Leiomyoma: Difference between revisions
No edit summary |
No edit summary |
||
| Line 3: | Line 3: | ||
{{CMG}} {{AE}} {{Ammu}}; {{SS}} | {{CMG}} {{AE}} {{Ammu}}; {{SS}} | ||
{{SK}} | {{SK}} Uterine myoma; Fibroid; Fibroids, Uterine; Fibroid Tumor; Fibroid Uterus; Fibromyoma | ||
==Overview== | ==Overview== | ||
Uterine leiomyoma was first discovered by Hippocrates, a greek physician also called as father of modern medicine in 460-375 B.C and called it “uterine stone”. Uterine leiomyoma may be classified according to their location into 3 subtypes: submucosal, subserous, and intramural. The pathogenesis of leiomyoma is characterized by [[benign]] [[smooth muscle]] [[neoplasm]]. They can occur in any organ, but the most common forms occur in the [[uterus]], [[small bowel]] and the [[esophagus]]. Chromosome aberrations such as t(12;14)(q14-q15;q23–24), del(7)(q22q32), rearrangements involving 6p21, 10q, trisomy 12, and deletions of 1p3q has been associated with the development of leiomyoma. Uterine leiomyoma must be differentiated from other diseases that cause uterine mass, such as:uterine adenomyoma, pregnancy, hematometra, uterine sarcoma, uterine carcinosarcoma, and metastasis. Leiomyoma is more commonly observed among patients aged 40 years and older. Common risk factors in the development of uterine leiomyoma are Afro-American race, early menarche, prenatal exposure to diethylstilbestrol, having one or more pregnancies extending beyond 20 weeks, obesity, significant consumption of beef and other reds meats, hypertension, family history, and alcohol consumption. Physical examination may be remarkable for enlarged, mobile uterus with an irregular contour on bimanual pelvic examination. The mainstay of therapy for uterine leiomyoma is oral contraceptive pills, either combination pills or progestin-only, [[Gonadotropin-releasing hormone analog]]s. Surgery is the mainstay of therapy for uterine leiomyoma. | Uterine leiomyoma was first discovered by Hippocrates, a greek physician also called as father of modern medicine in 460-375 B.C and called it “uterine stone”. Uterine leiomyoma may be classified according to their location into 3 subtypes: submucosal, subserous, and intramural. The pathogenesis of leiomyoma is characterized by [[benign]] [[smooth muscle]] [[neoplasm]]. They can occur in any organ, but the most common forms occur in the [[uterus]], [[small bowel]] and the [[esophagus]]. Chromosome aberrations such as t(12;14)(q14-q15;q23–24), del(7)(q22q32), rearrangements involving 6p21, 10q, trisomy 12, and deletions of 1p3q has been associated with the development of leiomyoma. Uterine leiomyoma must be differentiated from other diseases that cause uterine mass, such as:uterine adenomyoma, pregnancy, hematometra, uterine sarcoma, uterine carcinosarcoma, and metastasis. Leiomyoma is more commonly observed among patients aged 40 years and older. Common risk factors in the development of uterine leiomyoma are Afro-American race, early menarche, prenatal exposure to diethylstilbestrol, having one or more pregnancies extending beyond 20 weeks, obesity, significant consumption of beef and other reds meats, hypertension, family history, and alcohol consumption. Physical examination may be remarkable for enlarged, mobile uterus with an irregular contour on bimanual pelvic examination. The mainstay of therapy for uterine leiomyoma is oral contraceptive pills, either combination pills or progestin-only, [[Gonadotropin-releasing hormone analog]]s. Surgery is the mainstay of therapy for uterine leiomyoma. | ||
Revision as of 20:49, 19 April 2016
|
WikiDoc Resources for Leiomyoma |
|
Articles |
|---|
|
