Indinavir: Difference between revisions
No edit summary |
No edit summary |
||
| Line 126: | Line 126: | ||
}} | }} | ||
|mechAction=[[HIV-1]] protease is an enzyme required for the proteolytic cleavage of the viral polyprotein precursors into the individual functional proteins found in infectious [[HIV-1]]. Indinavir binds to the protease active site and inhibits the activity of the enzyme. This inhibition prevents cleavage of the viral polyproteins resulting in the formation of immature non-infectious viral particles. | |mechAction=[[HIV-1]] protease is an enzyme required for the proteolytic cleavage of the viral polyprotein precursors into the individual functional proteins found in infectious [[HIV-1]]. Indinavir binds to the protease active site and inhibits the activity of the enzyme. This inhibition prevents cleavage of the viral polyproteins resulting in the formation of immature non-infectious viral particles. | ||
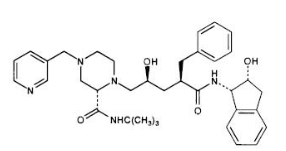
|structure=The chemical name for indinavir sulfate is | |structure=The chemical name for indinavir sulfate is 1(1S,2R),5(S)-2,3,5-trideoxy-N-(2,3-dihydro-2-hydroxy-1H-inden-1-yl)-5-2-(1,1-dimethylethyl)amino carbonyl-4-(3-pyridinylmethyl)-1-piperazinyl-2-(phenylmethyl)-D-erythro-pentonamide sulfate (1:1) salt. Indinavir sulfate has the following structural formula: | ||
[[file:Indinavir Structure.png|none|300px]] | [[file:Indinavir Structure.png|none|300px]] | ||
Revision as of 15:54, 2 February 2015
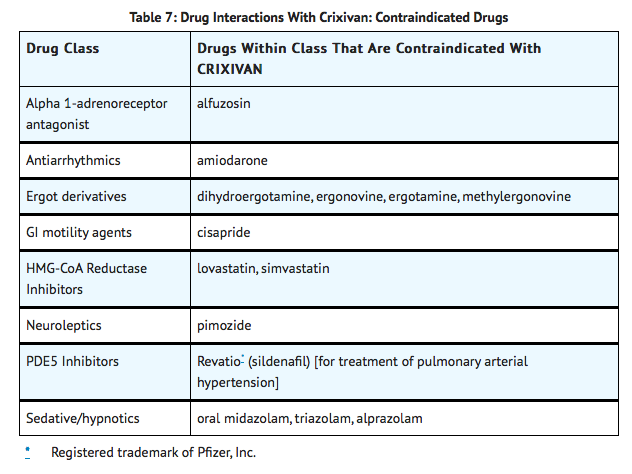
{{DrugProjectFormSinglePage |authorTag=Alberto Plate [1] |genericName=Indinavir |aOrAn=an |drugClass=antiretroviral agent and protease inhibitor |indicationType=treatment |indication=HIV infection in combination with other antiretroviral agents |adverseReactions=abdominal pain, heartburn, loss of appetite, nausea, taste sense altered, vomiting, neutrophil count abnormal, hyperbilirubinemia and headache |blackBoxWarningTitle=TITLE |blackBoxWarningBody=Condition Name: (Content) |offLabelAdultGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Indinavir in adult patients. |offLabelAdultNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Indinavir in adult patients. |offLabelPedGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Indinavir in pediatric patients. |offLabelPedNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Indinavir in pediatric patients. |contraindications=CRIXIVAN is contraindicated in patients with clinically significant hypersensitivity to any of its components.
Inhibition of CYP3A4 by CRIXIVAN can result in elevated plasma concentrations of the following drugs, potentially causing serious or life-threatening reactions:
|warnings=ALERT: Find out about medicines that should NOT be taken with CRIXIVAN. This statement is included on the product's bottle label.
Nephrolithiasis/Urolithiasis
Nephrolithiasis/urolithiasis has occurred with CRIXIVAN therapy. The cumulative frequency of nephrolithiasis is substantially higher in pediatric patients (29%) than in adult patients (12.4%; range across individual trials: 4.7% to 34.4%). The cumulative frequency of nephrolithiasis events increases with increasing exposure to CRIXIVAN; however, the risk over time remains relatively constant. In some cases, nephrolithiasis/urolithiasis has been associated with renal insufficiency or acute renal failure, pyelonephritis with or without bacteremia. If signs or symptoms of nephrolithiasis/urolithiasis occur, (including flank pain, with or without hematuria or microscopic hematuria), temporary interruption (e.g., 1-3 days) or discontinuation of therapy may be considered. Adequate hydration is recommended in all patients treated with CRIXIVAN.
