|
|
| Line 16: |
Line 16: |
| {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | | {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} |
|
| |
|
| ==Overview==
| | {{SK}} Juvenile osteochondrosis of head of femur; Perthes disease; Calve-Legg-Perthes disease; coxa plana; ischemic necrosis of the hip; osteochondritis; avascular necrosis of the femoral head; Legg-Perthes Disease; Legg-Calve-Perthes Disease; LCPD |
| '''Legg-Calvé-Perthes syndrome''' is a [[degenerative disease]] of the [[hip]] [[joint]], where a loss of bone mass leads to some degree of collapse of the hip joint, that is, to deformity of the ball of the femur and the surface of the hip socket. The disease is typically found in young children and small dogs, and it can lead to osteoarthritis in adults.
| |
| | |
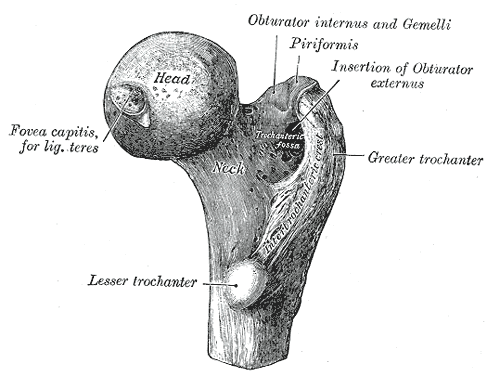
| It is the [[idiopathic]] avascular [[osteonecrosis]] of the capital femoral [[epiphysis]] of the femoral head. It is caused by an interruption to the [[circulatory system|blood supply]] of the head of the [[femur]] close to the [[hip joint]]. It is equivalent to adult [[avascular necrosis]].
| |
| | |
| It is also known as '''Perthes disease''',<ref>G. Perthes. Über Arthritis deformans juvenilis. Deutsche Zeitschrift für Chirurgie, Leipzig, 1910, 107: 111-159.</ref> ischemic necrosis of the hip, coxa plana, osteochondritis and avascular necrosis of the femoral head, or Legg-Perthes Disease or Legg-Calve-Perthes Disease (LCPD).
| |
| | |
| ==Cause==
| |
| The direct cause is a reduction in [[blood flow]] to the joint, though what causes this is unknown. It is thought that the artery of the ligamentum teres femoris closes too early, not allowing time for the [[medial circumflex femoral artery]] to take over. Genetics does not appear to be a determining factor, though it may be involved. When the disease is genetic in origin, it typically runs along the male line. Some evidence suggests that parental [[Tobacco smoking|smoking]] may be a factor, though this is not yet proven, or more recently that a deficiency of some blood factors used to disperse blood clots may lead to blockages in the vessels supplying the joint, but that, too, has not been proven.
| |
| | |
| ==Signs and symptoms==
| |
| Symptoms are hip or groin pain, exacerbated by hip/leg movement. There is a reduced [[range of motion]] at the hip joint and a painful [[gait]]. There may be atrophy of thigh muscles from disuse and an inequality of leg length. In some cases, some activity can cause severe irritation or inflammation of the damaged area including standing, walking, running, kneeling, or stooping repeatedly for an extended period of time.
| |
| | |
| The first signs are complaints of soreness from the child, which are often dismissed as [[growing pains]], and limping or other guarding of the joint, particularly when tired. The pain is usually in the hip, though can also be felt in the knee (so-called '[[referred pain]]'). In some cases, pain is felt in the unaffected hip and leg. This is due to the child favoring the injured side and placing the majority of the weight on the "good" leg. It is predominantly a disease of boys (around 4 in 5 cases). Whereas Perthes is generally diagnosed between 5 and 12 years of age, it has been diagnosed in children as young as infants. Typically the disease is only seen in one hip, bilateral perthes is seen in about 8-10% of children diagnosed.
| |
| ==Diagnosis==
| |
| [[X-Ray]]s of the hip joint are absolutely necessary. A [[bone scan]] may be useful in helping determine the extent of the avascular changes. A hip aspiration may be performed if there is suspicion of a [[septic arthritis]].
| |
| | |
| Diagnosis is made predominantly by [[X-ray]] study, together with physical examination ([[MRI]]s have also been found useful for judging the extent of the deformity). Sufferers typically have limited range of motion in their hip, particularly when rotating the joint.
| |
| | |
| * Early signs
| |
| | |
| ** Small femoral epiphysis (96%)
| |
| ** Sclerosis of the femoral head with sequestration and collapse (82%)
| |
| | |
| * Late signs
| |
| | |
| ** Radiolucent crescent line representing a subchondral fracture
| |
| ** Femoral head fragmentation and femoral neck cysts from intramedullary hemorrhage or extension of physeal cartilage into metaphysis, loose bodies, and coxa plana.
