatic transplant patients, administration of 1 g bid intravenous mycophenolate mofetil followed by 1.5 g bid oral mycophenolate mofetil resulted in mean MPA AUC values similar to those found in renal transplant patients administered 1 g mycophenolate mofetil bid.
Two 500 mg tablets have been shown to be bioequivalent to four 250 mg capsules. Five mL of the 200 mg/mL constituted oral suspension have been shown to be bioequivalent to four 250 mg capsules.
Special Populations
Shown below are the mean (±SD) pharmacokinetic parameters for MPA following the administration of oral mycophenolate mofetil given as single doses to non-transplant subjects with renal or hepatic impairment.
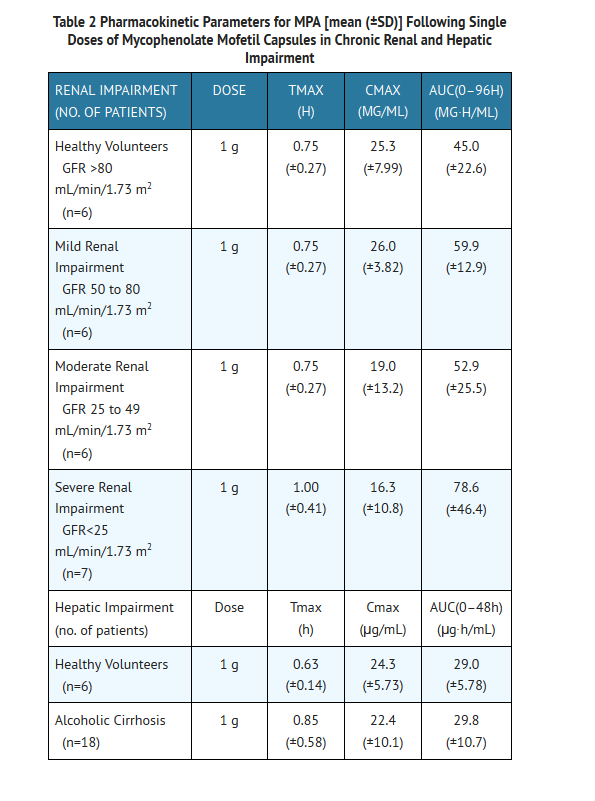
Renal Insufficiency
In a single-dose study, MMF was administered as capsule or intravenous infusion over 40 minutes. Plasma MPA AUC observed after oral dosing to volunteers with severe chronic renal impairment [glomerular filtration rate (GFR) <25 mL/min/1.73 m2] was about 75% higher relative to that observed in healthy volunteers (GFR >80 mL/min/1.73 m2). In addition, the single-dose plasma MPAG AUC was 3-fold to 6-fold higher in volunteers with severe renal impairment than in volunteers with mild renal impairment or healthy volunteers, consistent with the known renal elimination of MPAG. No data are available on the safety of long-term exposure to this level of MPAG.
Plasma MPA AUC observed after single-dose (1 g) intravenous dosing to volunteers (n=4) with severe chronic renal impairment (GFR<25 mL/min/1.73 m2) was 62.4 µg∙h/mL (±19.3). Multiple dosing of mycophenolate mofetil in patients with severe chronic renal impairment has not been studied (see PRECAUTIONS: Patients with Renal Impairment and DOSAGE AND ADMINISTRATION).
In patients with delayed renal graft function posttransplant, mean MPA AUC(0–12h) was comparable to that seen in posttransplant patients without delayed renal graft function. There is a potential for a transient increase in the free fraction and concentration of plasma MPA in patients with delayed renal graft function. However, dose adjustment does not appear to be necessary in patients with delayed renal graft function. Mean plasma MPAG AUC(0–12h) was 2-fold to 3-fold higher than in posttransplant patients without delayed renal graft function (see PRECAUTIONS: Patients with Renal Impairment and DOSAGE AND ADMINISTRATION).
