Mitral regurgitation echocardiography
| Resident Survival Guide |
|
Mitral Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Mitral regurgitation echocardiography On the Web |
|
American Roentgen Ray Society Images of Mitral regurgitation echocardiography |
|
Risk calculators and risk factors for Mitral regurgitation echocardiography |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Varun Kumar, M.B.B.S. [3]; Lakshmi Gopalakrishnan, M.B.B.S. [4]; Mohammed A. Sbeih, M.D.[5]; Yamuna Kondapally, M.B.B.S[6]
Overview
Transthoracic echocardiography (TTE) should be performed in a patient with suspected mitral regurgitation (MR) to confirm the diagnosis and to establish the baseline severity of disease. It should then be performed to monitor the course of disease over time. Color doppler flow on the TTE will reveal a jet of blood flowing from the left ventricle into the left atrium during ventricular systole. Echocardiographic features that suggest severe MR include systolic reversal of flow in the pulmonary veins and filling of the entire left atrial cavity by the regurgitant jet of MR.
Echocardiography
Transthoracic echocardiography (TTE) is the diagnostic modality of choice to evaluate mitral regurgitation. TEE allows the evaluation of the following:[1][2]
- Left ventricle structure and function
- Right ventricle structure and function
- The structures of the mitral valve and the underlying etiology of mitral regurgitation
- Leaflet perforation
- Chordal rupture
- Rupture of the papillary muscle
- Valvular vegetations
- Pulmonary artery pressure
- The severity of the mitral regurgitation through the measurement of:
- Effective orifice area
- Regurgitant volume
- Regurgitant fraction
When TTE is non diagnostic in the setting of acute MR and there is a clinical suspicion of MR, transesophageal echocardiography (TEE) must be performed particularly among myocardial infarction patients with acute hemodynamic deterioration in the context of a normally contracting left ventricle.[1]
Intraoperative TEE is routinely performed among patients undergoing mitral valve surgery in order to further identify the anatomy of the valve.[1]
Determination of the Underlying Cause of Mitral Regurgitation on Echocardiography
Mitral Valve Prolapse / Myxomatous Mitral Valve
- Mitral valve prolapse (MVP) is currently the most common cause of mitral regurgitation in the Western world. Echocardiography in MVP demonstrates thick and redundant leaflets and chordae tendinae. The echocardiographic criteria for the diagnosis of MVP include:
- Movement of any part of either leaflet more than 2 mm behind the annular plane in parasternal long axis view and
- Movement of the point of coaptation behind the annular plane in the apical 4 chamber view
- Over time, the poor tensile strength of the chordae leads to their progressive elongation and/or rupture. Ruptured chordae tendinae appear as flail segments.
Rheumatic Mitral Regurgitation
- Commissural fusion and thickening of the leaflets are visible and there is restricted movement of the leaflets.
Annular Calcification
- Normally, the mitral annulus contracts during systole, and mitral annular calcification makes the annulus more rigid and impairs its contraction.
- There is increased echogenicity on the LV side immediately adjacent to the attachment of the posterior mitral valve leaflet.
- The region of the annulus adjacent to the anterior mitral leaflet is rarely involved. The anterior region can be involved in elderly subjects and younger patients with chronic renal failure and hypertension.
Ischemic Mitral Regurgitation
- Ischemia can cause mitral regurgitation via regional left ventricular dysfunction due to abnormal contraction of the papillary muscle and/or the underlying left ventricular wall. Ischemic MR occurs during exertion while MR associated with myocardial infarction occurs at rest.
Papillary Muscle Rupture
- Most often this is a complication of myocardial infarction. If the entire papillary muscle is disconnected from the left ventricle, then severe MR results and the patient rarely survives. Partial rupture is more common and carries a more favorable prognosis.
Functional Mitral Regurgitation
Functional MR is due to dilation of the mitral valve apparatus as a result of LV dilatation and systolic dysfunction in the presence of a structurally normal mitral valve apparatus.
Echocardiographic Monitoring
Echocardiography is performed for follow up among asymptomatic patients with MR to assess the left ventricular ejection fraction (LVEF) and end-systolic dimension. The frequency of follow up with an echocardiogram among asymptomatic patients with MR and normal LVEF is as follows:[1]
- Mild MR: Every 3-5 years
- Moderate MR: Every 1-2 years
- Severe MR: Every 6-12 months (the frequency increases if the the LV dilatation increases)
Assessment of Severity of Mitral Regurgitation
Click here for details about the staging of mitral regurgitation by severity.
