Membranous glomerulonephritis: Difference between revisions
No edit summary |
m (Bot: Automated text replacement (-Category:Primary care +)) |
||
| (8 intermediate revisions by 7 users not shown) | |||
| Line 6: | Line 6: | ||
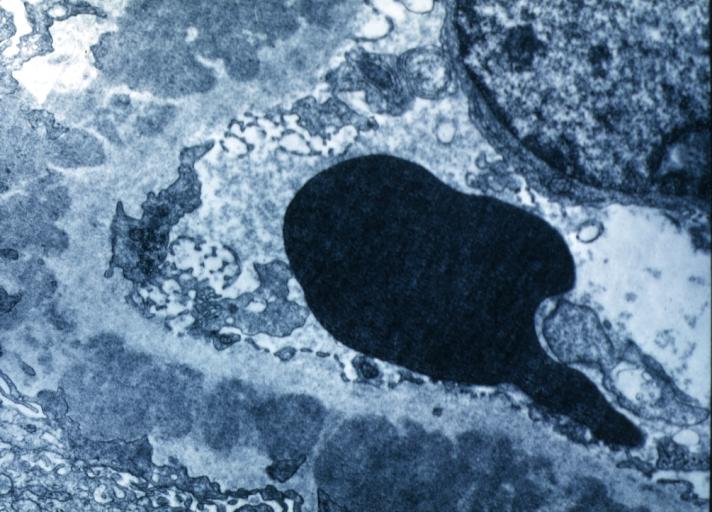
Caption = Membranous Glomerulonephritis: Electron micrography. An excellent example to show thickened basement membrane and immune complexes. <br> <small> [http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] </small> | | Caption = Membranous Glomerulonephritis: Electron micrography. An excellent example to show thickened basement membrane and immune complexes. <br> <small> [http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] </small> | | ||
DiseasesDB = 7970 | | DiseasesDB = 7970 | | ||
ICD10 = | ICD10 = | | ||
ICD9 = {{ICD9|583.1}} | | ICD9 = {{ICD9|583.1}} | | ||
ICDO = | | ICDO = | | ||
| Line 14: | Line 14: | ||
}} | }} | ||
{{Membranous glomerulonephritis}} | {{Membranous glomerulonephritis}} | ||
{{CMG}} | {{CMG}}; '''Associate Editor-In-Chief:''' {{SAH}} {{CZ}} {{HK}} {{JSS}} | ||
{{SK}} Extramembranous glomerulopathy; Heymann nephritis; idiopathic membranous glomerulonephritis; idiopathic membranous nephropathy; membranous glomerulonephropathy; membranous glomerulopathy; membranous nephropathy; nephropathy, membranous | |||
==[[Membranous glomerulonephritis overview|Overview]]== | |||
==[[Membranous glomerulonephritis historical perspective|Historical Perspective]]== | |||
==[[Membranous glomerulonephritis classification|Classification]]== | |||
==[[Membranous glomerulonephritis pathophysiology|Pathophysiology]]== | |||
==[[Membranous glomerulonephritis causes|Causes]]== | |||
==[[ | ==[[Membranous glomerulonephritis differential diagnosis|Differentiating Membranous glomerulonephritis from other Diseases]]== | ||
==[[Membranous glomerulonephritis epidemiology and demographics|Epidemiology and Demographics]]== | |||
==[[ | ==[[Membranous glomerulonephritis risk factors|Risk Factors]]== | ||
==[[Membranous glomerulonephritis screening|Screening]]== | |||
== | |||
==[[Membranous glomerulonephritis natural history, complications and prognosis|Natural History, Complications and Prognosis]]== | |||
==Diagnosis== | |||
[[Membranous glomerulonephritis history and symptoms|History and Symptoms]] | [[Membranous glomerulonephritis physical examination|Physical Examination]] | [[Membranous glomerulonephritis laboratory findings|Laboratory Findings]] | [[Membranous glomerulonephritis renal biopsy|Renal Biopsy]] | [[Membranous glomerulonephritis light microscopy|Light Microscopy]] | [[Membranous glomerulonephritis CT|CT]] | [[Membranous glomerulonephritis immunofluorescence microscopy|Immunofluorescence Microscopy]] | [[Membranous glomerulonephritis ultrasound|Ultrasound]] | [[Membranous glomerulonephritis other imaging findings|Other Imaging Findings]] | [[Membranous glomerulonephritis other diagnostic studies|Other Diagnostic Studies]] | |||
==Treatment== | ==Treatment== | ||
[[Membranous glomerulonephritis medical therapy|Medical Therapy]] | [[Membranous glomerulonephritis surgery|Surgery]] | [[Membranous glomerulonephritis primary prevention|Primary Prevention]] | [[Membranous glomerulonephritis secondary prevention|Secondary Prevention]] | [[Membranous glomerulonephritis cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Membranous glomerulonephritis future or investigational therapies|Future or Investigational Therapies]] | |||
==Case Studies== | |||
=== | |||
[[Membranous glomerulonephritis case study one|Case #1]] | |||
{{Nephrology}} | {{Nephrology}} | ||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
[[Category:Medicine]] | |||
[[Category:Nephrology]] | [[Category:Nephrology]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Radiology]] | |||
[[ | |||
[[ | |||
Latest revision as of 06:34, 28 July 2020
For patient information page, click here
| Membranous glomerulonephritis | |
 | |
|---|---|
| Membranous Glomerulonephritis: Electron micrography. An excellent example to show thickened basement membrane and immune complexes. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-9 | 583.1 |
| DiseasesDB | 7970 |
| MeSH | D015433 |
|
Membranous glomerulonephritis Microchapters |
|
Differentiating Membranous glomerulonephritis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Membranous glomerulonephritis On the Web |
|
American Roentgen Ray Society Images of Membranous glomerulonephritis |
|
Directions to Hospitals Treating Membranous glomerulonephritis |
|
Risk calculators and risk factors for Membranous glomerulonephritis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Syed Ahsan Hussain, M.D.[2] Cafer Zorkun, M.D., Ph.D. [3] Syed Hassan A. Kazmi BSc, MD [4] Jogeet Singh Sekhon, M.D. [5]
Synonyms and keywords: Extramembranous glomerulopathy; Heymann nephritis; idiopathic membranous glomerulonephritis; idiopathic membranous nephropathy; membranous glomerulonephropathy; membranous glomerulopathy; membranous nephropathy; nephropathy, membranous
Overview
Historical Perspective
Classification
Pathophysiology
Causes
Differentiating Membranous glomerulonephritis from other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications and Prognosis
Diagnosis
History and Symptoms | Physical Examination | Laboratory Findings | Renal Biopsy | Light Microscopy | CT | Immunofluorescence Microscopy | Ultrasound | Other Imaging Findings | Other Diagnostic Studies
Treatment
Medical Therapy | Surgery | Primary Prevention | Secondary Prevention | Cost-Effectiveness of Therapy | Future or Investigational Therapies