In 8 patients with primary graft non-function following renal transplantation, plasma concentrations of MPAG accumulated about 6-fold to 8-fold after multiple dosing for 28 days. Accumulation of MPA was about 1-fold to 2-fold.
The pharmacokinetics of mycophenolate mofetil are not altered by hemodialysis. Hemodialysis usually does not remove MPA or MPAG. At high concentrations of MPAG (>100 µg/mL), hemodialysis removes only small amounts of MPAG.
Hepatic Insufficiency In a single-dose (1 g oral) study of 18 volunteers with alcoholic cirrhosis and 6 healthy volunteers, hepatic MPA glucuronidation processes appeared to be relatively unaffected by hepatic parenchymal disease when pharmacokinetic parameters of healthy volunteers and alcoholic cirrhosis patients within this study were compared. However, it should be noted that for unexplained reasons, the healthy volunteers in this study had about a 50% lower AUC as compared to healthy volunteers in other studies, thus making comparisons between volunteers with alcoholic cirrhosis and healthy volunteers difficult. Effects of hepatic disease on this process probably depend on the particular disease. Hepatic disease with other etiologies, such as primary biliary cirrhosis, may show a different effect. In a single-dose (1 g intravenous) study of 6 volunteers with severe hepatic impairment (aminopyrine breath test less than 0.2% of dose) due to alcoholic cirrhosis, MMF was rapidly converted to MPA. MPA AUC was 44.1 µg∙h/mL (±15.5).
Pediatrics The pharmacokinetic parameters of MPA and MPAG have been evaluated in 55 pediatric patients (ranging from 1 year to 18 years of age) receiving mycophenolate mofetil oral suspension at a dose of 600 mg/m2 bid (up to a maximum of 1 g bid) after allogeneic renal transplantation. The pharmacokinetic data for MPA is provided in Table 3.
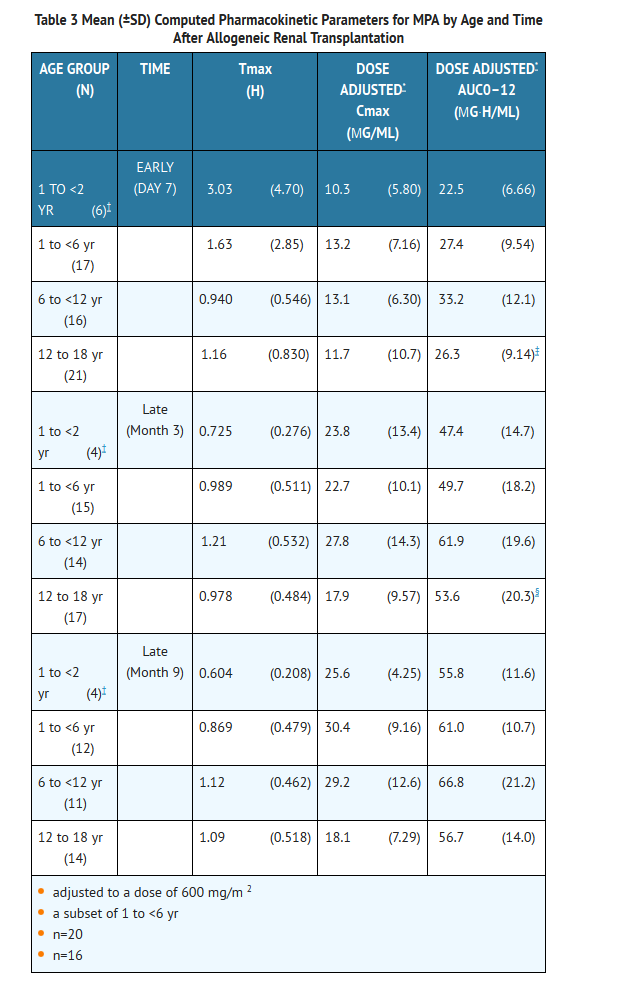
The mycophenolate mofetil oral suspension dose of 600 mg/m2 bid (up to a maximum of 1 g bid) achieved mean MPA AUC values in pediatric patients similar to those seen in adult renal transplant patients receiving mycophenolate mofetil capsules at a dose of 1 g bid in the early posttransplant period. There was wide variability in the data. As observed in adults, early posttransplant MPA AUC values were approximately 45% to 53% lower than those observed in the later posttransplant period (>3 months). MPA AUC values were similar in the early and late posttransplant period across the 1 year to 18 year age range.