- The degree of severity of mitral regurgitation can be quantified by the percentage of the left ventricular stroke volume that regurgitates into the left atrium (the regurgitant fraction).
- The echocardiographic technique to measure the regurgitant fraction is to determine the forward flow through the mitral valve (from the left atrium to the left ventricle) during ventricular diastole, and comparing it with the flow out of the left ventricle through the aortic valve in ventricular systole.
- This method assumes that the aortic valve does not suffer from aortic insufficiency. The regurgitant fraction would be described as:
Regurgitant fraction = { (Vmitral - Vaortic) ÷ Vmitral } x 100% where Vmitral and Vaortic are respectively the volumes of blood that flow forward through the mitral valve and aortic valve during a cardiac cycle.
- Another way to quantify the degree of mitral regurgitation is to determine the area of the regurgitant flow at the level of the valve. This is known as the regurgitant orifice area, and correlates with the size of the defect in the mitral valve.
- One particular echocardiographic technique used to measure the orifice area is measurement of the proximal isovelocity surface area (PISA). The flaw of using PISA to determine the mitral valve regurgitant orifice area is that it measures the flow at one moment in time in the cardiac cycle, which may not reflect the average performance of the regurgitant jet.
- If the left ventricular and left atrial sizes are normal on echocardiography, mitral regurgitation is not severe.
- Central jets indicate the presence of a fairly normal mitral valve and therefore the mitral regurgitation is not severe. Wide eccentric jets indicate that the regurgitation is severe.
- Echocardiographic findings must match the symptoms, if they do not, perform transesophageal echocardiography (TEE) or cardiac catheterization. TTE can underestimate the magnitude of mitral regurgitation in patients with clinical signs of severe MR.
Color Flow Mapping
- Size of flow recruitment is noted.
- Jet base width at the valve level.
- Intraatrial jet area if it is a central jet.
- Jet direction is usually away from a prolapsing leaflet and behind a restricted leaflet.
Continuous Wave Doppler
- Shape and density of signal - In severe Mitral regurgitation, the flow is dense and triangular.
- If as dense as forward flow, it is severe.
Pulse Wave Doppler(PW)
- PW in apical-4-chamber view.
- E wave more than 1.2m/s indicates severe MR.
- Even minor mitral stenosis or hyperdynamic circulation can increase E wave.
- If A-wave dominant, severe MR is virtually ruled out.
Vena Contracta
- Vena contracta is the narrowest region of regurgitant jet (usually just below the valve in LA).
- >0.7 cm - severe MR.
Pulmonary Venous Flow
- Usually forward throughout cycle.
- Systolic dominant
- As MR worsens, there is a blunting of systolic flow.
- If severe MR - systolic flow reversal.
Regurgitant Volume
- Mitral regurgitant volume = Mitral inflow volume - LV outflow volume.
- Mitral inflow volume = Vti * Cross sectional area of mitral valve.
- LV outflow volume = Vti * Cross sectional area at LV outflow.
- Regurtitant volume - <20% - mild , >50% severe
PISA (Proximal Isovelocity Surface Area)
The radius of Proximal isovelocity surface area or flow convergence zone which is a 3-dimensional surface area proximal to a narrowed orifice at which all the blood velocities are equal, can be used to calculate the severity of mitral regurgitation. The principle is that if the mitral regurgitation is mild, only the blood nearer to the valve orifice accelerates towards the atrium while in severe regurgitation, blood farther away from the valve moves back.
PISA radius
A simple method to determine severity of mitral regurgitation is to measure the PISA radius. Regurgitation is mild if radius is <0.4 cm and severe if >1 cm.
Regurgitant Flow (Instantaneous)
The instantaneous regurgitant flow can be calculated from the PISA radius and can be used to assess the severity of mitral regurgitation.
Regurgitant flow = 2π * r2 * Valiasing
Effective Regurgitant Orifice Area (EROA)
Effective regurgitant orifice area can be calculated using the instantaneous regurgitant flow. The formula can be derived from the following:
Valiasing * 2πr2 = Vmax * EROA
hence:
- EROA = PISA (2πr2) * Valiasing / Vmax
Mild = 0-20 cm2, moderate = 20 - 40 cm2, severe = >40 cm2
Regurgitant volume can be calculated from this.
- Regurgitant volume = Effective regurgitant orifice area * Vtime integrale
Echocardiographic Examples of Mitral Regurgitation
Shown below is an echocardiography image depicting flail posterior mitral leaflet.