Hemolytic Anemia
Acute hemolytic anemia, including cases resulting in death, has been reported in patients treated with CRIXIVAN. Once a diagnosis is apparent, appropriate measures for the treatment of hemolytic anemia should be instituted, including discontinuation of CRIXIVAN.
Hepatitis
Hepatitis including cases resulting in hepatic failure and death has been reported in patients treated with CRIXIVAN. Because the majority of these patients had confounding medical conditions and/or were receiving concomitant therapy(ies), a causal relationship between CRIXIVAN and these events has not been established.
Hyperglycemia
New onset diabetes mellitus, exacerbation of pre-existing diabetes mellitus and hyperglycemia have been reported during post-marketing surveillance in HIV-infected patients receiving protease inhibitor therapy. Some patients required either initiation or dose adjustments of insulin or oral hypoglycemic agents for treatment of these events. In some cases, diabetic ketoacidosis has occurred. In those patients who discontinued protease inhibitor therapy, hyperglycemia persisted in some cases. Because these events have been reported voluntarily during clinical practice, estimates of frequency cannot be made and a causal relationship between protease inhibitor therapy and these events has not been established.
Drug Interactions
Concomitant use of CRIXIVAN with lovastatin or simvastatin is contraindicated due to an increased risk of myopathy including rhabdomyolysis. Caution should be exercised if CRIXIVAN is used concurrently with atorvastatin or rosuvastatin. Titrate the atorvastatin and rosuvastatin doses carefully and use the lowest necessary dose with CRIXIVAN.
Midazolam is extensively metabolized by CYP3A4. Co-administration with CRIXIVAN with or without ritonavir may cause a large increase in the concentration of this benzodiazepine. No drug interaction study has been performed for the co-administration of CRIXIVAN with benzodiazepines. Based on data from other CYP3A4 inhibitors, plasma concentrations of midazolam are expected to be significantly higher when midazolam is given orally. Therefore CRIXIVAN should not be co-administered with orally administered midazolam, whereas caution should be used with co-administration of CRIXIVAN and parenteral midazolam. Data from concomitant use of parenteral midazolam with other protease inhibitors suggest a possible 3-4 fold increase in midazolam plasma levels. If CRIXIVAN with or without ritonavir is co-administered with parenteral midazolam, it should be done in a setting which ensures close clinical monitoring and appropriate medical management in case of respiratory depression and/or prolonged sedation. Dosage reduction for midazolam should be considered, especially if more than a single dose of midazolam is administered.
Particular caution should be used when prescribing sildenafil, tadalafil, or vardenafil in patients receiving indinavir. Coadministration of CRIXIVAN with these medications is expected to substantially increase plasma concentrations of sildenafil, tadalafil, and vardenafil and may result in an increase in adverse events, including hypotension, visual changes, and priapism, which have been associated with sildenafil, tadalafil, and vardenafil.
Concomitant use of CRIXIVAN and St. John's wort (Hypericum perforatum) or products containing St. John's wort is not recommended. Coadministration of CRIXIVAN and St. John's wort has been shown to substantially decrease indinavir concentrations and may lead to loss of virologic response and possible resistance to CRIXIVAN or to the class of protease inhibitors. |clinicalTrials=====Clinical Trials in Adults==== Nephrolithiasis/urolithiasis, including flank pain with or without hematuria (including microscopic hematuria), has been reported in approximately 12.4% (301/2429; range across individual trials: 4.7% to 34.4%) of patients receiving CRIXIVAN at the recommended dose in clinical trials with a median follow-up of 47 weeks (range: 1 day to 242 weeks; 2238 patient-years follow-up). The cumulative frequency of nephrolithiasis events increases with duration of exposure to CRIXIVAN; however, the risk over time remains relatively constant. Of the patients treated with CRIXIVAN who developed nephrolithiasis/urolithiasis in clinical trials during the double-blind phase, 2.8% (7/246) were reported to develop hydronephrosis and 4.5% (11/246) underwent stent placement. Following the acute episode, 4.9% (12/246) of patients discontinued therapy.
