Lateral medullary syndrome: Difference between revisions
No edit summary |
|||
| Line 19: | Line 19: | ||
==Overview== | ==Overview== | ||
The lateral medullary syndrome is one of the most common clinical syndromes of brainstem caused by the decreased blood supply to the lateral medulla. It is also commonly known as Wallenberg's syndrome or posterior inferior cerebellar artery syndrome (PICA). The most common cause is thromboembolic occlusion of vertebral arteries. It was described in 1895. | The lateral medullary syndrome is one of the most common clinical syndromes of brainstem caused by the decreased blood supply to the lateral medulla. It is also commonly known as Wallenberg's syndrome or posterior inferior cerebellar artery syndrome (PICA). The most common cause is thromboembolic occlusion of vertebral arteries. It was described in 1895. The lateral medullary syndrome is basically a manifestation of the vaso-occlusive disease of intracranial vertebral arteries (ICVA) such as vertebral artery or posterior inferior cerebellar artery. The various pathophysiologic mechanisms involved can include; atherosclerosis, athero-embolic phenomenon (heart, aorta, or vertebral arteries), dissection and increased vascular tortuosity, vascular insufficiency, Virchow’s triad play an important role in understanding the pathogenesis of Wallenberg's syndrome. | ||
==Historical Perspective== | ==Historical Perspective== | ||
* Gaspard Vieusseux, in 1808, was the first person to describe Wallenberg's syndrome | * Gaspard Vieusseux, in 1808, was the first person to describe Wallenberg's syndrome | ||
*This syndrome was later on further elaborated by Adolf Wallenberg, in 1895. | *This syndrome was later on further elaborated by Adolf Wallenberg, in 1895. | ||
*Thomas William was the first person to document extensive anatomy and physiology of brain stem, the cerebellum, and the ventricles in the 17th century. He performed necropsies and extensive dissections on his patient's brains. | *Thomas William was the first person to document extensive anatomy and physiology of brain stem, the cerebellum, and the ventricles in the 17th century. He performed necropsies and extensive dissections on his patient's brains. | ||
* Joseph Jules Dejerine (1849–1917) and his wife Dejerine-Klumpke demonstrated extensive visual illustrations of the various brain stem and cerebellar lesions. | * Joseph Jules Dejerine (1849–1917) and his wife Dejerine-Klumpke demonstrated extensive visual illustrations of the various brain stem and cerebellar lesions. | ||
* Charles Foix (1882–1927) was the first person to write an extensive case series on posterior cerebral arteries occlusion related syndromes and lateral medullary syndrome. | * Charles Foix (1882–1927) was the first person to write an extensive case series on posterior cerebral arteries occlusion related syndromes and lateral medullary syndrome. | ||
*Vertebral Basal Insufficiency (VBI) was first introduced by clinicians at the Mayo Clinic, Bob Siekert and Clark Millikan in 1970s. | *Vertebral Basal Insufficiency (VBI) was first introduced by clinicians at the Mayo Clinic, Bob Siekert and Clark Millikan in 1970s. | ||
== Pathophysiology == | == Pathophysiology == | ||
The lateral medullary syndrome is basically a manifestation of the vaso-occlusive disease of intracranial vertebral arteries (ICVA) such as vertebral artery or posterior inferior cerebellar artery. The various pathophysiologic mechanisms involved can include; | The lateral medullary syndrome is basically a manifestation of the vaso-occlusive disease of intracranial vertebral arteries (ICVA) such as vertebral artery or posterior inferior cerebellar artery. The various pathophysiologic mechanisms involved can include; | ||
* Atherosclerosis, | * Atherosclerosis, | ||
| Line 54: | Line 54: | ||
== Causes == | == Causes == | ||
*[[Atherosclerosis]] (VA>PICA>Medullary arteries) | *[[Atherosclerosis]] (VA>PICA>Medullary arteries) | ||
*[[Embolism]] | *[[Embolism]] | ||
*[[Dissection]] (especially in younger patients) | *[[Dissection]] (especially in younger patients) | ||
*[[Dolichoectasias|Dolichoectasia]] | *[[Dolichoectasias|Dolichoectasia]] | ||
*[[Vasospasm]] | *[[Vasospasm]] | ||
| Line 92: | Line 92: | ||
*[[Ageusia]] or [[loss of taste]] on one side of the [[tongue]] | *[[Ageusia]] or [[loss of taste]] on one side of the [[tongue]] | ||