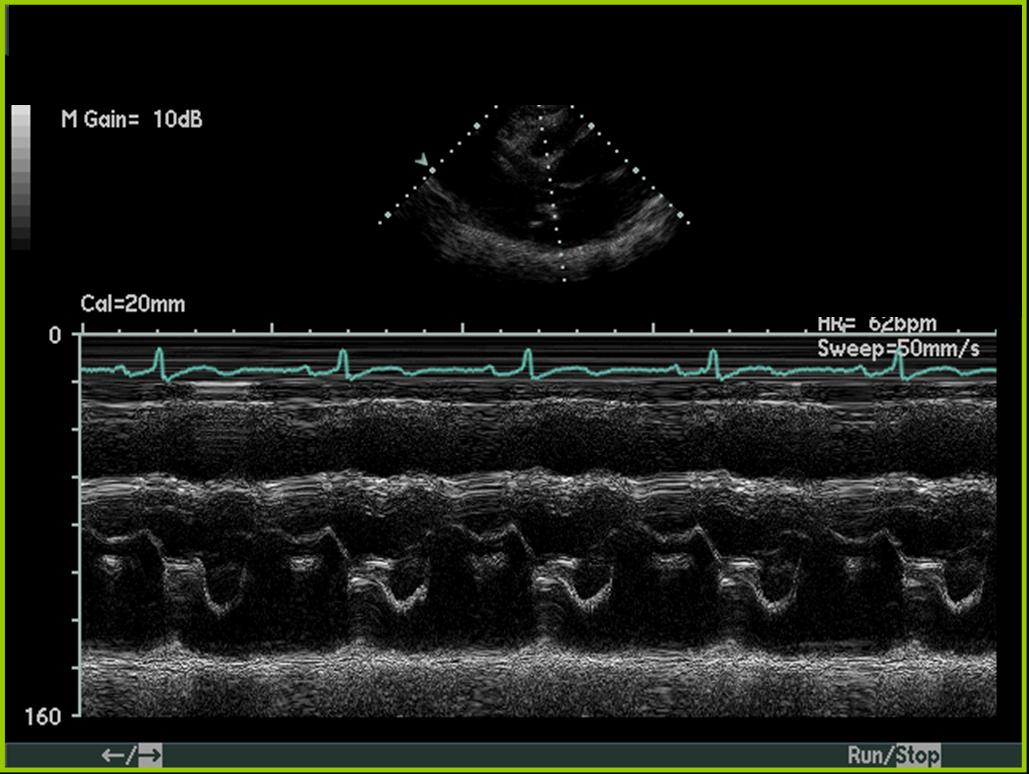 |
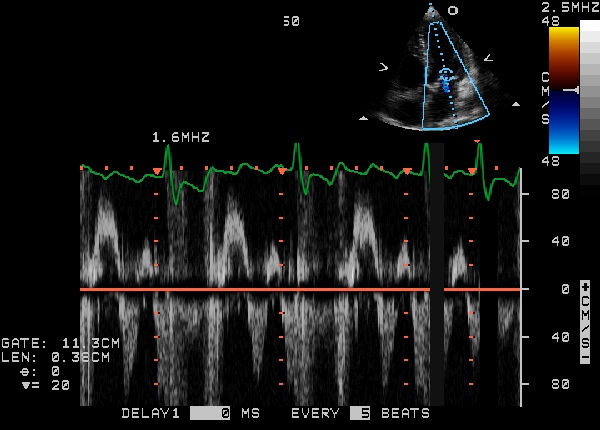
Shown below is an echocardiography image of pulmonary vein pulsed wave Doppler depicting severe MR from ring dehiscence.
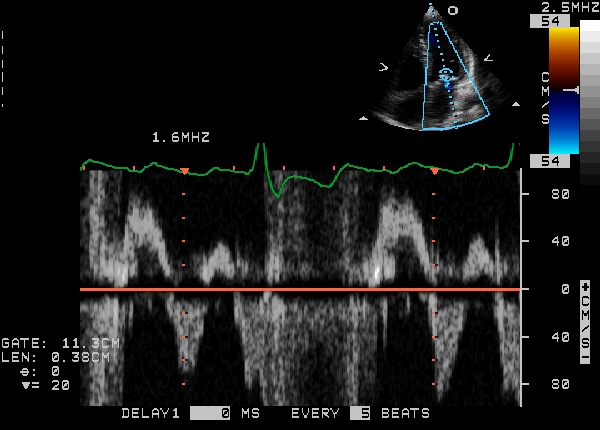
Shown below is an echocardiography image of pulmonary vein pulsed wave Doppler depicting severe MR pulmonary vein pulsed wave Doppler.