Gender Data obtained from several studies were pooled to look at any gender-related differences in the pharmacokinetics of MPA (data were adjusted to 1 g oral dose). Mean (±SD) MPA AUC(0–12h) for males (n=79) was 32.0 (±14.5) and for females (n=41) was 36.5 (±18.8) µg∙h/mL while mean (±SD) MPA Cmax was 9.96 (±6.19) in the males and 10.6 (±5.64)µg/mL in the females. These differences are not of clinical significance.
Geriatrics Pharmacokinetics in the elderly have not been studied.
Nonclinical Toxicology
There is limited information regarding Nonclinical Toxicology of Mycophenolate in the drug label.
Clinical Studies
Adults The safety and efficacy of mycophenolate mofetil in combination with corticosteroids and cyclosporine for the prevention of organ rejection were assessed in randomized, double-blind, multicenter trials in renal (3 trials), in cardiac (1 trial), and in hepatic (1 trial) adult transplant patients.
Renal Transplant
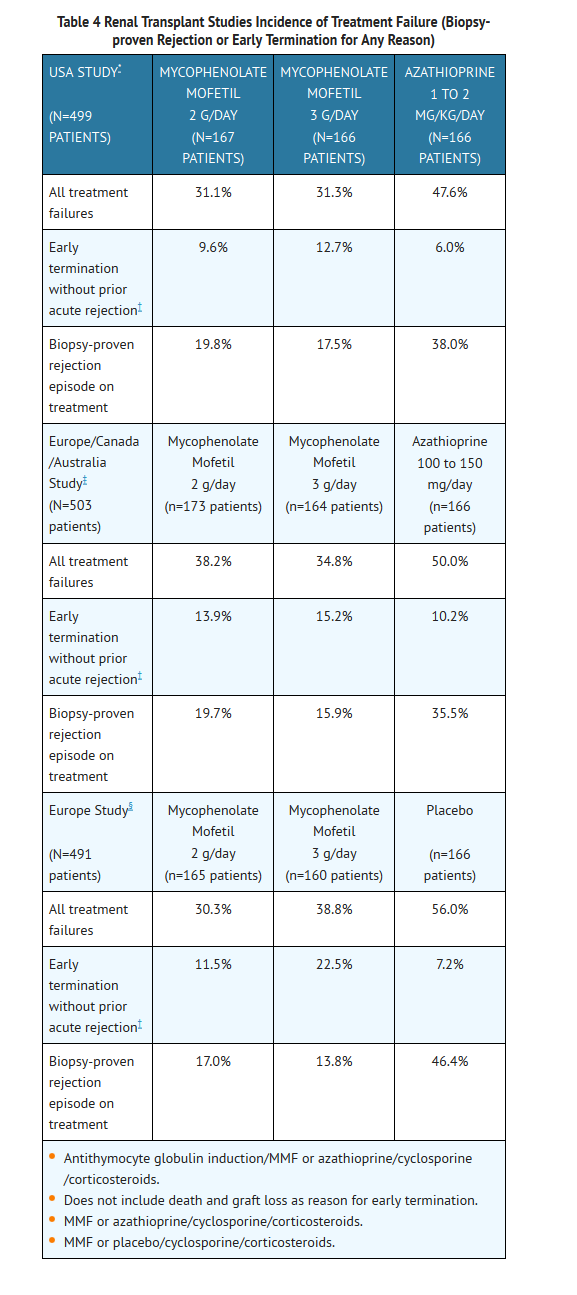
Adults The three renal studies compared two dose levels of oral mycophenolate mofetil (1 g bid and 1.5 g bid) with azathioprine (2 studies) or placebo (1 study) when administered in combination with cyclosporine (Sandimmune®) and corticosteroids to prevent acute rejection episodes. One study also included antithymocyte globulin (ATGAM®) induction therapy. These studies are described by geographic location of the investigational sites. One study was conducted in the USA at 14 sites, one study was conducted in Europe at 20 sites, and one study was conducted in Europe, Canada, and Australia at a total of 21 sites.
