Mastoiditis pathophysiology
|
Mastoiditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mehrian Jafarizade, M.D [2]
Overview
Mastoiditis refers to an infection that occurs in the cavities of the mastoid process of temporal bone after otitis media. At birth, the mastoid consists of a single cavity, which is connected to the middle ear by a canal. As the child grows, the mastoid bone becomes pneumatized, resulting in a series of connected cavities, lined by a mucosa derived from respiratory epithelium. The connection between the middle ear, the eustachian tube, and the mastoid has a fundamental role in the pathogenesis of mastoiditis. In the setting of acute otitis media, the mucosa that lines the middle ear and also mastoid air cells becomes inflamed. In a majority of cases of acute otitis media inflammation resolves; when it persists, it leads to bacterial and fluid accumulation within the mastoid air cells. Gradually, as a result of pressure rising in the mastoid, air cell septae may be destroyed and mastoiditis could proceed to periostitis, cavity abscess, and osteomyelitis. The mastoid is near vital organs in the head and neck and mastoid infection may cause serious complications. There is evidence of a genetic predisposition to recurrent otitis media and therefore mastoiditis, with statistically significant evidence that it has high heritability. The following genes have been identified as having potential pathogenic qualities for otitis media: CAPN14, GALNT14, BPIFA3, BPIFA1, BMP5, GALNT13, NELL1, TGFB3.
Pathogenesis
Mastoiditis is the infection in the cavities of mastoid process of temporal bone that occurs after otitis media. At birth, the mastoid consists of a single cavity, which is connected to the middle ear by a canal. As the child grows, the mastoid bone becomes pneumatized, resulting in a series of connected cavities, lined by a mucosa derived from respiratory epithelium. There is a relationship between the middle ear, eustachian tube, and the mastoid. This connection has a fundamental role in the pathogenesis of mastoiditis. In the setting of acute otitis media, the mucosa that lines the middle ear and also mastoid air cells becomes inflamed. In majority of cases of acute otitis media, the inflammation resolves, but some persist leading to bacterial and fluid accumulation within the mastoid air cells. Gradually, as a result of pressure rising in the mastoid, air cell septae may be destroyed and mastoiditis could proceed to periostitis, cavity abscess, and osteomyelitis.
- Mastoid is near important structures like the facial nerve, sternocleidomastoid muscle, jugular vein, internal carotid artery, sigmoid sinus, brain, and meninges; as a result of this proximity, spread of infection to these places may cause complications.[1][2]
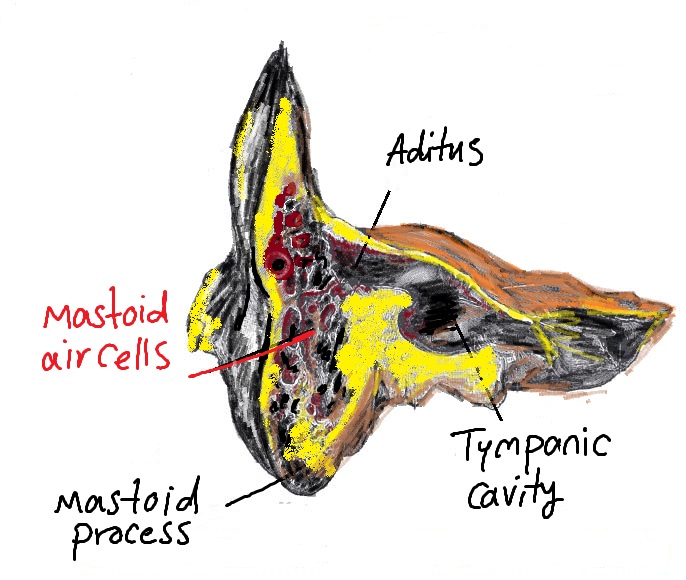
Below shows connection of the tympanic membrane and mastoid ear cells:
Transmission
Mastoiditis results from the extension of adjacent infection in the middle ear.
Genetics
- There is evidence of a genetic predisposition to recurrent otitis media, and thereby mastoiditis, with statistically significant evidence that it has high heritability.[3]
- Hereditary factors comprise 45-75% of risk factors for recurrent otitis media, as revealed by heritability studies involving twins and triplets.[4]
- The following genes have been identified as having potential pathogenic qualities for recurrent otitis media and mastoiditis:[4][2]
- 2p23.1
- CAPN14
- GALNT14
- 20q11.21
- BPIFA3
- BPIFA1
- Those that interact with the TGFβ pathway:
- BMP5
- GALNT13
- NELL1
- TGFB3
- 2p23.1
- Upregulation of the genes correlated to recurrent otitis media pathogenesis, contributes to individual susceptibility to mastoiditis.
Associated Conditions
- Mastoiditis is often associated with other upper respiratory conditions caused by the nasopharyngeal pathogen, including:[5][2]
- Allergy-related conditions, such as allergic rhinitis, are also associated with mastoiditis.
Gross Pathology
Gross pathological findings of mastoiditis may include:[6]
- Clouded appearance of tympanic membrane
- Presence of exudate
- Obliteration of external ear canal
- Pus
Microscopic Pathology
Microscopic pathological findings in mastoiditis may include the following:[6]
- Neutrophilic exudate seen in mastoid cavities
- Prominent dilated blood vessels
- Edema and focal inflammation
References
- ↑ Lin HW, Shargorodsky J, Gopen Q (2010). "Clinical strategies for the management of acute mastoiditis in the pediatric population". Clin Pediatr (Phila). 49 (2): 110–5. doi:10.1177/0009922809344349. PMID 19734439.
- ↑ 2.0 2.1 2.2 Pang LH, Barakate MS, Havas TE (2009). "Mastoiditis in a pediatricc population: a review of 11 years experience in management". Int. J. Pediatr. Otorhinolaryngol. 73 (11): 1520–4. doi:10.1016/j.ijporl.2009.07.003. PMID 19758711.
- ↑ Hafrén L, Kentala E, Järvinen TM, Leinonen E, Onkamo P, Kere J, Mattila PS (2012). "Genetic background and the risk of otitis media". Int. J. Pediatr. Otorhinolaryngol. 76 (1): 41–4. doi:10.1016/j.ijporl.2011.09.026. PMID 22018929.
- ↑ 4.0 4.1 Rye MS, Warrington NM, Scaman ES, Vijayasekaran S, Coates HL, Anderson D, Pennell CE, Blackwell JM, Jamieson SE (2012). "Genome-wide association study to identify the genetic determinants of otitis media susceptibility in childhood". PLoS ONE. 7 (10): e48215. doi:10.1371/journal.pone.0048215. PMC 3485007. PMID 23133572.
- ↑ Coticchia JM, Chen M, Sachdeva L, Mutchnick S (2013). "New paradigms in the pathogenesis of otitis media in children". Front Pediatr. 1: 52. doi:10.3389/fped.2013.00052. PMC 3874850. PMID 24400296.
- ↑ 6.0 6.1 Liao YJ, Liu TC (2013). "Images in clinical medicine. Mastoiditis". N. Engl. J. Med. 368 (21): 2014. doi:10.1056/NEJMicm1205007. PMID 23697516.