*[[Ataxia]] or [[incoordination]] | *[[Ataxia]] or [[incoordination]] | ||
*[[Diplopia]] or [[double vision]] | *[[Diplopia]] or [[double vision]] | ||
*Oscillopsia | *Oscillopsia | ||
*[[Dizziness]] | *[[Dizziness]] | ||
| Line 100: | Line 100: | ||
*Ipsilateral sensory deficits (pain and temperature sensation) affecting the face and cranial nerves | *Ipsilateral sensory deficits (pain and temperature sensation) affecting the face and cranial nerves | ||
**absence of pain on the ipsilateral side of the face, as well as an absent [[corneal reflex]] (Damage to the spinal [[trigeminal nucleus]]) | **absence of pain on the ipsilateral side of the face, as well as an absent [[corneal reflex]] (Damage to the spinal [[trigeminal nucleus]]) | ||
*[[Ataxia]] | *[[Ataxia]] | ||
*[[Horner's syndrome]] | *[[Horner's syndrome]] | ||
*Ipsilateral vocal fold paralysis | *Ipsilateral vocal fold paralysis | ||
*Palatal and pharyngeal paresis | *Palatal and pharyngeal paresis | ||
| Line 121: | Line 121: | ||
* Hemorrhagic stroke | * Hemorrhagic stroke | ||
* Multiple sclerosis | * Multiple sclerosis | ||
* Acute labyrinthitis | * Acute labyrinthitis | ||
* Acute neuromyelitis optic | * Acute neuromyelitis optic | ||
* Chronic pain syndrome | * Chronic pain syndrome | ||
| Line 135: | Line 135: | ||
==== Diagnostic Tests: ==== | ==== Diagnostic Tests: ==== | ||
* MRI is the best diagnostic test to establish the diagnosis of Wallenberg's syndrome resulting from an infarct. | * MRI is the best diagnostic test to establish the diagnosis of Wallenberg's syndrome resulting from an infarct. | ||
* CTA and MRA can also be done to determine the vascular occlusion sites and to rule out dissection. | * CTA and MRA can also be done to determine the vascular occlusion sites and to rule out dissection. | ||
* An EKG should be done to rule out any underlying thromboembolic phenomenon such as afib. | * An EKG should be done to rule out any underlying thromboembolic phenomenon such as afib. | ||
| Line 158: | Line 158: | ||
==Treatment== | ==Treatment== | ||
* An interprofessional approach, aiming at a rapid response and coordinated team effort, involving neurologist, neurology specialty nurse, and the pharmacist has shown improved outcomes. | * An interprofessional approach, aiming at a rapid response and coordinated team effort, involving neurologist, neurology specialty nurse, and the pharmacist has shown improved outcomes. | ||
*Treatment of Wallenberg's syndrome, like other stroke management, is aimed to achieve 3 goals | *Treatment of Wallenberg's syndrome, like other stroke management, is aimed to achieve 3 goals | ||
**Reducing the size of infarction | **Reducing the size of infarction | ||
| Line 165: | Line 165: | ||
* Management includes: | * Management includes: | ||
** IV Thrombolytics | ** IV Thrombolytics | ||
*** Tissue plasminogen activator (TPA) within 3-4.5 hours | *** Tissue plasminogen activator (TPA) within 3-4.5 hours | ||
** Endovascular revascularization | ** Endovascular revascularization | ||
*** For larger intracranial vessels | *** For larger intracranial vessels | ||
Revision as of 18:04, 3 August 2020
| Lateral medullary syndrome | |
 | |
|---|---|
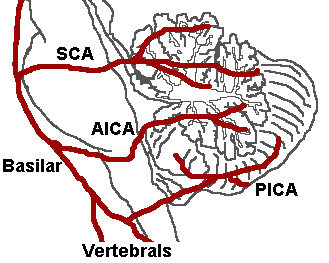
| The three major arteries of the cerebellum: the SCA, AICA, and PICA. (Posterior inferior cerebellar artery is PICA.) | |
| ICD-10 | G46.3 |
| DiseasesDB | 10449 |
| MeSH | D014854 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Wallenberg's syndrome; posterior inferior cerebellar artery syndrome (PICA)
Overview
The lateral medullary syndrome is one of the most common clinical syndromes of brainstem caused by the decreased blood supply to the lateral medulla. It is also commonly known as Wallenberg's syndrome or posterior inferior cerebellar artery syndrome (PICA). The most common cause is thromboembolic occlusion of vertebral arteries. It was described in 1895. The lateral medullary syndrome is basically a manifestation of the vaso-occlusive disease of intracranial vertebral arteries (ICVA) such as vertebral artery or posterior inferior cerebellar artery. The various pathophysiologic mechanisms involved can include; atherosclerosis, athero-embolic phenomenon (heart, aorta, or vertebral arteries), dissection and increased vascular tortuosity, vascular insufficiency, Virchow’s triad play an important role in understanding the pathogenesis of Wallenberg's syndrome.
