Intracranial hemorrhage CT: Difference between revisions
No edit summary |
|||
| (3 intermediate revisions by the same user not shown) | |||
| Line 17: | Line 17: | ||
*CT allows rapid establishment of the presence or absence of an ICH and exclusion of an [[Cerebrovascular accident | acute cerebral infarction]]. | *CT allows rapid establishment of the presence or absence of an ICH and exclusion of an [[Cerebrovascular accident | acute cerebral infarction]]. | ||
*Non-enhanced head CT is the preferred imaging modality for initial work-up as it provides crucial information regarding the characteristics of the ICH, including size, location, shape, and extension to the | *Non-enhanced head CT is the preferred imaging modality for initial work-up as it provides crucial information regarding the characteristics of the ICH, including size, location, shape, and extension to the extra-axial spaces. | ||
*If an ICH is present in a cortical-subcortical location suspicious for | *If an ICH is present in a cortical-subcortical location suspicious for cerebral amyloid angiopathy, the patient should undergo additional evaluation with MR imaging. | ||
*GRE is currently the most sensitive MR imaging sequence for detection of the chronic cortical-subcortical microhemorrhage. | *GRE is currently the most sensitive MR imaging sequence for detection of the chronic cortical-subcortical microhemorrhage. | ||
| Line 62: | Line 62: | ||
*Subarachnoid hemorrhage appears as a high-attenuating, amorphous substance that fills the normally dark CSF-filled subarachnoid spaces. | *Subarachnoid hemorrhage appears as a high-attenuating, amorphous substance that fills the normally dark CSF-filled subarachnoid spaces. | ||
*These findings are most evident in the largest subarachnoid spaces, such as the suprasellar cistern and Sylvian fissures. | *These findings are most evident in the largest subarachnoid spaces, such as the suprasellar cistern and Sylvian fissures. | ||
*Acute | *Acute subarachnoid hemorrhage is typically 50-60 HU. | ||
*When CT scanning is performed several days to weeks after the initial bleed, the findings are more subtle. | *When CT scanning is performed several days to weeks after the initial bleed, the findings are more subtle. | ||
**The initial high-attenuation of blood and clot tend to decrease, and these appear as intermediate gray. | **The initial high-attenuation of blood and clot tend to decrease, and these appear as intermediate gray. | ||
**These findings can be isointense relative to normal brain parenchyma. | **These findings can be isointense relative to normal brain parenchyma. | ||
*In addition to detecting | *In addition to detecting subarachnoid hemorrhage, CT is useful in localizing the source of bleeding. | ||
[http://www.radswiki.net Images courtesy of RadsWiki] | [http://www.radswiki.net Images courtesy of RadsWiki] | ||
| Line 84: | Line 84: | ||
**They do not cross the midline because of the meningeal reflections. | **They do not cross the midline because of the meningeal reflections. | ||
*In the | *In the acute phase, subdural hematomas appear as a crescent-shaped extra-axial collection with increased attenuation that, when large enough, causes effacement of the adjacent sulci and midline shift. | ||
*The attenuation changes as the hematoma ages. | *The attenuation changes as the hematoma ages. | ||
* | *Subacute subdural hematomas may be difficult to detect because they may have isoattenuation compared with adjacent gray matter | ||
* | *Chronic subdural hematomas have isoattenuation relative to the cerebrospinal fluid. | ||
*Rebleeding into subdural hematomas also may occur and is depicted as a layer of high-attenuation hemorrhage within a lower attenuation hematoma. | *Rebleeding into subdural hematomas also may occur and is depicted as a layer of high-attenuation hemorrhage within a lower attenuation hematoma. | ||
Latest revision as of 18:38, 13 March 2013
|
Intracranial hemorrhage Microchapters |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
CT
CT scan (computed axial tomography) is the definitive tool for accurate diagnosis of an intracranial hemorrhage.
 |
 |
Cerebral Amyloid Angiopathy [1]
- Cerebral amyloid angiopathy manifests radiologically as part or all of a constellation of findings including:
- Acute or chronic ICHs in a distinctive cortical-subcortical distribution
- Leukoencephalopathy
- Atrophy
- CT allows rapid establishment of the presence or absence of an ICH and exclusion of an acute cerebral infarction.
- Non-enhanced head CT is the preferred imaging modality for initial work-up as it provides crucial information regarding the characteristics of the ICH, including size, location, shape, and extension to the extra-axial spaces.
- If an ICH is present in a cortical-subcortical location suspicious for cerebral amyloid angiopathy, the patient should undergo additional evaluation with MR imaging.
- GRE is currently the most sensitive MR imaging sequence for detection of the chronic cortical-subcortical microhemorrhage.