Asymptomatic hyperbilirubinemia (total bilirubin ≥2.5 mg/dL), reported predominantly as elevated indirect bilirubin, has occurred in approximately 14% of patients treated with CRIXIVAN. In <1% this was associated with elevations in ALT or AST.
Hyperbilirubinemia and nephrolithiasis/urolithiasis occurred more frequently at doses exceeding 2.4 g/day compared to doses ≤2.4 g/day.
Clinical adverse experiences reported in ≥2% of patients treated with CRIXIVAN alone, CRIXIVAN in combination with zidovudine or zidovudine plus lamivudine, zidovudine alone, or zidovudine plus lamivudine are presented in TABLE 10.
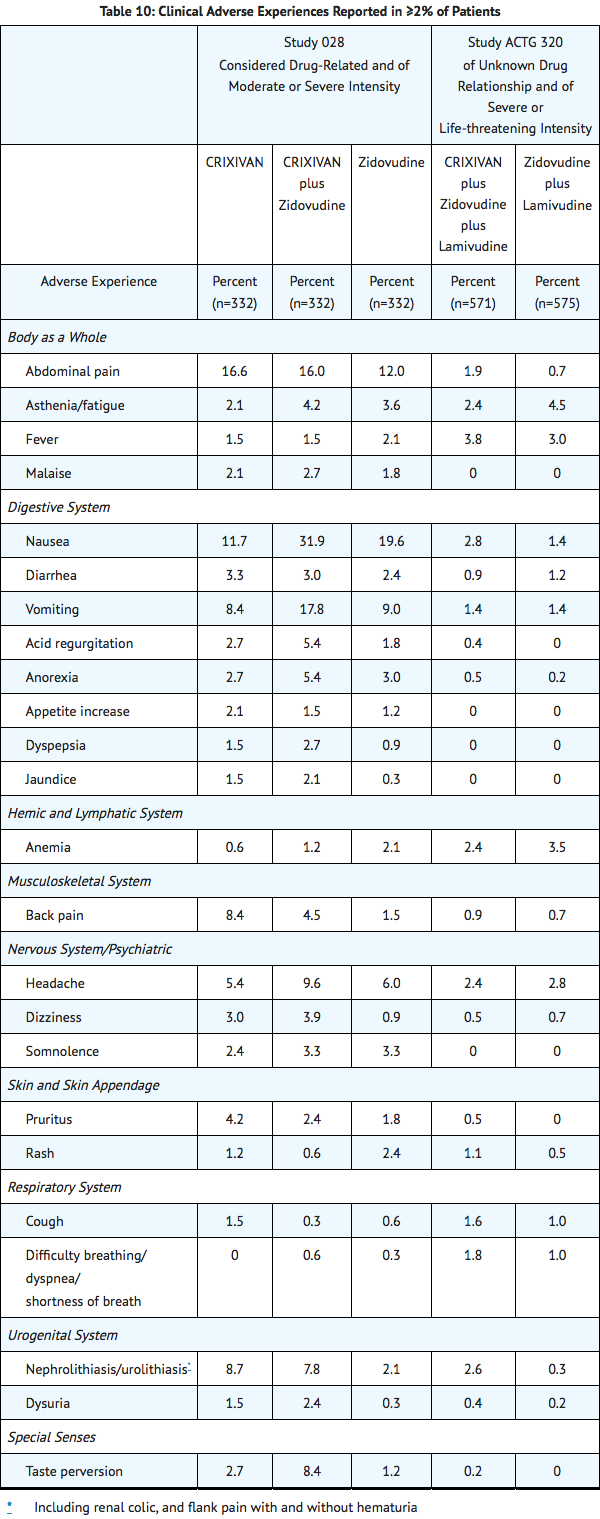
In Phase I and II controlled trials, the following adverse events were reported significantly more frequently by those randomized to the arms containing CRIXIVAN than by those randomized to nucleoside analogues: rash, upper respiratory infection, dry skin, pharyngitis, taste perversion.
