Mantle cell lymphoma pathophysiology
|
Mantle cell lymphoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Mantle cell lymphoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Mantle cell lymphoma pathophysiology |
|
Risk calculators and risk factors for Mantle cell lymphoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ali Akram, M.B.B.S.[2] Sowminya Arikapudi, M.B,B.S. [3]
Overview
Pathophysiology
Pathogenesis
The translocation t(11;14)(q13;q32) is considered the precipitating oncogenic event that induces cell cycle deregulation due to overexpression of cyclin D1. This translocation juxtaposes the CCDN1 gene encoding cyclin D1 to the immunoglobulin heavy chain (IgH) leading to its overexpression. However, less commonly, mutations in CCDN2 and CCDN3 have also been identified in cases of mantle cell lymphoma lacking the t(11;14) translocation.[1]
Genetics
Genes involved in the pathogenesis of mantle cell lymphoma include:
- CCDN1 (primarily)
- CCDN2 (less frequently)
- CCDN3 (less frequently)
Associated Conditions
Conditions associated with [disease name] include:
- [Condition 1]
- [Condition 2]
- [Condition 3]
Gross Pathology
On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Microscopic Pathology
On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
References
- ↑ Itziar Salaverria, Cristina Royo, Alejandra Carvajal-Cuenca, Guillem Clot, Alba Navarro, Alejandra Valera, Joo Y. Song, Renata Woroniecka, Grzegorz Rymkiewicz, Wolfram Klapper, Elena M. Hartmann, Pierre Sujobert, Iwona Wlodarska, Judith A. Ferry, Philippe Gaulard, German Ott, Andreas Rosenwald, Armando Lopez-Guillermo, Leticia Quintanilla-Martinez, Nancy L. Harris, Elaine S. Jaffe, Reiner Siebert, Elias Campo & Silvia Bea (2013). "CCND2 rearrangements are the most frequent genetic events in cyclin D1(-) mantle cell lymphoma". Blood. 121 (8): 1394–1402. doi:10.1182/blood-2012-08-452284. PMID 23255553. Unknown parameter
|month=ignored (help)
Overview
Development of mantle cell lymphoma is the result of (non-inherited) genetic mutations in somatic cells. Mantle cell lymphoma cells generally over-express cyclin D1 due to a t(11:14)[1] chromosomal translocation in the DNA. Cells affected by mantle cell lymphoma proliferate in a nodular or diffuse pattern with two main cytologic variants: typical or blastic.
Pathophysiology
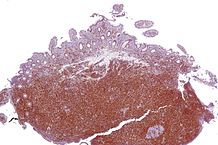
Mantle cell lymphoma is a subtype of B-cell lymphoma, due to CD5 positive antigen-naive pregerminal center B-cell within the mantle zone that surrounds normal germinal center follicles. Mantle cell lymphoma cells generally over-express cyclin D1 due to a t(11:14)[1] chromosomal translocation in the DNA.
Genetics
Mantle cell lymphoma, like most malignancies, results from the acquisition of a combination of (non-inherited) genetic mutations in somatic cells. This leads to a clonal expansion of malignant B lymphocytes. The factors that initiate the genetic alterations are typically not identifiable, and usually occur in people with no particular risk factors for lymphoma development. Because it is an acquired genetic disorder, mantle cell lymphoma is neither communicable nor inheritable. A defining characteristic of mantle cell lymphoma is mutation and overexpression of cyclin D1, a cell cycle gene, that contributes to the abnormal proliferation of the malignant cells. Mantle cell lymphoma cells may also be resistant to drug induced apoptosis, making them harder to cure with chemotherapy or radiation.
Microscopic pathology
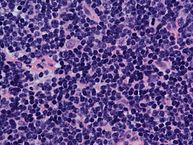
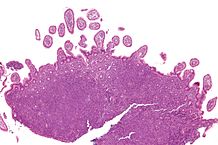
Cells affected by mantle cell lymphoma proliferate in a nodular or diffuse pattern with two main cytologic variants: typical or blastic.
- Typical cases are small to intermediate sized cells with irregular nuclei.
- Blastic (aka blastoid) variants have intermediate to large sized cells with finely dispersed chromatin and are more aggressive in nature.
The tumor cells accumulate in the lymphoid system, including lymph nodes and the spleen, with non-useful cells eventually rendering the system dysfunctional. Mantle cell lymphoma may also replace normal cells in the bone marrow, which impairs normal blood cell production.
-
Intermediate magnification micrograph of mantle cell lymphoma of the terminal ileum. Endoscopic biopsy. H&E stain. Histomorphologic features: Monomorphic small lymphoid cells less than twice the size of a resting lymphocyte. Abundant mitoses. Sclerosed blood vessels. Scattered epithelioid histiocytes.
-
Mantle cell lymphoma. Notice the irregular nuclear contours of the medium-sized lymphoma cells and the presence of a pink histiocyte. By immunohistochemistry the lymphoma cells expressed CD20, CD5 and Cyclin D1 (high power view, H&E).
-
Lymph node with mantle cell lymphoma (low power view, H&E).
-
Micrograph of terminal ileum with mantle cell lymphoma (bottom of image). H&E stain.
-
Micrograph of terminal ileum with mantle cell lymphoma (bottom of image - brown colour). Cyclin D1 immunostain.