Intraosseous ganglion: Difference between revisions
No edit summary |
|||
| (20 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{SI}} | {{SI}} | ||
{{CMG}}; | {{CMG}}; AE {{DMakkar}} | ||
==Overview== | ==Overview== | ||
| Line 39: | Line 39: | ||
*3.Goldman and Feldman propose a theory suggesting that the initial proliferation of connective tissue cells induces heightened synthesis of hyaluronic acid, causing cystic metamorphosis at the site of initial proliferation. | *3.Goldman and Feldman propose a theory suggesting that the initial proliferation of connective tissue cells induces heightened synthesis of hyaluronic acid, causing cystic metamorphosis at the site of initial proliferation. | ||
However, the precise etiology remains unidentified. | |||
==Pathology== | |||
These cysts, situated within bone near joints, can either be solitary or consist of multiple compartments. | |||
They are filled with a thick, mucoid, gelatinous substance and are encased by a fibrous lining. In contrast to subchondral cysts, they lack an epithelial or synovial lining. | |||
The majority of intraosseous ganglia are small, typically measuring up to 1-2 cm, with larger lesions exceeding 5 cm being infrequent occurrences. | |||
==Epidemiology== | |||
Intraosseous ganglion cysts typically manifest during middle age, with the highest occurrence observed in individuals within the fourth and fifth decades of life. Additionally, there appears to be a slightly higher prevalence among men. | |||
===Locations=== | |||
Common locations are: | |||
*1.Epiphyses and metaphyses of long bones (tibia, femur, humerus, ulna) | |||
*2.Carpal or tarsal bones | |||
*3.Flat bones (acetabulum, scapula) | |||
==Natural History of Disease== | |||
Patients may exhibit symptoms such as localized pain, swelling, and/or tenderness, or they may remain asymptomatic. | |||
==Complications== | |||
Complications associated with intraosseous ganglion cysts may include | |||
*1.Fractures, often resulting from repeated erosion. | |||
*2.Rupture of tendons, notably the flexor tendon of the finger, presents another significant complication. | |||
*3.Reoccurrence of the cyst is a potential issue following bone graft procedures. | |||
*4.Documented cases have also highlighted the occurrence of carpal tunnel syndrome and the rupture of the flexor tendon of the index finger as notable complications. | |||
=Diagnosis= | |||
The identification of intraosseous ganglia typically relies on a combination of clinical history, physical examination, and characteristic imaging features. Confirmation of diagnosis through histological examination is feasible upon excision. | |||
==X-ray== | |||
*A solitary well-defined lytic lesion located in the subchondral region, characterized by a sclerotic margin. | |||
==CT scan== | |||
On computed tomography (CT), intraosseous ganglia manifest as isolated lucency within bone, accompanied by a sclerotic margin, typically adjacent to joints. | |||
==MRI== | |||
MRI is the diagnostic investigation of choice | |||
*Intraosseous ganglia typically manifest as solitary lesions, which can be either unilocular or multilocular. They often exhibit homogeneity and are encased by a sclerotic rim. | |||
*Fluid-fluid levels within intraosseous ganglia are uncommon, while bone marrow edema adjacent to the ganglion cyst is frequently observed. | |||
**T1: isointense-to-high signal (compared to skeletal muscle) | |||
**T2/STIR: high signal | |||
**T1C+: rim enhancement more common than heterogeneous enhancement | |||
==Bone Scan== | |||
Bone scintigraphy reveals heightened uptake of radiotracer. | |||
==Treatment== | |||
The treatment consists of bone grafting and curettage for bigger lesions, while small and asymptomatic cysts can be left as such. It can be performed open or arthroscopic. | |||
Various bone graft sources have been used, following are the pros and cons of each: | |||
*1.iliac crest as a graft in curettage and bone grafting procedures may give rise to complications associated with the donor site, encompassing issues such as painful scarring, infection, hematoma formation, fractures, and gait disturbances. | |||
*2.With distal radius, especially with cyst in carpals, prolonged immobilization is often necessary, potentially resulting in diminished outcomes such as reduced grip strength, limited range of motion, and a delay in the benefits of early mobilization and return to work. | |||
*3.Synthetic calcium phosphate graft 50% cases had persistent pain and 50% had partial absorption of cement | |||
*4.Autologous fibrin clot graft performed in capitate | |||
== Differential Diagnosis== | |||
The differential diagnosis of the intraosseous ganglion include: | |||
*subchondral cyst: adjacent degenerative joint disease present otherwise indistinguishable on imaging | |||
*unicameral bone cyst | |||
*chondromyxoid fibroma | |||
*Brodie abscess | |||
*giant cell tumour of bone | |||
*chondroblastoma | |||
*chondrosarcoma | |||
(mnemonic CFCBUGS) | |||
==References== | ==References== | ||
Latest revision as of 21:57, 15 April 2024
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; AE Dheeraj Makkar, M.D.[2]
Overview
Historical Perspective
- In 1928 Carp and Stout wrote a complete discussion on the genesis of the "simple" ganglion.
- In 1931 King proposed an intriguing hypothesis suggesting that the development of a ganglion was not attributed to degenerative processes but rather to the primitive mucoid secretion of connective tissue cells.
- Fairbank and Lloyd (1934), Ghormlev and Duckerty (1943), and Watson Jones (1948) have documented the reports of erosion of the tibial head by cysts originating from the semilunar cartilages.
- In 1949, Geoffrey R. Fisk introduced a description of an intraosseous ganglion in the distal end tibia.
- In 1956, Hicks introduced the term "synovial bone cysts" to characterize radiolucencies bordered by sclerotic margins within bones.