The primary efficacy endpoint was the proportion of patients in each treatment group who experienced treatment failure within the first 6 months after transplantation (defined as biopsy-proven acute rejection on treatment or the occurrence of death, graft loss or early termination from the study for any reason without prior biopsy-proven rejection). Mycophenolate mofetil, when administered with antithymocyte globulin (ATGAM®) induction (one study) and with cyclosporine and corticosteroids (all three studies), was compared to the following three therapeutic regimens: (1) antithymocyte globulin (ATGAM®) induction/azathioprine/cyclosporine/corticosteroids, (2) azathioprine/cyclosporine/corticosteroids, and (3) cyclosporine/corticosteroids.
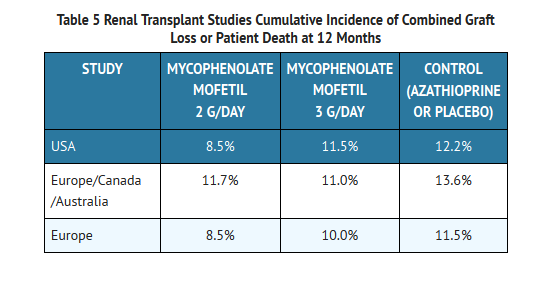
Mycophenolate mofetil, in combination with corticosteroids and cyclosporine reduced (statistically significant at 0.05 level) the incidence of treatment failure within the first 6 months following transplantation. Table 4 and Table 5 summarize the results of these studies. These tables show (1) the proportion of patients experiencing treatment failure, (2) the proportion of patients who experienced biopsy-proven acute rejection on treatment, and (3) early termination, for any reason other than graft loss or death, without a prior biopsy-proven acute rejection episode. Patients who prematurely discontinued treatment were followed for the occurrence of death or graft loss, and the cumulative incidence of graft loss and patient death are summarized separately. Patients who prematurely discontinued treatment were not followed for the occurrence of acute rejection after termination. More patients receiving mycophenolate mofetil discontinued without prior biopsy-proven rejection, death or graft loss than discontinued in the control groups, with the highest rate in the mycophenolate mofetil 3 g/day group. Therefore, the acute rejection rates may be underestimates, particularly in the mycophenolate mofetil 3 g/day group.
The cumulative incidence of 12-month graft loss or patient death is presented below. No advantage of mycophenolate mofetil with respect to graft loss or patient death was established. Numerically, patients receiving mycophenolate mofetil 2 g/day and 3 g/day experienced a better outcome than controls in all three studies; patients receiving mycophenolate mofetil 2 g/day experienced a better outcome than mycophenolate mofetil 3 g/day in two of the three studies. Patients in all treatment groups who terminated treatment early were found to have a poor outcome with respect to graft loss or patient death at 1 year.
Pediatrics
One open-label, safety and pharmacokinetic study of mycophenolate mofetil oral suspension 600 mg/m2 bid (up to 1 g bid) in combination with cyclosporine and corticosteroids was performed at centers in the US (9), Europe (5) and Australia (1) in 100 pediatric patients (3 months to 18 years of age) for the prevention of renal allograft rejection. Mycophenolate mofetil was well tolerated in pediatric patients (see ADVERSE REACTIONS), and the pharmacokinetics profile was similar to that seen in adult patients dosed with 1 g bid mycophenolate mofetil capsules (see CLINICAL PHARMACOLOGY: Pharmacokinetics). The rate of biopsy-proven rejection was similar across the age groups (3 months to <6 years, 6 years to <12 years, 12 years to 18 years). The overall biopsy-proven rejection rate at 6 months was comparable to adults. The combined incidence of graft loss (5%) and patient death (2%) at 12 months posttransplant was similar to that observed in adult renal transplant patients.