Historical Perspective
- Gaspard Vieusseux, in 1808, was the first person to describe Wallenberg's syndrome
- This syndrome was later on further elaborated by Adolf Wallenberg, in 1895.
- Thomas William was the first person to document extensive anatomy and physiology of brain stem, the cerebellum, and the ventricles in the 17th century. He performed necropsies and extensive dissections on his patient's brains.
- Joseph Jules Dejerine (1849–1917) and his wife Dejerine-Klumpke demonstrated extensive visual illustrations of the various brain stem and cerebellar lesions.
- Charles Foix (1882–1927) was the first person to write an extensive case series on posterior cerebral arteries occlusion related syndromes and lateral medullary syndrome.
- Vertebral Basal Insufficiency (VBI) was first introduced by clinicians at the Mayo Clinic, Bob Siekert and Clark Millikan in 1970s.
Pathophysiology
The lateral medullary syndrome is basically a manifestation of the vaso-occlusive disease of intracranial vertebral arteries (ICVA) such as vertebral artery or posterior inferior cerebellar artery. The various pathophysiologic mechanisms involved can include;
- Atherosclerosis,
- Athero-embolic phenomenon (heart, aorta, or vertebral arteries)
- Dissection and increased vascular tortuosity
- Vascular insufficiency
- Virchow’s triad play an important role in understanding the pathogenesis of Wallenberg's syndrome
- An abnormality of the intima and vascular wall
- An abnormality of blood flow, and
- An abnormality of blood coagulability
Involvement of various structures in lateral medulla along with respective manifestation or clinical signs include;
- Nucleus ambiguous: dysphagia, dysphonia, and dysarthria, laryngeal, pharyngeal and palatal paralysis
- Trigeminal nucleus: ipsilateral facial and corneal anesthesia
- Spinothalamic tract: loss of pain and temperature sensation to the opposite side of the body
- Cerebellum: ataxia
- Hypothalamic fibers: sympathetic nervous system abnormal c/w Horners syndrome
- Deiters' nucleus and other vestibular nuclei: nystagmus and vertigo
- Central tegmental tract: palatal myoclonus
Causes
- Atherosclerosis (VA>PICA>Medullary arteries)
- Embolism
- Dissection (especially in younger patients)
- Dolichoectasia
- Vasospasm
Risk Factors
- Uncontrolled hypertension
- Smoking
- Diabetes
- Neck manipulation or injury
- Marfan syndrome
- Ehlers Danlos syndrome
- Fibromuscular dysplasia.
Natural History, Complications and Prognosis
- The natural history, complications, and prognosis of Lateral medullary syndrome depends upon the size and location of the infarct/hemorrhagic area of the medulla.
- Some people may experience a gradual improvement in their symptoms with complete resolution of the symptoms within the week to months while others may worsen or show no improvement despite the treatment.
- Overall, the prognosis is good and most of the patients are able to return back to a normal baseline. Ataxia is seen as the most common sequelae.
