Leptospirosis causes: Difference between revisions
No edit summary |
(→Causes) |
||
| Line 18: | Line 18: | ||
Humans become infected through contact with water, food, or soil containing urine from these infected animals. This may happen by swallowing contaminated food or water or through skin contact. The disease is not known to be spread from person to person and cases of bacterial dissemination in convalescence are extremely rare in humans. Leptospirosis is common among watersport enthusiasts in specific areas as prolonged immersion in water is known to promote the entry of the bacteria. Occupational risk factors include [[veterinarian]]s, slaughter house workers, farmers, and sewer workers. An outbreak in an inner city environment has been linked to contact with rat urine.<ref name=VCNA>{{cite journal|author=Heuter, Kerry J.,Langston, Cathy E.|title=Leptospirosis: A re-emerging zoonotic disease|journal=The Veterinary Clinics of North America|year=2003|volume=33|pages=791-807}}</ref> | Humans become infected through contact with water, food, or soil containing urine from these infected animals. This may happen by swallowing contaminated food or water or through skin contact. The disease is not known to be spread from person to person and cases of bacterial dissemination in convalescence are extremely rare in humans. Leptospirosis is common among watersport enthusiasts in specific areas as prolonged immersion in water is known to promote the entry of the bacteria. Occupational risk factors include [[veterinarian]]s, slaughter house workers, farmers, and sewer workers. An outbreak in an inner city environment has been linked to contact with rat urine.<ref name=VCNA>{{cite journal|author=Heuter, Kerry J.,Langston, Cathy E.|title=Leptospirosis: A re-emerging zoonotic disease|journal=The Veterinary Clinics of North America|year=2003|volume=33|pages=791-807}}</ref> | ||
{| border="2" cellpadding="4" cellspacing="0" style="margin: 1em 1em 1em 0; background: #f9f9f9; border: 1px #aaa solid; border-collapse: collapse;" width="75%" | |||
!colspan="1" style="background: #4479BA; text-align: center;" | {{fontcolor|#FFF| '''Species'''}} | |||
!colspan="1" style="background: #4479BA; text-align: center;" | {{fontcolor|#FFF| '''Serovar'''}} | |||
!colspan="1" style="background: #4479BA; text-align: center;" | {{fontcolor|#FFF|Reference strain}} | |||
!colspan="1" style="background: #4479BA; text-align: center;" | {{fontcolor|#FFF|Serogroup}} | |||
|- | |||
| | |||
|} | |||
==References== | ==References== | ||
Revision as of 14:32, 6 March 2017
|
Leptospirosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Leptospirosis causes On the Web |
|
American Roentgen Ray Society Images of Leptospirosis causes |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
For more information about Leptospira click here
Overview
Leptospirosis is caused by an infection with Leptospira. Several species of Leptospira have identified and have been classified, genotypically, which include both pathogenic and saprophytic species. Among the pathogenic species, over 300 serovars have been identified by serotyping methods.[1]
Causes
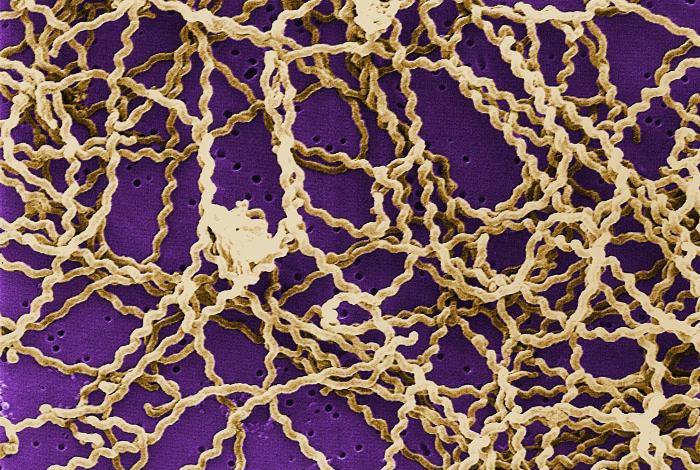
Leptospirosis is caused by a spirochaete bacterium called Leptospira spp. that has at 5 different serovars of importance in the United States causing disease (icterohaemorrhagiae, canicola, pomona, grippotyphosa, and bratislava).[2] There are other (less common) infectious strains. It should however be noted that genetically different leptospira organisms may be identical serologically and vice versa. Hence, an argument exists on the basis of strain identification. The traditional serologic system is seemingly more useful from diagnostic and epidemiologic standpoint at the moment (which may change with further development and spread of technologies like PCR).
Leptospirosis is transmitted by the urine of an infected animal, and is contagious as long as it is still moist. Although rats, mice and voles are important primary hosts, a wide range of other mammals including dogs, deer, rabbits, hedgehogs, cows, sheep, raccoons, possums, skunks, and even certain marine mammals are also able to carry and transmit the disease as secondary hosts. Dogs may lick the urine of an infected animal off the grass or soil, or drink from an infected puddle. There have been reports of "house dogs" contracting leptospirosis apparently from licking the urine of infected mice that entered the house. The type of habitats most likely to carry infective bacteria are muddy riverbanks, ditches, gulleys and muddy livestock rearing areas where there is regular passage of either wild or farm mammals. There is a direct correlation between the amount of rainfall and the incidence of leptospirosis, making it seasonal in temperate climates and year-round in tropical climates.
Leptospirosis is also transmitted by the semen of infected animals[3]. Abattoir workers can contract the disease through contact with infected blood or body fluids.
Humans become infected through contact with water, food, or soil containing urine from these infected animals. This may happen by swallowing contaminated food or water or through skin contact. The disease is not known to be spread from person to person and cases of bacterial dissemination in convalescence are extremely rare in humans. Leptospirosis is common among watersport enthusiasts in specific areas as prolonged immersion in water is known to promote the entry of the bacteria. Occupational risk factors include veterinarians, slaughter house workers, farmers, and sewer workers. An outbreak in an inner city environment has been linked to contact with rat urine.[2]
| Species | Serovar | Reference strain | Serogroup |
|---|---|---|---|
References
- ↑ Forbes AE, Zochowski WJ, Dubrey SW, Sivaprakasam V (2012). "Leptospirosis and Weil's disease in the UK". QJM. 105 (12): 1151–62. doi:10.1093/qjmed/hcs145. PMID 22843698.
- ↑ 2.0 2.1 Heuter, Kerry J.,Langston, Cathy E. (2003). "Leptospirosis: A re-emerging zoonotic disease". The Veterinary Clinics of North America. 33: 791–807.
- ↑ Kiktenko VS (1976). "Leptospirosis infection through insemination of animals". J Hyg Epidemiol Microbiol Immunol. 21 (2): 207-213.