Cardiac Transplant
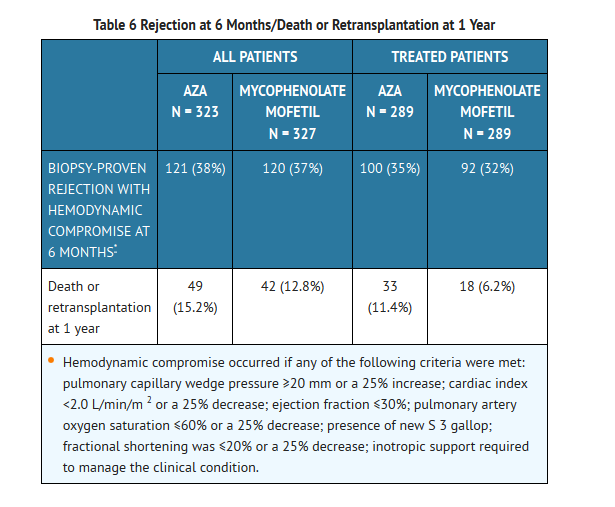
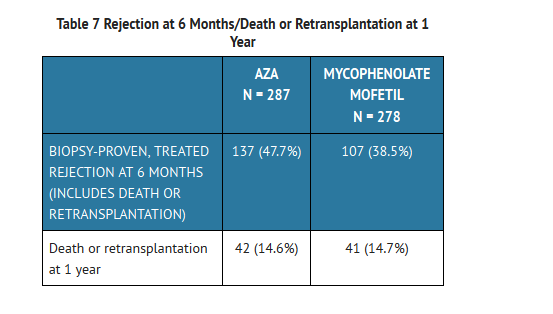
A double-blind, randomized, comparative, parallel-group, multicenter study in primary cardiac transplant recipients was performed at 20 centers in the United States, 1 in Canada, 5 in Europe and 2 in Australia. The total number of patients enrolled was 650; 72 never received study drug and 578 received study drug. Patients received mycophenolate mofetil 1.5 g bid (n=289) or azathioprine 1.5 to 3 mg/kg/day (n=289), in combination with cyclosporine (Sandimmune® or Neoral®) and corticosteroids as maintenance immunosuppressive therapy. The two primary efficacy endpoints were: (1) the proportion of patients who, after transplantation, had at least one endomyocardial biopsy-proven rejection with hemodynamic compromise, or were retransplanted or died, within the first 6 months, and (2) the proportion of patients who died or were retransplanted during the first 12 months following transplantation. Patients who prematurely discontinued treatment were followed for the occurrence of allograft rejection for up to 6 months and for the occurrence of death for 1 year.
1 Rejection: No difference was established between mycophenolate mofetil and azathioprine (AZA) with respect to biopsy-proven rejection with hemodynamic compromise.
2 Survival: Mycophenolate mofetil was shown to be at least as effective as AZA in preventing death or retransplantation at 1 year (see Table 6).