Most recent articles on Leiomyoma |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Leiomyoma at Clinical Trials.gov Clinical Trials on Leiomyoma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Leiomyoma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Leiomyoma Discussion groups on Leiomyoma Directions to Hospitals Treating Leiomyoma Risk calculators and risk factors for Leiomyoma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Leiomyoma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]; Sheng Shi, M.D. [3]
Synonyms and keywords: Uterine myoma; Fibroid; Fibroids, Uterine; Fibroid Tumor; Fibroid Uterus; Fibromyoma
Overview
Uterine leiomyoma was first discovered by Hippocrates, a greek physician also called as father of modern medicine in 460-375 B.C and called it “uterine stone”. Uterine leiomyoma may be classified according to their location into 3 subtypes: submucosal, subserous, and intramural. The pathogenesis of leiomyoma is characterized by benign smooth muscle neoplasm. They can occur in any organ, but the most common forms occur in the uterus, small bowel and the esophagus. Chromosome aberrations such as t(12;14)(q14-q15;q23–24), del(7)(q22q32), rearrangements involving 6p21, 10q, trisomy 12, and deletions of 1p3q has been associated with the development of leiomyoma. Uterine leiomyoma must be differentiated from other diseases that cause uterine mass, such as:uterine adenomyoma, pregnancy, hematometra, uterine sarcoma, uterine carcinosarcoma, and metastasis. Leiomyoma is more commonly observed among patients aged 40 years and older. Common risk factors in the development of uterine leiomyoma are Afro-American race, early menarche, prenatal exposure to diethylstilbestrol, having one or more pregnancies extending beyond 20 weeks, obesity, significant consumption of beef and other reds meats, hypertension, family history, and alcohol consumption. Physical examination may be remarkable for enlarged, mobile uterus with an irregular contour on bimanual pelvic examination. The mainstay of therapy for uterine leiomyoma is oral contraceptive pills, either combination pills or progestin-only, Gonadotropin-releasing hormone analogs. Surgery is the mainstay of therapy for uterine leiomyoma.
Historical Perspective
- Uterine leiomyoma was first discovered by Hippocrates, a greek physician also called as father of modern medicine in 460-375 B.C and called it “uterine stone”.
- In the second centruary of Christian era, Galen described the lesion as "scleromas".[1]
- In 1860 and 1863, Rokitansky and Klob coined the term fibroid.
- In 1854, Virchow a German pathologist demonstrated that those tumors originated from the uterine smooth muscle. Thus, the term "myoma" became current in clinical use.
- In 1809, the first laparotomy consequent to myoma indication was conducted by Ephraim McDowell to treat Leiomyoma in Danville, USA.
- The first successful myomectomy was performed by Amussat in 1840, after a clinical diagnosis of ovarian tumor because pelvic examination showed a pediculate and large uterine leiomyoma.
- The first scientific report of a uterus conserving myomectomy through the vagina appeared in 1845 in the American Journal of the Medical Science, accomplished by Washington Atlee, in Pennsylvania.
- In 1898, Alexander Adam presented 11 cases of myomectomy through an abdominal route, in Liverpool.
- In 1940, Carlos R. Círio proposed a technique of the myometrium emptying, called myometrectomy.
Classification
- Uterine leiomyoma may be classified according to their location into 3 subtypes:
- Submucosal – lie just beneath the endometrium.
- Intramural – lie within the uterine wall.
- Subserous – lies at the serosal surface of the uterus or may bulge out from the myometrium and can become pedunculated.
Pathophysiology
- The pathogenesis of leiomyoma is characterized by benign smooth muscle neoplasm. They can occur in any organ, but the most common forms occur in the uterus, small bowel and the esophagus.