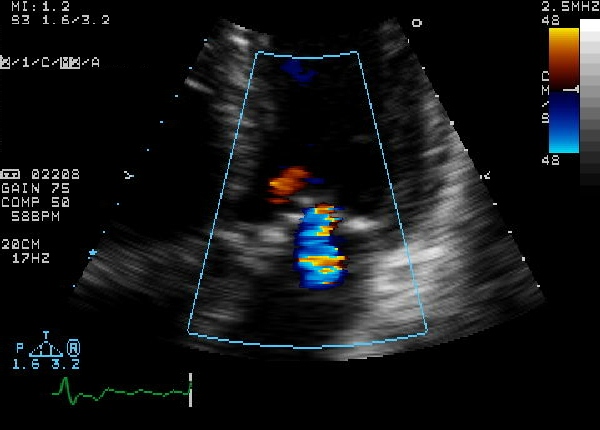
Shown below are echocardiography images depicting diastolic MR secondary to severe aortic stenosis.
2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines[3]
Recommendations for Diagnostic Testing: Initial Diagnosis of Chronic MR Referenced studies that support the recommendations are summarized in Online Data Supplement
| Class I |
| 1. In patients with known or suspected primary MR, TTE is indicated for baseline evaluation of LV size and function, RV function, LA size, pulmonary artery pressure, and the mechanism and severity of primary MR (Stages A to D) (Level of Evidence: B-NR)
2. In patients with primary MR, when TTE provides insufficient or discordant information, TEE is indicated for evaluation of the severity of MR, mechanism of MR, and status of LV function (Stages B to D). (Level of Evidence: B-NR) 4. In patients with severe primary MR undergoing mitral intervention, intraoperative TEE is indicated to establish the anatomic basis for primary MR (Stages C and D) and to guide repair. (Level of Evidence: B-NR) |
Recommendation for Diagnostic Testing: Changing Signs or Symptoms in Patients With Primary MR Referenced studies that support the recommendation are summarized in Online Data Supplement
| Class I |
| 1. In patients with primary MR (Stages B to D) and new-onset or changing symptoms, TTE is indicated to evaluate the mitral valve apparatus and LV function.(Level of Evidence: B-NR) |
Recommendations for Diagnostic Testing: Routine Follow-Up for Chronic Primary MR Referenced studies that support the recommendations are summarized in Online Data Supplement
| Class I |
| 1. For asymptomatic patients with severe primary MR (Stages B and C1), TTE is indicated every 6 to 12 months for surveillance of LV function (estimated by LVEF, LVEDD, and LVESD) and assessment of pulmonary artery pressure |
Recommendation for Diagnostic Testing: Exercise Testing for Chronic Primary MR Referenced studies that support the recommendation are summarized in Online Data Supplement
| Class IIa |
| 1. In patients with primary MR (Stages B and C) and symptoms that might be attributable to MR, hemodynamic exercise testing using Doppler echocardiography or cardiac catheterization or cardiopulmonary exercise testing is reasonable. (Level of Evidence: B-NR) |
Recommendations for Diagnosis of Secondary MR Referenced studies that support the recommendations are summarized in Online Data Supplement
| Class I |
| 1. In patients with chronic secondary MR (Stages B to D), TTE is useful to establish the etiology and to assess the extent of regional and global LV remodeling and systolic dysfunction, severity of MR, and magnitude of pulmonary hypertension(Level of Evidence: B-NR)
2. In patients with chronic secondary MR (Stages B to D), noninvasive imaging (stress nuclear/PET, CMR, or stress echocardiography), coronary CT angiography, or coronary arteriography is useful to establish etiology of MR and to assess myocardial viability(Level of Evidence: C-EO) 3. In patients with chronic secondary MR with severe symptoms (Stage D) that are unresponsive to GDMT who are being considered for transcatheter mitral valve interventions, TEE is indicated to determine suitability for the procedure.(Level of Evidence: B-NR) 4. In patients with chronic secondary MR undergoing transcatheter mitral valve intervention, intraprocedural guidance with TEE is recommended(Level of Evidence: C-EO) |
2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary[1]
Recommendations for Chronic Primary Mitral Regurgitation
| Class I |
| "1. Transthoracic echocardiography (TTE) is indicated for baseline evaluation of LV size and function, right ventricular (RV) function and left atrial size, pulmonary artery pressure, and mechanism and severity of primary MR (stages A to D) in any patient suspected of having chronic primary MR. (Level of Evidence: B) " |
| "2. Intraoperative transesophageal echocardiography (TEE) is indicated to establish the anatomic basis for chronic primary MR (stages C and D) and to guide repair. (Level of Evidence: B) " |
