Lateral medullary syndrome: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
|||
| Line 31: | Line 31: | ||
* Atherosclerosis, | * Atherosclerosis, | ||
* Athero-embolic phenomenon (heart, aorta, or vertebral arteries) | * Athero-embolic phenomenon (heart, aorta, or vertebral arteries) | ||
* Dissection and increased vascular tortuosity | * Dissection and increased vascular tortuosity | ||
*Vascular insufficiency | |||
*Virchow’s triad play an impoprtant role in understanding the pathogenesis of Wallenberg's syndrome | |||
**An abnormality of the intima and vascular wall | |||
**An abnormality of blood flow, and | |||
**An abnormality of blood coagulability | |||
Involvement of various structures in lateral medulla along with respective manifestation or clinical signs include; | Involvement of various structures in lateral medulla along with respective manifestation or clinical signs include; | ||
Revision as of 01:35, 3 August 2020
| Lateral medullary syndrome | |
 | |
|---|---|
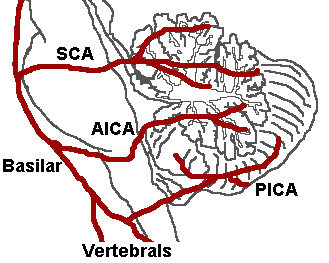
| The three major arteries of the cerebellum: the SCA, AICA, and PICA. (Posterior inferior cerebellar artery is PICA.) | |
| ICD-10 | G46.3 |
| DiseasesDB | 10449 |
| MeSH | D014854 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Wallenberg's syndrome; posterior inferior cerebellar artery syndrome (PICA)
Overview
Historical Perspective
- Thomas William was the first person to document extensive anatomy and physiology of brain stem, the cerebellum, and the ventricles in 17th century. He performed necropsies and extensive dissections on his patients brains.
- Joseph Jules Dejerine (1849–1917) and his wife Dejerine-Klumpke demonstrated extensive visual illustrations of various brain stem and cerebellar lesions.
- Charles Foix (1882–1927) was the firdt person to write an extensive case series on posterior cerebral arteries occlusion related syndromes and lateral medullary syndrome.
- Vertebral Basal Insufficiency (VBI) was first introduced by clinicians at the Mayo Clinic, Bob Siekert and Clark Millikan in 1970s.
Pathophysiology
Lateral medullary syndrome is basically a manifestation of vasoocclusive disease of intracranial vertebral artery (ICVA) such as vertebral artery or posterior inferior cerebellar artery. The various pathophysiologic mechanisms involved can include
- Atherosclerosis,
- Athero-embolic phenomenon (heart, aorta, or vertebral arteries)
- Dissection and increased vascular tortuosity
- Vascular insufficiency
- Virchow’s triad play an impoprtant role in understanding the pathogenesis of Wallenberg's syndrome
- An abnormality of the intima and vascular wall
- An abnormality of blood flow, and
- An abnormality of blood coagulability
Involvement of various structures in lateral medulla along with respective manifestation or clinical signs include;
- Nucleus ambiguus: dysphagia, dysphonia and dysarthria, laryngeal, pharyngeal and palatal paralysis
- Trigeminal nucleus: ipsilateral facial and corneal anesthesia
- Spinothalamic tract: loss of pain and temperature sensation to the opposite side of body
- Crebellum: ataxia
- Hypothalamic fibers: sympathetic nervous system abnormal c/w Horners syndrome
- Deiters' nucleus and other vestibular nuclei: nystagmus and vertigo
- Central tegmental tract: palatal myoclonus
Causes
- Atherosclerosis
- Embolism
- Dissection
- Dolichoectasia
- Vasospasm (spasme arterielle)
- Hypercoaguability
- Uncontrolled hypertension
Natural History, Complications and Prognosis
- The natural history, complications and prognosis of Lateral medullary syndrome depends upon the size and location of the infarct/hemorrhagic area of medulla.
- Some people may experience gradual improvement in their symptoms with complete resolution of the symptoms within week to months while other may worsen or show no improvement despite the treatment.
Diagnosis
Symptoms
Symptoms include:
- Ageusia or loss of taste on one side of the tongue
- Ataxia or incoordination
- Diplopia or double vision
- Oscillopsia
- Dizziness
- Dysphagia or difficulties with swallowing
- Dysphonia or hoarseness
- Dysarthria or slurred speech
- Facial pain
- Falling
- Palatal myoclonus
- Hiccups
- Hoarseness
- Bilateral leg weakness
- Hemiparesis
- Hypesthesia or lack of pain and temperature sensation on only one side of the face
- Nystagmus
- Nausea and vomiting
- Vertigo
Physical Examination
Neurologic
- Contralateral sensory deficits (pain and temperature sensation) affecting the trunk and extremities
- Ipsilateral sensory deficits (pain and temperature sensation) affecting the face and cranial nerves
- absence of pain on the ipsilateral side of the face, as well as an absent corneal reflex (Damage to the spinal trigeminal nucleus)
- Ataxia
- Nystagmus,
- Horner's syndrome
- Ipsilateral vocal fold paralysis
- Palatal and pharyngeal paresis
Localization of the Lesion
| Dysfunction | Effects |
| lateral spinothalamic tract | contralateral deficits in pain and temperature sensation from body |
| spinal trigeminal nucleus | ipsilateral loss of pain and temperature sensation from face |
| nucleus ambiguus (which affects vagus X and glossopharyngeal nerves IX) | dysphagia, hoarseness, diminished gag reflex |
| vestibular system | vertigo, diplopia, nystagmus, vomiting |
| descending sympathetic fibers | ipsilateral Horner's syndrome |
| central tegmental tract | palatal myoclonus |
Treatment
- Treatment of Lateral medullary syndrome is symptomatic.
- Feeding tube or PEG tube may be considered for patients with severe dysphagia
- Patients with speech difficulties may benefit from speech therapy
- Acute and chronic pain management
References
External links
Template:Diseases of the nervous system Template:Lesions of spinal cord and brainstem