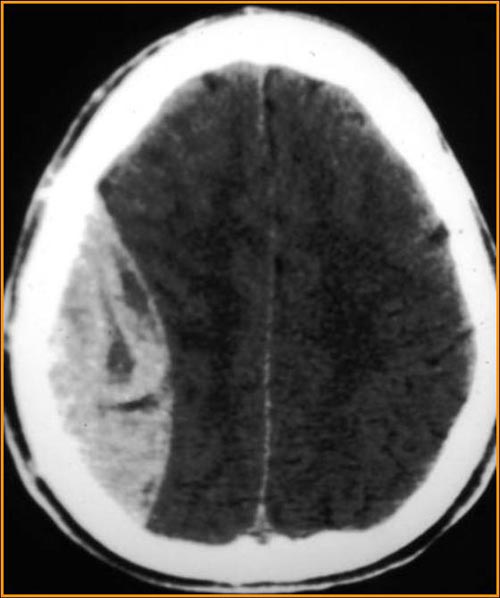
Epidural Hematoma
- Typical appearance is a biconvex, elliptical, extra-axial fluid collections.
- Acute EDH may contain both a hyperattenuating clot and a swirling lucency (believed to represent a mixture of active bleeding and the serum remaining after previous clot formation).
- Subacute EDH becomes homogeneously hyperattenuating.
- Chronic EDH is at least partly hypoattenuating as the clot undergoes breakdown and resorption.
-
CT: Epidural hematoma
-
CT: Epidural hematoma
-
CT: Epidural hematoma
-
CT: Epidural hematoma
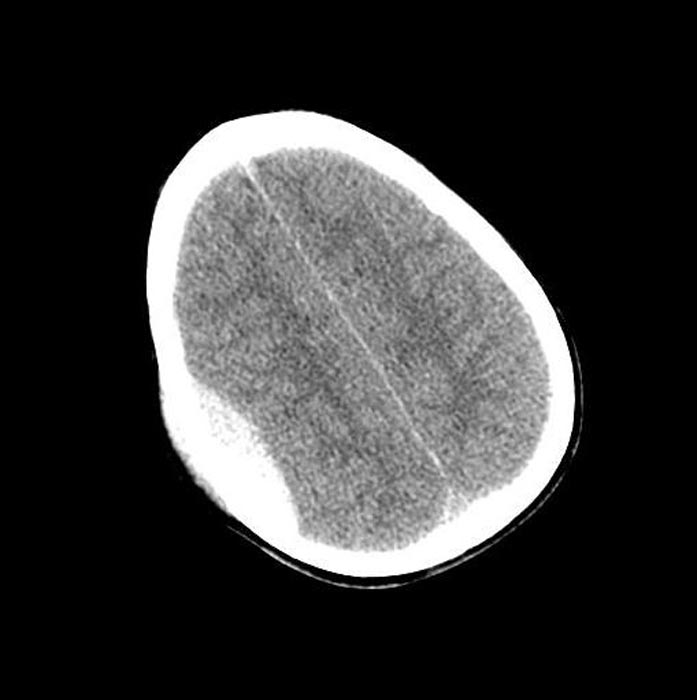
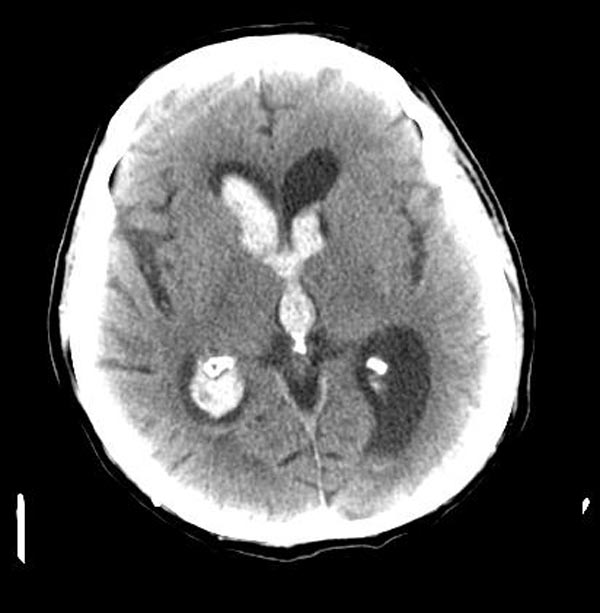
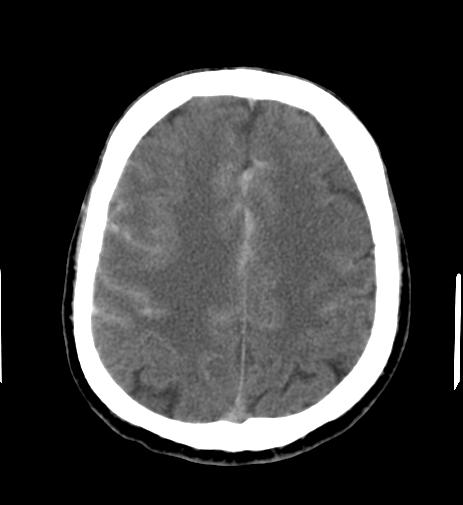