| |
| ** Coxa magna or remodeling of the femoral head, which becomes wider and flatter and similar in appearance to a mushroom.
| |
| | |
| <gallery>
| |
| Image:
| |
| | |
| Legg-calves-perthes-001.jpg
| |
| | |
| Image:
| |
| Legg-calves-perthes-002.jpg</gallery>
| |
| | |
| ==Treatment==
| |
| The goal of treatment is to avoid severe degenerative arthritis. Orthopedic assessment is crucial. Younger children have a better prognosis than older children. There are no drugs for treatment of Perthes. [[Analgesia|Analgesic medication]] may be given as necessary.
| |
| | |
| Treatment has traditionally centered on removing pressure from the joint until the disease has run its course. Options have included bed rest and traction (to separate the femur from the pelvis and reduce wear), often for several months or even years. Braces and plaster casts were also popular, again to isolate the joint. Recent evidence suggests that these methods are not effective, and treatment seems to be moving towards a mixture of careful monitoring, [[physiotherapy]], and surgical intervention when necessary. For older children, the distraction method been found to be a successful treatment by using an external fixator which relieves the hip from carrying the body's weight. This allows room for the top of the femur to regrow and shape better.
| |
| | |
| Modern treatment focuses on removing pressure from the joint in concert with physiotherapy. Pressure is minimized on the hip through use of [[Crutch|crutches]] or a cane, and the avoidance of running-based sports. [[Swimming]] is highly recommended - it allows exercise of the hip muscles with the full range of motion, while reducing the stress to a minimum. Physiotherapy treatment generally involves a daily series of exercises, with weekly meetings with a physiotherapist to monitor progress. These exercises focus on improving and maintaining a full range of motion of the femur within the hip socket. Performing these exercises during the healing process is essential to ensure that the femur and hip socket have a perfectly smooth interface. This will minimize the long term effects of the disease.
| |
| | |
| Perthes is a long-term problem - treatment is aimed at minimizing damage while the disease runs its course, not at 'curing' the disease. As sufferers age problems in the knee and back can arise, as a result of the abnormal posture and stride adopted to protect the affected joint. The condition is also linked to arthritis of the hip and other joints, though this appears not to be an inevitable consequence. Hip replacements are relatively common as the already damaged hip suffers routine wear; this varies by individual, but generally is required any time after age 50.
| |
| | |
| ==Incidence==
| |
| Perthes is a relatively unusual condition, with only 1 in 1200 children being affected.
| |
| | |
| Caucasians are affected more frequently than other races, males are affected 4-5 times more often than females, suggesting a partial sex-linked genetic inheratance of the the syndrome. 1 in 100 male children of adults with Legg-Calvé-Perthes syndrome also exhibit the syndrome. It is most commonly seen in persons aged 3-12 years, with a median of 6 years of age. In the US, 1 in 1200 children younger than 15 years will have this disease while in the UK the incidence is higher, with Ireland having the highest percentage. It is also found in Latin Americans, Asians and Inuit Indians.
| |
| | |
| ==Prognosis==
| |
| Children younger than 6 or 7 have the best prognosis since they have time for the dead bone to revascularize and remodel. Children that have been diagnosed with Perthes' Disease after the age of 10 are at a very high risk of developing [[osteoarthritis]] and Coxa Magna.
| |
|
| |
|
| ==References== | | ==References== |
| {{reflist|2}} | | {{reflist|2}} |
| <div class="references-small"> <references/> </div> | | <div class="references-small"> <references/> </div> |
|
| |
| ==External links==
| |
| * [http://groups.yahoo.com/groups/leggperthessupportgroup Legg Perthes Support Group, Int'l. Contact founder at reidweaver@yahoo.com to join]
| |
| * [http://www.perthes.org.uk Perthes Association (UK)]
| |
| * Because of its relatively low profile, much of the available literature on the subject is written from a medical viewpoint. A useful first step for parents or others affected by the disease is the [http://www.nonf.org/perthesbrochure/perthes-brochure.htm Legg-Calvé-Perthes Disease page of the National Osteonecrosis Foundation]
| |
|
| |
| * [http://whatiswhat.com Bill Shannon], a dancer with Legg-Calve-Perthes Syndrome who incorporates his crutches into his routines, which frequently take place in public with the intent of challenging peoples' perceptions of disability.
| |
|
| |
| * Parents of children with Perthes disease can get a lot of useful information from other parents in online support groups: [http://health.groups.yahoo.com/group/intl_perthes_support/ International Perthes Support] and [http://health.groups.yahoo.com/group/Information-perthes/ Legg Calve Perthes Disease Information] are very active
| |
|
| |
| * {{WhoNamedIt|synd|908}}
| |
|
| |
|
| {{Diseases of the musculoskeletal system and connective tissue}} | | {{Diseases of the musculoskeletal system and connective tissue}} |