- The most common complications seen are;
- Aspiration pneumonia
- Deep vein thrombosis
- Pulmonary embolism
- Myocardial infarction
Diagnosis
History and Physical Examination
- Rostral lesions present as marked dysphagia and dysphonia (nucleus ambiguous)
- Caudal lesion present as vertigo, ataxia, nausea/vomiting, and Horner syndrome
Ipsilateral (same side of lesion):
- Ageusia or loss of taste on one side of the tongue
- Ataxia or incoordination
- Diplopia or double vision
- Oscillopsia
- Dizziness
- Dysphagia or difficulties with swallowing
- Dysphonia or hoarseness
- Dysarthria or slurred speech
- Ipsilateral sensory deficits (pain and temperature sensation) affecting the face and cranial nerves
- absence of pain on the ipsilateral side of the face, as well as an absent corneal reflex (Damage to the spinal trigeminal nucleus)
- Ataxia
- Horner's syndrome
- Ipsilateral vocal fold paralysis
- Palatal and pharyngeal paresis
- Palatal myoclonus
- Hiccups
- Hoarseness
- Nystagmus
- Vertigo
Contralateral (opposite side of lesion):
- Contralateral sensory deficits (pain and temperature sensation) affecting the trunk and extremities
- No or minimal hemiparesis
Evaluation:
Differential Diagnosis:
- Hemorrhagic stroke
- Multiple sclerosis
- Acute labyrinthitis
- Acute neuromyelitis optic
- Chronic pain syndrome
- Lacunar stroke
- Middle cerebral artery stroke
- Migraine headache
- Posterior reversible encephalopathy syndrome
- Subarachnoid hemorrhage
- Subdural hematoma
- Systemic lupus erythematosus
- Vertebrobasilar stroke
Diagnostic Tests:
- MRI is the best diagnostic test to establish the diagnosis of Wallenberg's syndrome resulting from an infarct.
- CTA and MRA can also be done to determine the vascular occlusion sites and to rule out dissection.
- An EKG should be done to rule out any underlying thromboembolic phenomenon such as afib.
Localization of the Lesion
| Dysfunction | Effects |
| lateral spinothalamic tract | contralateral deficits in pain and temperature sensation from body |
| spinal trigeminal nucleus | ipsilateral loss of pain and temperature sensation from face |
| nucleus ambiguus (which affects vagus X and glossopharyngeal nerves IX) | dysphagia, hoarseness, diminished gag reflex |
| vestibular system | vertigo, diplopia, nystagmus, vomiting |
| descending sympathetic fibers | ipsilateral Horner's syndrome |
| central tegmental tract | palatal myoclonus |
Treatment
- An interprofessional approach, aiming at a rapid response and coordinated team effort, involving neurologist, neurology specialty nurse, and the pharmacist has shown improved outcomes.
- Treatment of Wallenberg's syndrome, like other stroke management, is aimed to achieve 3 goals
- Reducing the size of infarction
- Preventing any medical complication
- Improving patient outcome and prognosis
- Management includes:
- IV Thrombolytics
- Tissue plasminogen activator (TPA) within 3-4.5 hours
- Endovascular revascularization
- For larger intracranial vessels
- Carotid endarterectomy
- For larger extracranial vessels
- Antithrombotics has a controversial role in the setting of an acute stroke but have shown improved outcomes when combined with aspirin
- Oral anticoagulants and antiplatelet agents should be considered upon discharge for secondary prevention of stroke
- High dose statins
- Close ICU monitoring for first 24 hrs after giving TPA
- Blood pressure monitoring, allow permissive hypertension and lower the BP only if,
- BP > 220/120 mmHg
- Patient receives IV TPA
- Normal saline is preferred for IV fluids and hypotonic fluids should be avoided to prevent cerebral edema
- Blood pressure monitoring, allow permissive hypertension and lower the BP only if,
- Speech therapy to assess the risk of aspiration. A feeding tube or PEG tube may be considered for patients with severe dysphagia.
- Low dose heparin or low molecular weight heparin (LWMH) for DVT prophylaxis
- Physical therapy and Occupational therapy
- IV Thrombolytics
References
External links
Template:Diseases of the nervous system Template:Lesions of the spinal cord and brainstem