- The chromosome aberrations such as t(12;14)(q14-q15;q23–24), del(7)(q22q32), rearrangements involving 6p21, 10q, trisomy 12, and deletions of 1p3q has been associated with the development of leiomyoma.[2]
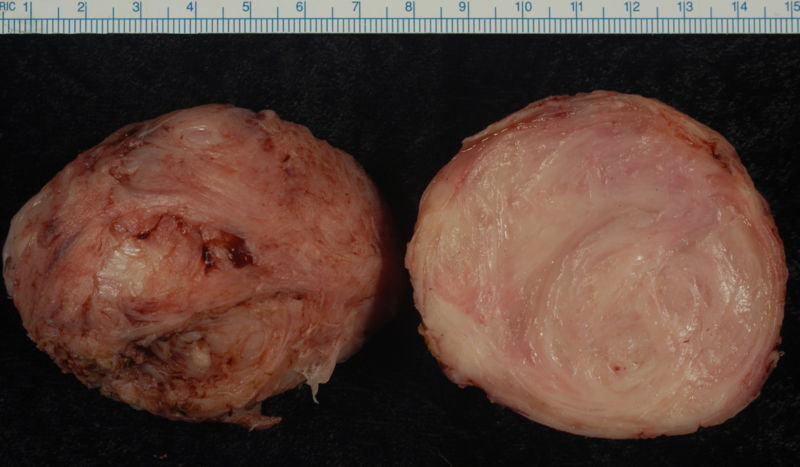
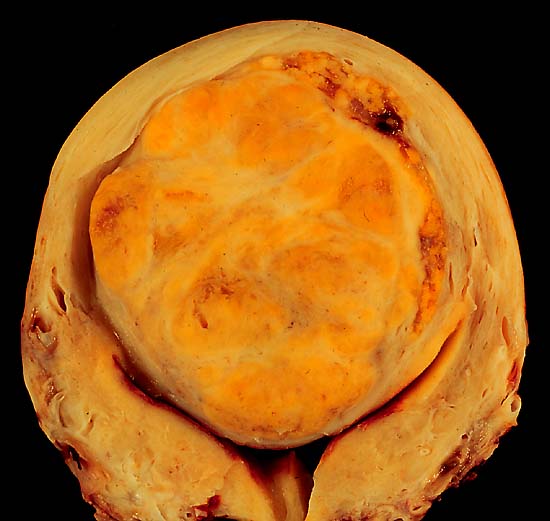
- On gross pathology, round, well circumscribed (but not encapsulated), solid nodules that are white or tan, and whorled are characteristic findings of leiomyoma .
- On microscopic histopathological analysis, elongated, spindle-shaped cells with a cigar-shaped nucleus are characteristic findings of leiomyoma.
Uterine Leiomyomata
Uterine fibroids are leiomyomata of the uterine smooth muscle. As other leiomyomata, they are benign, but may lead to excessive menstrual bleeding (menorrhagia), often cause anemia and may lead to infertility. Enucleation is removal of fibroids without removing the uterus (hysterectomy), which is also commonly performed. Laser surgery (called myolysis) is increasingly used, and provides a viable alternative to surgery. Estrogen and progesterone usually stimulate their growth, and hormone suppression may hence decrease their size.
Esophageal
They are also the most common benign esophageal tumour, though this accounts for less than 1% of esophageal neoplasms. The remainder consists mainly of carcinomas. Although the vast majority of benign esophageal tumors are clinically silent and go undetected, large or strategically located tumors may become symptomatic. [3]
Leiomyoma of Jejunum
Leiomyoma is the most common benign tumor of small bowel. Approximately 50% of cases are found in the jejunum, followed by the ileum in 31% of cases. Almost one half of all lesions are less than 5 centimeters. [4]
-
Leiomyoma enucleated from a uterus. External surface on left; cut surface on right
-
A large, solitary leiomyoma in the uterus, distoring the endometrial cavity into a Y shape by splaying and pressing it downwards.
(Image courtesy of Ed Uthman, MD)
Causes
- Chromosome aberrations such as t(12;14)(q14-q15;q23–24), del(7)(q22q32), rearrangements involving 6p21, 10q, trisomy 12, and deletions of 1p3q has been associated with the development of leiomyoma.
Differentiating Leiomyoma from other Diseases
- Uterine leiomyoma must be differentiated from other diseases that cause uterine mass, such as:
- Uterine adenomyoma
- Pregnancy
- Hematometra
- Uterine sarcoma
- Uterine carcinosarcoma
- Endometrial carcinoma
- Metastasis
Epidemiology and Demographics
Age
- Leiomyoma is more commonly observed among patients aged 40 years and older.
Race
- Leiomyoma usually affects individuals of the Afro-American women.
Risk Factors
- Common risk factors in the development of uterine leiomyoma are Afro-American race, early menarche, prenatal exposure to diethylstilbestrol, having one or more pregnancies extending beyond 20 weeks, obesity, significant consumption of beef and other reds meats, hypertension, family history, and alcohol consumption.
Natural History, Complications and Prognosis
- The majority of patients with uterine leiomyoma remain asymptomatic for 30s or 40s.