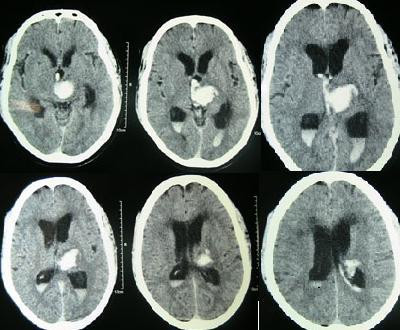
Intracerebral Parenchymal Hemorrhage
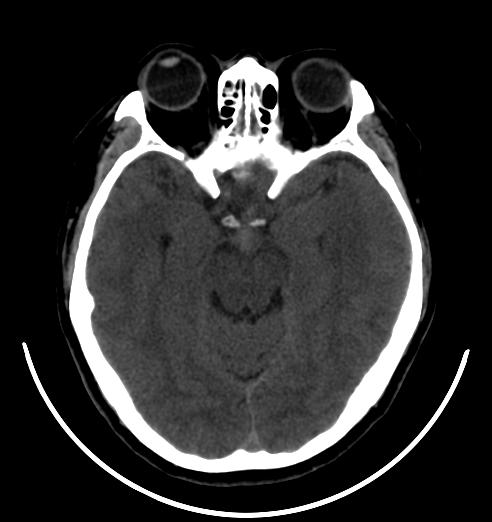
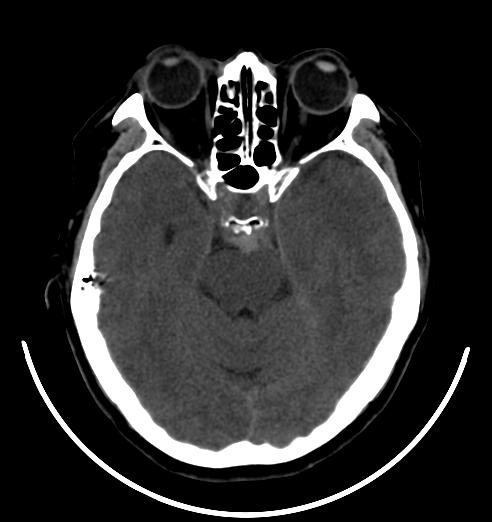
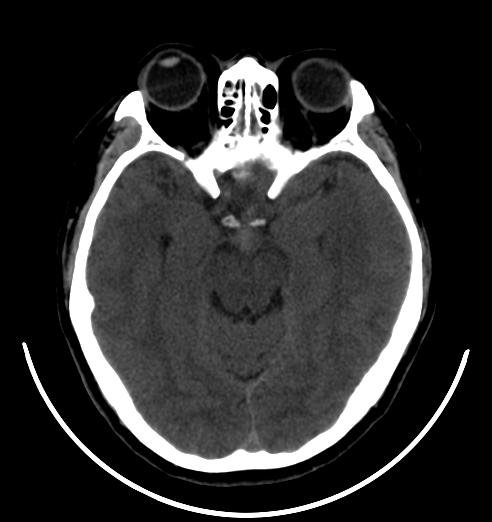
-
CT: Intracerebral parenchymal hemorrhage
-
CT: Intracerebral parenchymal hemorrhage
-
CT: Intracerebral parenchymal hemorrhage
-
CT: Intracerebral parenchymal hemorrhage
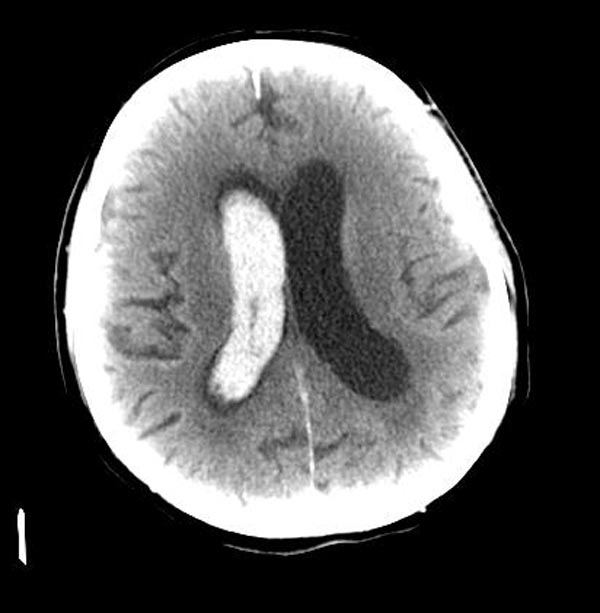
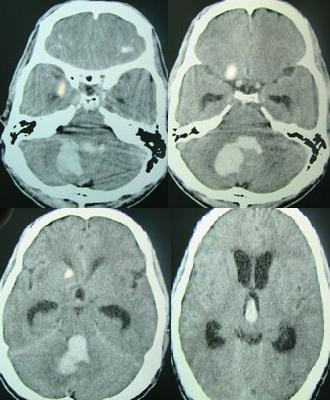
Intraventricular Hemorrhage
-
CT: Intraventricular hemorrhage
-
CT: Intraventricular hemorrhage
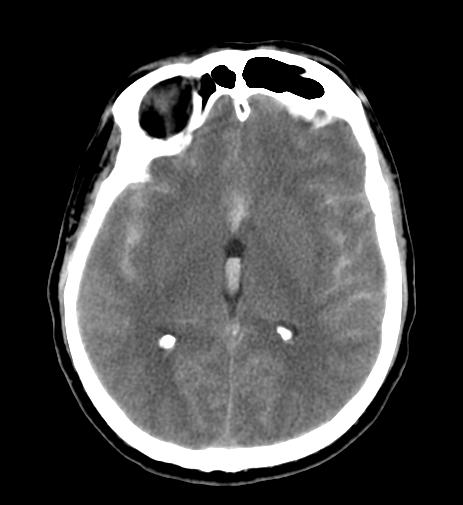
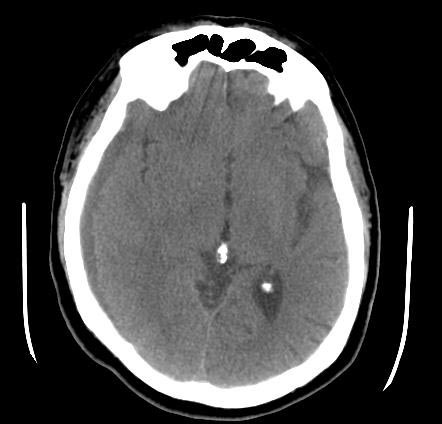
Subarachnoid Hemorrhage
Computed Tomography
- Subarachnoid hemorrhage appears as a high-attenuating, amorphous substance that fills the normally dark CSF-filled subarachnoid spaces.
- These findings are most evident in the largest subarachnoid spaces, such as the suprasellar cistern and Sylvian fissures.
- Acute subarachnoid hemorrhage is typically 50-60 HU.
- When CT scanning is performed several days to weeks after the initial bleed, the findings are more subtle.
- The initial high-attenuation of blood and clot tend to decrease, and these appear as intermediate gray.
- These findings can be isointense relative to normal brain parenchyma.
- In addition to detecting subarachnoid hemorrhage, CT is useful in localizing the source of bleeding.