Hepatic Transplant
A double-blind, randomized, comparative, parallel-group, multicenter study in primary hepatic transplant recipients was performed at 16 centers in the United States, 2 in Canada, 4 in Europe and 1 in Australia. The total number of patients enrolled was 565. Per protocol, patients received mycophenolate mofetil 1 g bid intravenously for up to 14 days followed by mycophenolate mofetil 1.5 g bid orally or azathioprine 1 to 2 mg/kg/day intravenously followed by azathioprine 1 to 2 mg/kg/day orally, in combination with cyclosporine (Neoral®) and corticosteroids as maintenance immunosuppressive therapy. The actual median oral dose of azathioprine on study was 1.5 mg/kg/day (range of 0.3 to 3.8 mg/kg/day) initially and 1.26 mg/kg/day (range of 0.3 to 3.8 mg/kg/day) at 12 months. The two primary endpoints were: (1) the proportion of patients who experienced, in the first 6 months posttransplantation, one or more episodes of biopsy-proven and treated rejection or death or retransplantation, and (2) the proportion of patients who experienced graft loss (death or retransplantation) during the first 12 months posttransplantation. Patients who prematurely discontinued treatment were followed for the occurrence of allograft rejection and for the occurrence of graft loss (death or retransplantation) for 1 year.
Results In combination with corticosteroids and cyclosporine, mycophenolate mofetil obtained a lower rate of acute rejection at 6 months and a similar rate of death or retransplantation at 1 year compared to azathioprine.
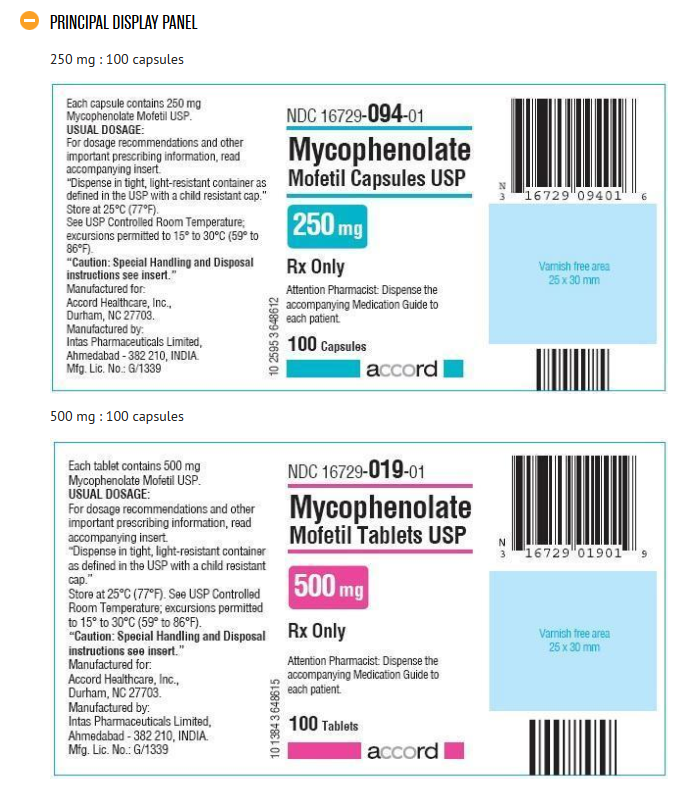
How Supplied
Mycophenolate Mofetil Capsules USP 250 mg
Light blue/peach, size ‘1’ hard gelatin capsules, printed in black with ‘GC1’ on body containing white to off white powder.
NDC Number Size
NDC 16729-094-01 Bottle of 100
NDC 16729-094-29 Bottle of 120
NDC 16729-094-16 Bottle of 500
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Mycophenolate Mofetil Tablets USP 500 mg
Purple coloured, capsule shaped,biconvex film-coated tablets debossed ‘AHI ’ on one side and ‘500 ’ on other side.
NDC Number Size
NDC 16729-019-01 Bottle of 100
NDC 16729-019-16 Bottle of 500
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Dispense in light-resistant containers, such as the manufacturer's original containers.
Images
Drug Images
{{#ask: Page Name::Mycophenolate |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Mycophenolate |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Mycophenolate in the drug label.
Precautions with Alcohol
- Alcohol-Mycophenolate interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- ®[1]
Look-Alike Drug Names
- A® — B®[2]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Empty citation (help)
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Mycophenolate
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Mycophenolate |Label Name=Mycophenolate11.png
}}
{{#subobject:
|Label Page=Mycophenolate |Label Name=Mycophenolate11.png
}}