- Common complications of uterine leiomyoma include dysmenorrhea, dyspareunia, leiomyoma degeneration or torsion, transcervical prolapse, and miscarriage.
Diagnosis
Symptoms
- Leiomyoma is usually asymptomatic.
- Symptoms of uterine leiomyoma may include the following:
- Abnormal gynecologic hemorrhage
- Heavy or painful periods
- Abdominal discomfort or bloating
- Back ache
- Urinary frequency or retention
- Infertility
Physical Examination
- Physical examination may be remarkable for:
- Enlarged, mobile uterus with an irregular contour on bimanual pelvic examination
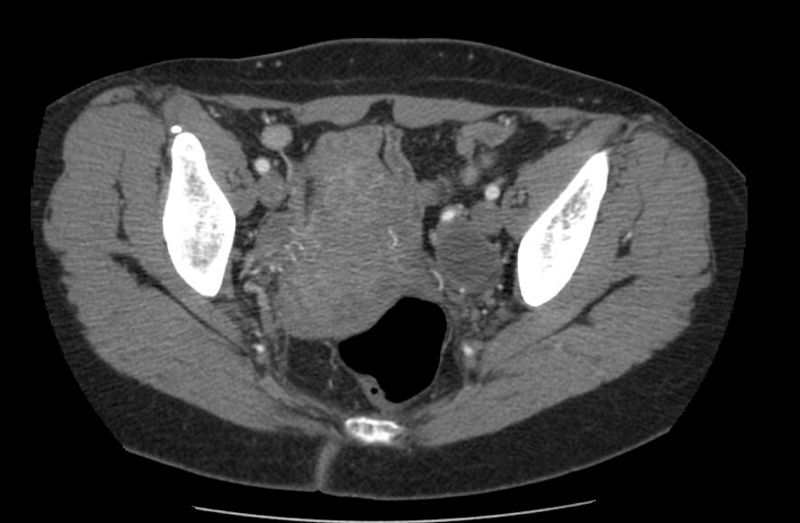
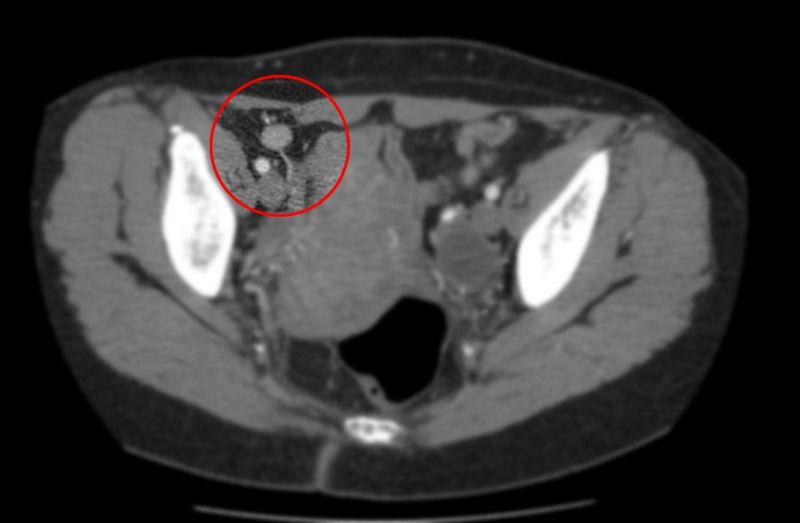
Imaging Findings
- On ultrasound imaging, uterine leiomyoma is characterized by the fibroids as focal masses with a heterogeneous texture, which usually cause shadowing of the ultrasound beam.