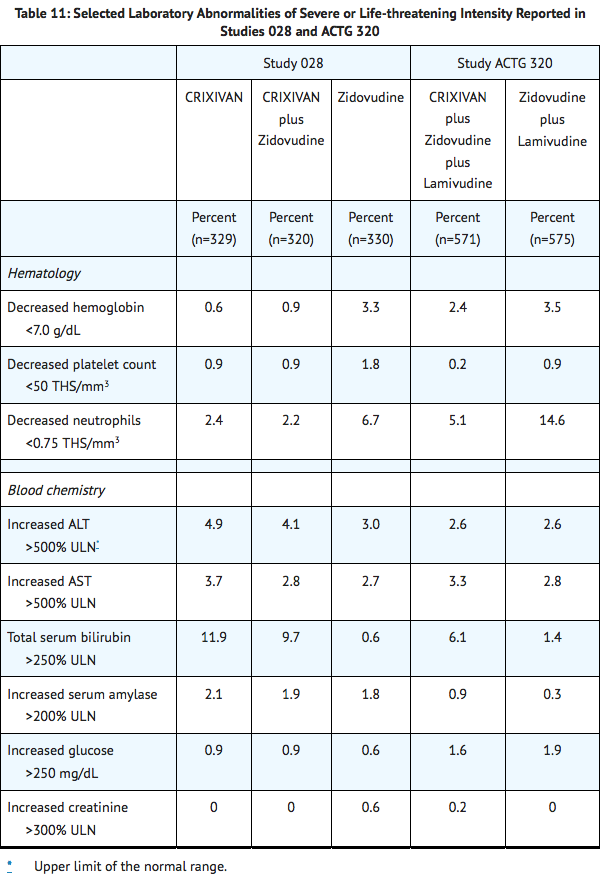
Selected laboratory abnormalities of severe or life-threatening intensity reported in patients treated with CRIXIVAN alone, CRIXIVAN in combination with zidovudine or zidovudine plus lamivudine, zidovudine alone, or zidovudine plus lamivudine are presented in Table 11.
|postmarketing=*Body As A Whole: redistribution/accumulation of body fat.
- Cardiovascular System: cardiovascular disorders including myocardial infarction and angina pectoris; cerebrovascular disorder.
- Digestive System: liver function abnormalities; hepatitis including reports of hepatic failure; pancreatitis; jaundice; abdominal distention; dyspepsia.
- Hematologic: increased spontaneous bleeding in patients with hemophilia; acute hemolytic anemia.
- Endocrine/Metabolic: new onset diabetes mellitus, exacerbation of pre-existing diabetes mellitus, hyperglycemia.
- Hypersensitivity: anaphylactoid reactions; urticaria; vasculitis.
- Musculoskeletal System: arthralgia, periarthritis.
- Nervous System/Psychiatric: oral paresthesia; depression.
- Skin and Skin Appendage: rash including erythema multiforme and Stevens-Johnson syndrome; hyperpigmentation; alopecia; ingrown toenails and/or paronychia; pruritus.
- Urogenital System: nephrolithiasis/urolithiasis, in some cases resulting in renal insufficiency or acute renal failure, [pyelonephritis]] with or without bacteremia; interstitial nephritis sometimes with indinavir crystal deposits; in some patients, the interstitial nephritis did not resolve following discontinuation of CRIXIVAN; renal insufficiency; renal failure; leukocyturia, crystalluria; dysuria.
- Laboratory Abnormalities: Increased serum triglycerides; increased serum cholesterol.