| "3. TEE is indicated for evaluation of patients with chronic primary MR (stages B to D) in whom noninvasive imaging provides nondiagnostic information about severity of MR, mechanism of MR, and/or status of LV function. (Level of Evidence: C) " |
Recommendations for Chronic Secondary Mitral Regurgitation
| Class I |
| "1. Transthoracic echocardiography (TTE) is useful to establish the etiology of chronic secondary MR (stages B to D) and the extent and location of wall motion abnormalities and to assess global LV function, severity of MR and magnitude of pulmonary hypertension. (Level of Evidence: C) " |
2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) [4]
Transthoracic Echocardiography Indications (DO NOT EDIT) [4]
| Class I |
| "1. Transthoracic echocardiography is indicated for baseline evaluation of LV size and function, RV and left atrial size, pulmonary artery pressure, and severity of MR in any patient suspected of having MR.(Level of Evidence: C) " |
| "2. Transthoracic echocardiography is indicated for delineation of the mechanism of MR.(Level of Evidence: B) " |
| "3. Transthoracic echocardiography is indicated for annual or semiannual surveillance of LV function (estimated by ejection fraction and end-systolic dimension) in asymptomatic patients with moderate to severe MR.(Level of Evidence: C) " |
| "4. Transthoracic echocardiography is indicated in patients with MR to evaluate the mitral valve apparatus and LV function after a change in signs or symptoms.(Level of Evidence: C) " |
| "5. Transthoracic echocardiography is indicated to evaluate LV size and function and MVhemodynamics in the initial evaluation after mitral valve replacement or mitral valve repair.(Level of Evidence: C) " |
| Class III |
| "1. Transthoracic echocardiography is not indicated for routine follow-up evaluation of asymptomatic patients with mild MR and normal LV size and systolic function.(Level of Evidence: C) " |
| Class IIa |
| "1. Exercise Doppler echocardiography is reasonable in asymptomatic patients with severe MR to assess exercise tolerance and the effects of exercise on pulmonary artery pressure and MR severity.(Level of Evidence: C) " |
Transesophageal Echocardiography Indications (DO NOT EDIT) [5]
| Class I |
| "1. Preoperative or intraoperative transesophageal echocardiography is indicated to establish the anatomic basis for severe MR in patients in whom surgery is recommended to assess feasibility of repair and to guide repair.(Level of Evidence: B) " |
| "2. Transesophageal echocardiography is indicated for evaluation of MR patients in whom [[transthoracic echocardiography] provides nondiagnostic information regarding severity of MR, mechanism of MR, and/or status of LV function.(Level of Evidence: B) " |
| Class III |
| "1. Transesophageal echocardiography is not indicated for routine follow-up or surveillance of asymptomatic patients with native valve [[MR].(Level of Evidence: C) " |
| Class IIa |
| "1. Preoperative transesophageal echocardiography is reasonable in asymptomatic patients with severe MR who are considered for surgery to assess feasibility of repair.(Level of Evidence: C) " |
Sources
- 2008 Focused Update Incorporated Into the ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease [4]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. 129 (23): 2440–92. doi:10.1161/CIR.0000000000000029. PMID 24589852.
- ↑ Enriquez-Sarano M, Akins CW, Vahanian A (2009). "Mitral regurgitation". Lancet. 373 (9672): 1382–94. doi:10.1016/S0140-6736(09)60692-9. PMID 19356795.
- ↑ Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, Gentile F; et al. (2021). "2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines". Circulation. 143 (5): e72–e227. doi:10.1161/CIR.0000000000000923. PMID 33332150 Check
|pmid=value (help). - ↑ 4.0 4.1 4.2 Bonow RO, Carabello BA, Chatterjee K; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172. Unknown parameter
|month=ignored (help) - ↑ Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD; et al. (2008). "2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". J Am Coll Cardiol. 52 (13): e1–142. doi:10.1016/j.jacc.2008.05.007. PMID 18848134.