-
CT: Diffuse subarachnoid hemorrhage
-
CT: Diffuse subarachnoid hemorrhage
-
CT: Diffuse subarachnoid hemorrhage
-
CT: Diffuse subarachnoid hemorrhage
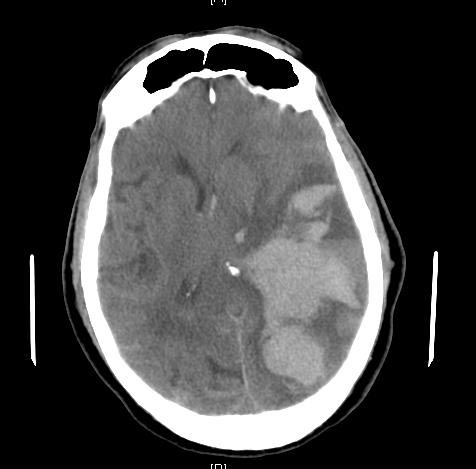
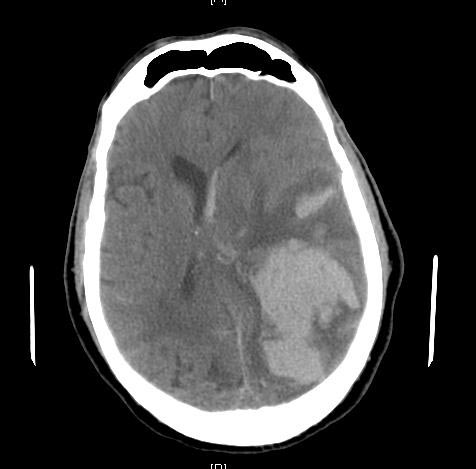
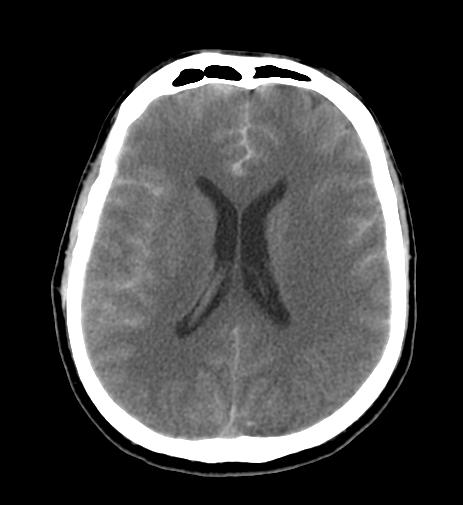
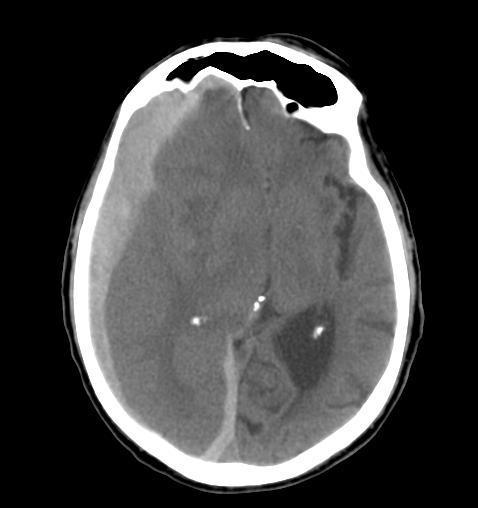
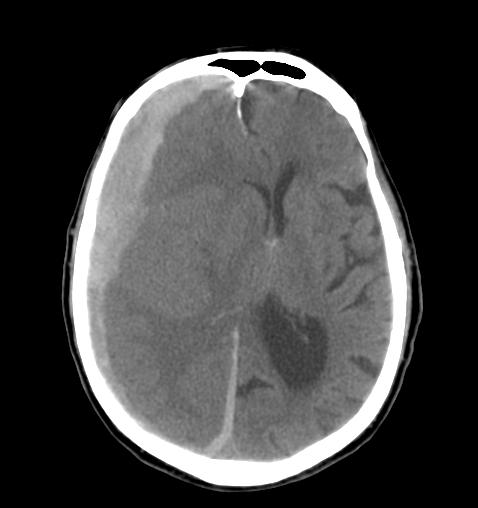
Subdural Hemorrhage
Computed Tomography
- Unlike epidural hematomas, subdural hematomas are not restricted by dural tethering at the cranial sutures.
- They can cross suture lines and continue along the falx and tentorium.
- They do not cross the midline because of the meningeal reflections.
- In the acute phase, subdural hematomas appear as a crescent-shaped extra-axial collection with increased attenuation that, when large enough, causes effacement of the adjacent sulci and midline shift.
- The attenuation changes as the hematoma ages.
- Subacute subdural hematomas may be difficult to detect because they may have isoattenuation compared with adjacent gray matter
- Chronic subdural hematomas have isoattenuation relative to the cerebrospinal fluid.
- Rebleeding into subdural hematomas also may occur and is depicted as a layer of high-attenuation hemorrhage within a lower attenuation hematoma.
-
CT: Subdural hemorrhage
-
CT: Subdural hemorrhage
-
CT: Subdural hemorrhage
-
CT: Subdural hemorrhage
-
CT: Subdural hemorrhage
Perimesencephalic Hemorrhage [2]
-
CT: Perimesencephalic hemorrhage
-
CT: Perimesencephalic hemorrhage
-
CT: Perimesencephalic hemorrhage
References
- ↑ Christine P. Chao, Amy L. Kotsenas, and Daniel F. Broderick. Cerebral Amyloid Angiopathy: CT and MR Imaging Findings. RadioGraphics 2006 26: 1517-1531.
- ↑ Schievink, Wouter I., Wijdicks, Eelco F.M., Spetzler, Robert F. Diffuse Vasospasm after Pretruncal Nonaneurysmal Subarachnoid Hemorrhage. AJNR Am J Neuroradiol 2000 21: 521-523