|overdose=There have been more than 60 reports of acute or chronic human overdosage (up to 23 times the recommended total daily dose of 2400 mg) with CRIXIVAN. The most commonly reported symptoms were renal (e.g., nephrolithiasis/urolithiasis, flank pain, hematuria) and gastrointestinal (e.g., nausea, vomiting, diarrhea). It is not known whether CRIXIVAN is dialyzable by peritoneal or hemodialysis. |drugBox={{Drugbox2 | Verifiedfields = changed | verifiedrevid = 477168143 | IUPAC_name = (2S)-1-[(2S,4R)-4-benzyl-2-hydroxy-4-{[(1S,2R)-2-hydroxy-2,3-dihydro-1H-inden-1-yl]carbamoyl}butyl]-N-tert-butyl-4-(pyridin-3-ylmethyl)piperazine-2-carboxamide | image = Indinavir Structure.png | width = 250 | image2 = Indinavir ball-and-stick.png
| tradename = Crixivan | Drugs.com = Monograph | MedlinePlus = a696028 | licence_US = Indinavir | pregnancy_US = C | legal_status = | routes_of_administration = Oral
| bioavailability = | protein_bound = 60% | metabolism = Hepatic via CYP3A4 | elimination_half-life = 1.8 (± 0.4) hours
| CASNo_Ref =
| CAS_number_Ref =
| CAS_number = 150378-17-9
| ATC_prefix = J05
| ATC_suffix = AE02
| ATC_supplemental =
| PubChem = 5362440
| DrugBank_Ref =
| DrugBank = DB00224
| ChemSpiderID_Ref =
| ChemSpiderID = 4515036
| NIAID_ChemDB = 005824
| UNII_Ref =
| UNII = 9MG78X43ZT
| KEGG_Ref =
| KEGG = C07051
| ChEBI_Ref =
| ChEBI = 44032
| ChEMBL_Ref =
| ChEMBL = 540914
| PDB_ligand = MK1
| C=36 | H=47 | N=5 | O=4
| molecular_weight = 613.79 g/mol
| smiles = CC(C)(C)NC(=O)[C@@H]1CN(CCN1C[C@H](C[C@@H](Cc2ccccc2)C(=O)N[C@H]3c4ccccc4C[C@H]3O)O)Cc5cccnc5
| InChI = 1/C36H47N5O4/c1-36(2,3)39-35(45)31-24-40(22-26-12-9-15-37-21-26)16-17-41(31)23-29(42)19-28(18-25-10-5-4-6-11-25)34(44)38-33-30-14-8-7-13-27(30)20-32(33)43/h4-15,21,28-29,31-33,42-43H,16-20,22-24H2,1-3H3,(H,38,44)(H,39,45)/t28-,29+,31+,32-,33+/m1/s1
| InChIKey = CBVCZFGXHXORBI-PXQQMZJSBP
| StdInChI_Ref =
| StdInChI = 1S/C36H47N5O4/c1-36(2,3)39-35(45)31-24-40(22-26-12-9-15-37-21-26)16-17-41(31)23-29(42)19-28(18-25-10-5-4-6-11-25)34(44)38-33-30-14-8-7-13-27(30)20-32(33)43/h4-15,21,28-29,31-33,42-43H,16-20,22-24H2,1-3H3,(H,38,44)(H,39,45)/t28-,29+,31+,32-,33+/m1/s1
| StdInChIKey_Ref =
| StdInChIKey = CBVCZFGXHXORBI-PXQQMZJSSA-N
}}
|mechAction=HIV-1 protease is an enzyme required for the proteolytic cleavage of the viral polyprotein precursors into the individual functional proteins found in infectious HIV-1. Indinavir binds to the protease active site and inhibits the activity of the enzyme. This inhibition prevents cleavage of the viral polyproteins resulting in the formation of immature non-infectious viral particles.
|structure=The chemical name for indinavir sulfate is 1(1S,2R),5(S)-2,3,5-trideoxy-N-(2,3-dihydro-2-hydroxy-1H-inden-1-yl)-5-2-(1,1-dimethylethyl)amino carbonyl-4-(3-pyridinylmethyl)-1-piperazinyl-2-(phenylmethyl)-D-erythro-pentonamide sulfate (1:1) salt. Indinavir sulfate has the following structural formula:
|alcohol=Alcohol-Indinavir interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. }}
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]; Associate Editor(s)-in-Chief: Mohamed Moubarak, M.D. [3]
Overview
Indinavir (IDV; trade name Crixivan, manufactured by Merck) is a protease inhibitor used as a component of highly active antiretroviral therapy (HAART) to treat HIV infection and AIDS.
Category
US Brand Names
CRIXIVAN®
FDA Package Insert
Description | Clinical Pharmacology | Microbiology | Indications and Usage | Contraindications | Warnings and Precautions | Adverse Reactions | Overdosage | Dosage and Administration | How Supplied
Mechanism of Action
HIV-1 protease is an enzyme required for the proteolytic cleavage of the viral polyprotein precursors into the individual functional proteins found in infectious HIV-1. Indinavir binds to the protease active site and inhibits the activity of the enzyme. This inhibition prevents cleavage of the viral polyproteins resulting in the formation of immature non-infectious viral particles.[1]
References
- ↑ "CRIXIVAN (INDINAVIR SULFATE) CAPSULE [MERCK SHARP & DOHME CORP.]". Text " accessdate" ignored (help)