- In 1966, Crabbe coined the term "intraosseous ganglion" to describe a similar phenomenon.
- Other interchangeable terms for these entities include ganglionic cystic defect of bone, subchondral bone cyst, and juxta-articular bone cyst.
Classification
There are two primary types of intraosseous ganglion cysts:
- one arises from the infiltration of an extraosseous ganglion into the underlying bone,
- the other type is idiopathic in nature.
Pathophysiology
Potential theories regarding the pathogenesis include:
- 1.According to Menges et al., repeated instances of trauma may precipitate the protrusion of the synovial membrane into the subchondral spongiosa .
- 2.The second theory implicates myxoid degeneration of collagen fibers within the intraosseous connective tissue, possibly occurring during reparative processes subsequent to focal ischemic events or minor aseptic bone necroses.
- 3.Goldman and Feldman propose a theory suggesting that the initial proliferation of connective tissue cells induces heightened synthesis of hyaluronic acid, causing cystic metamorphosis at the site of initial proliferation.
However, the precise etiology remains unidentified.
Pathology
These cysts, situated within bone near joints, can either be solitary or consist of multiple compartments. They are filled with a thick, mucoid, gelatinous substance and are encased by a fibrous lining. In contrast to subchondral cysts, they lack an epithelial or synovial lining. The majority of intraosseous ganglia are small, typically measuring up to 1-2 cm, with larger lesions exceeding 5 cm being infrequent occurrences.
Epidemiology
Intraosseous ganglion cysts typically manifest during middle age, with the highest occurrence observed in individuals within the fourth and fifth decades of life. Additionally, there appears to be a slightly higher prevalence among men.
Locations
Common locations are:
- 1.Epiphyses and metaphyses of long bones (tibia, femur, humerus, ulna)
- 2.Carpal or tarsal bones
- 3.Flat bones (acetabulum, scapula)
Natural History of Disease
Patients may exhibit symptoms such as localized pain, swelling, and/or tenderness, or they may remain asymptomatic.
Complications
Complications associated with intraosseous ganglion cysts may include
- 1.Fractures, often resulting from repeated erosion.
- 2.Rupture of tendons, notably the flexor tendon of the finger, presents another significant complication.
- 3.Reoccurrence of the cyst is a potential issue following bone graft procedures.
- 4.Documented cases have also highlighted the occurrence of carpal tunnel syndrome and the rupture of the flexor tendon of the index finger as notable complications.
Diagnosis
The identification of intraosseous ganglia typically relies on a combination of clinical history, physical examination, and characteristic imaging features. Confirmation of diagnosis through histological examination is feasible upon excision.
X-ray
- A solitary well-defined lytic lesion located in the subchondral region, characterized by a sclerotic margin.
CT scan
On computed tomography (CT), intraosseous ganglia manifest as isolated lucency within bone, accompanied by a sclerotic margin, typically adjacent to joints.
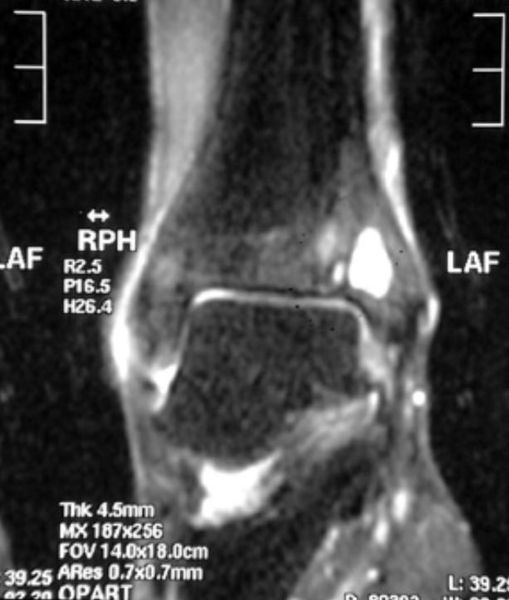
MRI
MRI is the diagnostic investigation of choice
- Intraosseous ganglia typically manifest as solitary lesions, which can be either unilocular or multilocular. They often exhibit homogeneity and are encased by a sclerotic rim.
- Fluid-fluid levels within intraosseous ganglia are uncommon, while bone marrow edema adjacent to the ganglion cyst is frequently observed.
- T1: isointense-to-high signal (compared to skeletal muscle)
- T2/STIR: high signal
- T1C+: rim enhancement more common than heterogeneous enhancement
Bone Scan
Bone scintigraphy reveals heightened uptake of radiotracer.
Treatment
The treatment consists of bone grafting and curettage for bigger lesions, while small and asymptomatic cysts can be left as such. It can be performed open or arthroscopic. Various bone graft sources have been used, following are the pros and cons of each:
- 1.iliac crest as a graft in curettage and bone grafting procedures may give rise to complications associated with the donor site, encompassing issues such as painful scarring, infection, hematoma formation, fractures, and gait disturbances.
- 2.With distal radius, especially with cyst in carpals, prolonged immobilization is often necessary, potentially resulting in diminished outcomes such as reduced grip strength, limited range of motion, and a delay in the benefits of early mobilization and return to work.
- 3.Synthetic calcium phosphate graft 50% cases had persistent pain and 50% had partial absorption of cement
- 4.Autologous fibrin clot graft performed in capitate
Differential Diagnosis
The differential diagnosis of the intraosseous ganglion include:
- subchondral cyst: adjacent degenerative joint disease present otherwise indistinguishable on imaging
- unicameral bone cyst
- chondromyxoid fibroma
- Brodie abscess
- giant cell tumour of bone
- chondroblastoma
- chondrosarcoma
(mnemonic CFCBUGS)