Mantle cell lymphoma pathophysiology
|
Mantle cell lymphoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Mantle cell lymphoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Mantle cell lymphoma pathophysiology |
|
Risk calculators and risk factors for Mantle cell lymphoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ali Akram, M.B.B.S.[2] Sowminya Arikapudi, M.B,B.S. [3]
Overview
Pathophysiology
Pathogenesis
- The translocation t(11;14)(q13;q32) is considered the precipitating oncogenic event that induces cell cycle deregulation due to overexpression of cyclin D1.
- This translocation juxtaposes the CCDN1 gene encoding cyclin D1 to the immunoglobulin heavy chain (IgH) leading to its overexpression. However, less commonly, mutations in CCDN2 and CCDN3 have also been identified in cases of mantle cell lymphoma lacking the t(11;14) translocation.[1]
- In addition to the pathogonomic translocation, MCL progression is controlled by secondary genetic abberations and dysregulated signaling pathways involved in DNA damage response, proliferation, and apoptosis.[2]
Genetics
Genes involved in the pathogenesis of mantle cell lymphoma include:
- CCDN1 (primarily)
- CCDN2 (less frequently)
- CCDN3 (less frequently)
Gross Pathology
On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Microscopic Pathology
On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
References
- ↑ Itziar Salaverria, Cristina Royo, Alejandra Carvajal-Cuenca, Guillem Clot, Alba Navarro, Alejandra Valera, Joo Y. Song, Renata Woroniecka, Grzegorz Rymkiewicz, Wolfram Klapper, Elena M. Hartmann, Pierre Sujobert, Iwona Wlodarska, Judith A. Ferry, Philippe Gaulard, German Ott, Andreas Rosenwald, Armando Lopez-Guillermo, Leticia Quintanilla-Martinez, Nancy L. Harris, Elaine S. Jaffe, Reiner Siebert, Elias Campo & Silvia Bea (2013). "CCND2 rearrangements are the most frequent genetic events in cyclin D1(-) mantle cell lymphoma". Blood. 121 (8): 1394–1402. doi:10.1182/blood-2012-08-452284. PMID 23255553. Unknown parameter
|month=ignored (help) - ↑ Patricia Perez-Galan, Martin Dreyling & Adrian Wiestner (2011). "Mantle cell lymphoma: biology, pathogenesis, and the molecular basis of treatment in the genomic era". Blood. 117 (1): 26–38. doi:10.1182/blood-2010-04-189977. PMID 20940415. Unknown parameter
|month=ignored (help)
Overview
Development of mantle cell lymphoma is the result of (non-inherited) genetic mutations in somatic cells. Mantle cell lymphoma cells generally over-express cyclin D1 due to a t(11:14)[1] chromosomal translocation in the DNA. Cells affected by mantle cell lymphoma proliferate in a nodular or diffuse pattern with two main cytologic variants: typical or blastic.
Microscopic pathology
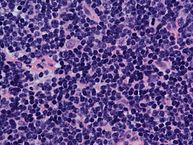
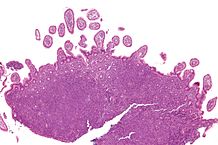
Cells affected by mantle cell lymphoma proliferate in a nodular or diffuse pattern with two main cytologic variants: typical or blastic.
- Typical cases are small to intermediate sized cells with irregular nuclei.
- Blastic (aka blastoid) variants have intermediate to large sized cells with finely dispersed chromatin and are more aggressive in nature.
The tumor cells accumulate in the lymphoid system, including lymph nodes and the spleen, with non-useful cells eventually rendering the system dysfunctional. Mantle cell lymphoma may also replace normal cells in the bone marrow, which impairs normal blood cell production.
-
Intermediate magnification micrograph of mantle cell lymphoma of the terminal ileum. Endoscopic biopsy. H&E stain. Histomorphologic features: Monomorphic small lymphoid cells less than twice the size of a resting lymphocyte. Abundant mitoses. Sclerosed blood vessels. Scattered epithelioid histiocytes.
-
Mantle cell lymphoma. Notice the irregular nuclear contours of the medium-sized lymphoma cells and the presence of a pink histiocyte. By immunohistochemistry the lymphoma cells expressed CD20, CD5 and Cyclin D1 (high power view, H&E).
-
Lymph node with mantle cell lymphoma (low power view, H&E).
-
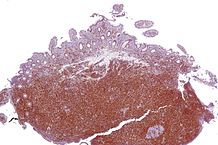
Micrograph of terminal ileum with mantle cell lymphoma (bottom of image). H&E stain.
-
Micrograph of terminal ileum with mantle cell lymphoma (bottom of image - brown colour). Cyclin D1 immunostain.