Other Diagnostic Studies
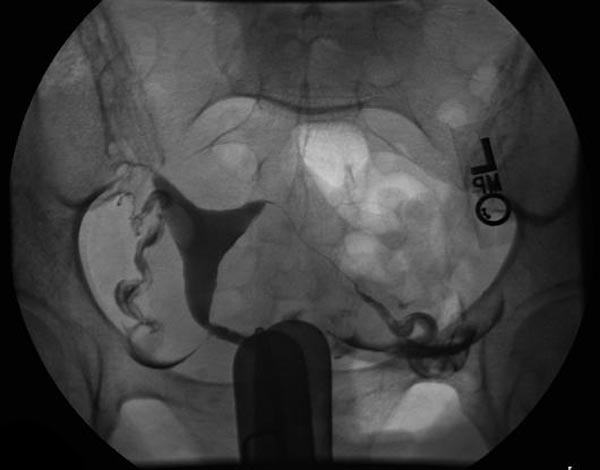
- Uterine leiomyoma may also be diagnosed using diagnostic hysteroscopy, magnetic resonance imaging, and hysterosalpingography.
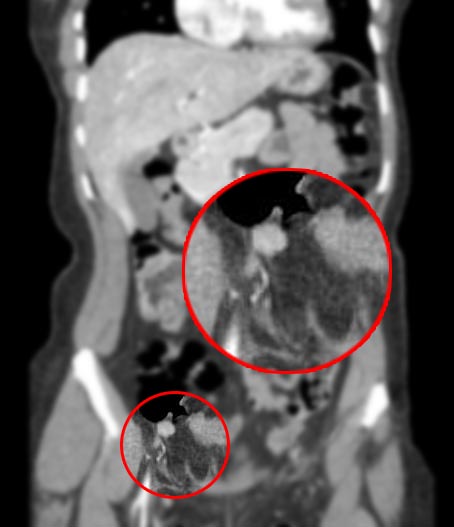
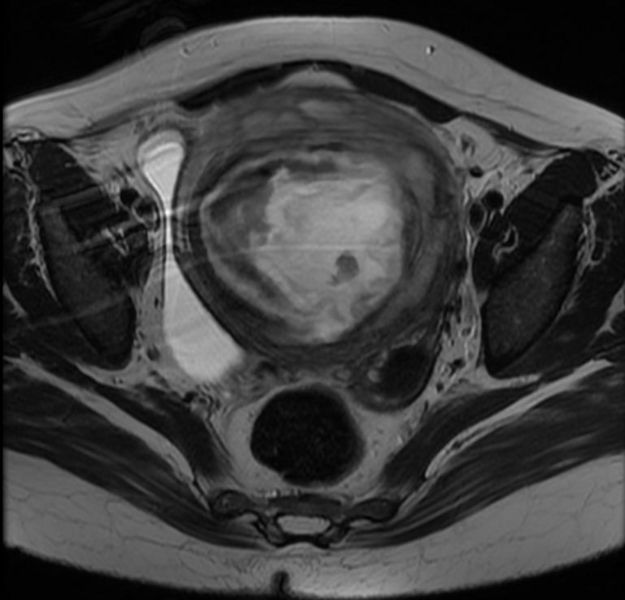
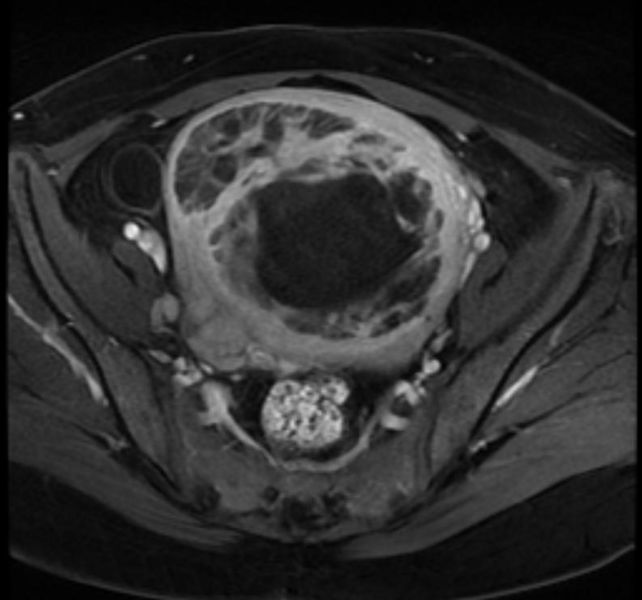
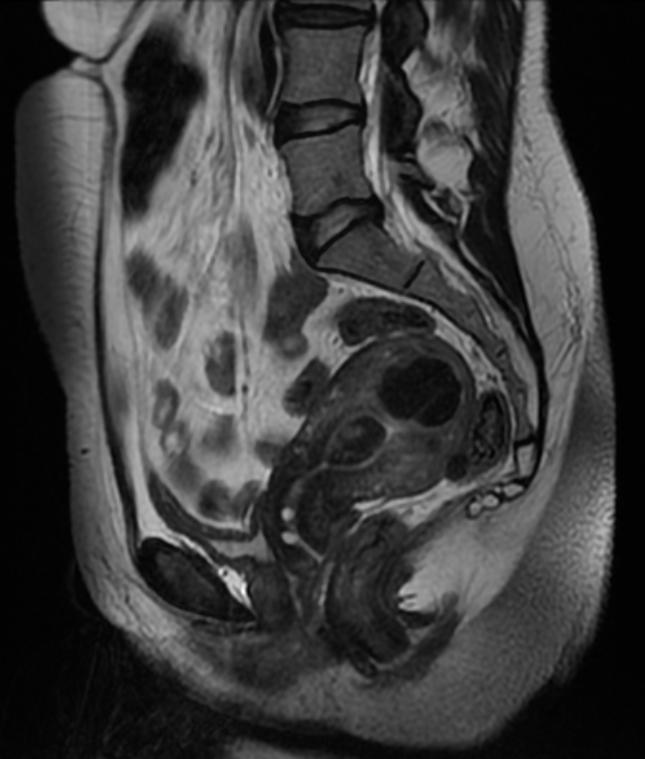
Patient #1: MR images demonstrate large degenerating leiomyomas
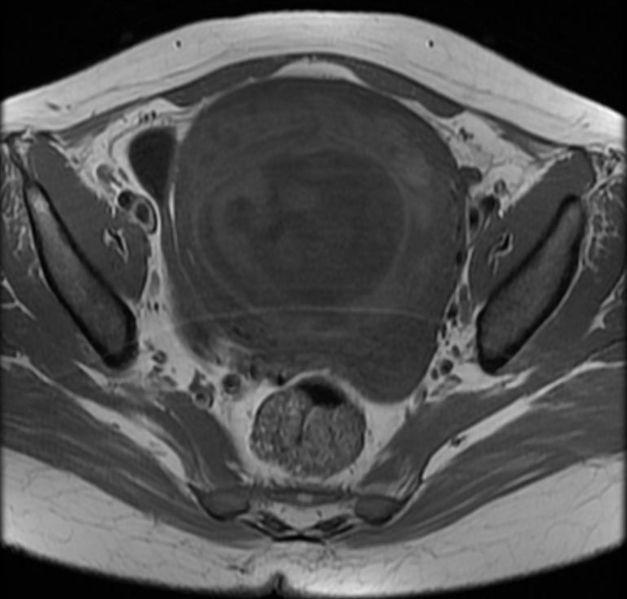
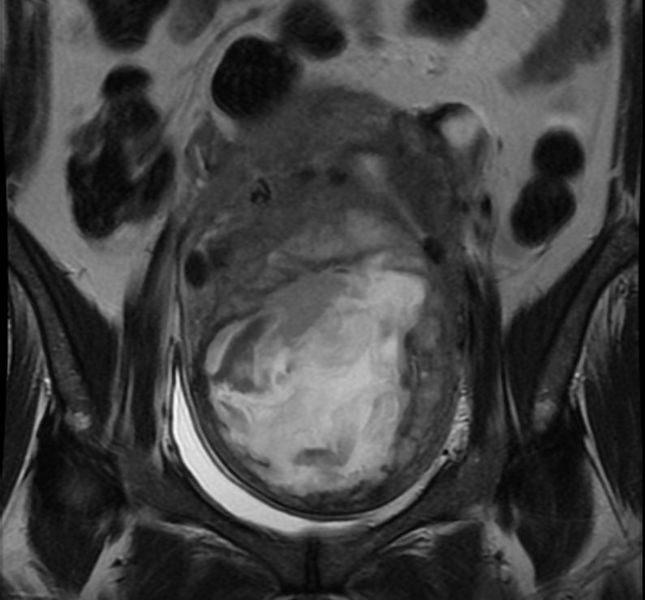
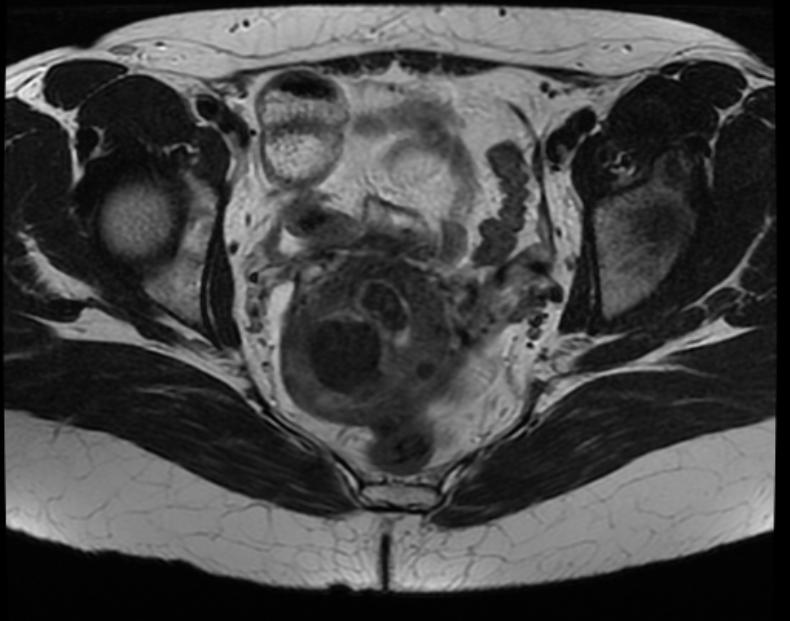
Patient #2: MR images demonstrate a leiomyoma prolapsing into the endometrial canal
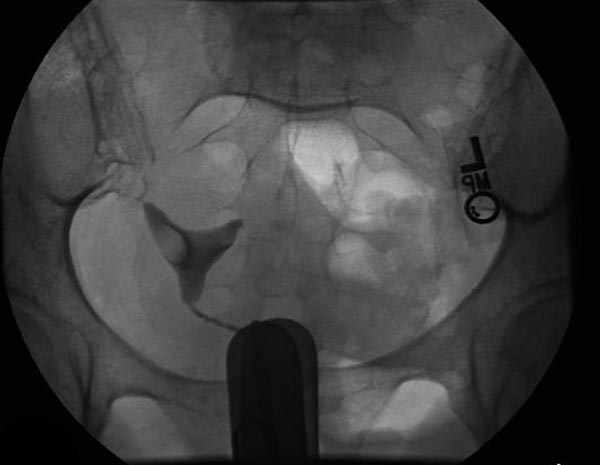
Hysterosalpingogram(HSG) reveals a submucosal leiomyoma
Treatment
Medical Therapy
- The mainstay of therapy for uterine leiomyoma is oral contraceptive pills, either combination pills or progestin-only, Gonadotropin-releasing hormone analogs.
Surgery
- Surgery is the mainstay of therapy for uterine leiomyoma.
- Uterine artery embolization in conjunction with laparotomic myomectomy is the most common approach to the treatment of [disease name].
- Hysteroscopic myomectomy can also be performed for patients with uterine leiomyoma.
References
- ↑ Bozini, Nilo; Baracat, Edmund C (2007). "The history of myomectomy at the Medical School of University of São Paulo". Clinics. 62 (3). doi:10.1590/S1807-59322007000300002. ISSN 1807-5932.
- ↑ Genetics of Uterine Leiomyomas. glowm (2016). http://www.glowm.com/section_view/heading/Genetics%20of%20Uterine%20Leiomyomas/item/363 Accessed on April 19, 2016
- ↑ James C. Chou, MD & Frank G. Gress, MD. "Benign Esophageal Tumors". Esophageal Cancer Overview (Cancer of the Esophagus). Retrieved 2007-03-21. Unknown parameter
|publsiher=ignored (|publisher=suggested) (help) - ↑ By Michael P. Buetow, M.D. "Leiomyoma of Jejunum". Retrieved 2007-03-21. Unknown parameter
|publsiher=ignored (|publisher=suggested) (help)