|
|
| Line 20: |
Line 20: |
| {{SK}} Cryptogenic fibrosing alveolitis; IPF | | {{SK}} Cryptogenic fibrosing alveolitis; IPF |
|
| |
|
| ==Classification==
| |
| '''Idiopathic pulmonary fibrosis''' is a type of [[idiopathic interstitial pneumonia]] (IIP), which in turn is a type (or group) of interstitial lung diseases.<ref name=ATS2>{{cite journal |url=http://ajrccm.atsjournals.org/cgi/content/full/165/2/277 |title=American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias |journal=American Journal of Respiratory and Critical Care Medicine |volume=165 |number=2 |month=January |year=2002 |pages=277-304}}</ref>
| |
|
| |
|
| Idiopathic interstitial pneumonias include:
| |
| * [[idiopathic pulmonary fibrosis]] (IPF) (the most common)
| |
| * [[nonspecific interstitial pneumonia]]
| |
| * [[cryptogenic organizing pneumonia]]
| |
| * [[acute interstitial pneumonia]]
| |
| * respiratory bronchiolitis-associated interstitial lung disease
| |
| * [[desquamative interstitial pneumonia]]
| |
| * [[lymphoid interstitial pneumonia]]
| |
|
| |
|
| ==Clinical features== | | ==Clinical features== |
|
| |
|
| Idiopathic Pulmonary Fibrosis is slightly more common in males and usually presents in patients greater than 50 years of age. Average survival from time of diagnosis varies between 2.5 and 3.5 years, depending on severity, although some patients live greater than 10 years.<ref name=ATS2/>
| |
|
| |
|
| Symptoms are gradual in onset. The most common are [[dyspnea]] (difficulty breathing), but also include nonproductive [[cough]], [[clubbing]] (a disfigurement of the fingers), and [[crackles]] (crackling sound in lungs during inhalation).<ref name=ATS2/> It should be noted that these features are non-specific and can occur in a spectrum of other pulmonary disorders.
| |
|
| |
|
| The key issue facing clinicians is whether the presenting history, symptoms/signs, radiology, and pulmonary function testing are collectively in keeping with the diagnosis of IPF (which carries the relatively poor prognosis described above) or whether the findings are due to another process. It has long been recognized that patients with interstitial lung disease related to [[asbestos]] exposure, [[drug]]s (particularly [[chemotherapeutic]] agents), a [[connective tissue]] disease, or other diseases may have features that are difficult to distinguish from IPF. Important differential diagnostic considerations include asbestosis; interstitial lung disease related to [[scleroderma]], [[mixed connective tissue disease]], or [[rheumatoid arthritis]]; advanced sarcoidosis, [[hypersensitivity pneumonitis]], or [[Langerhans cell histiocytosis]]; chronic [[pulmonary aspiration]]; radiation-induced fibrosis; as well as previous therapy with [[cyclophosphamide]], [[nitrofurantoin]], [[methotrexate]], and other drugs.
| |
|
| |
|
| When diagnostic uncertainty remains, a surgical lung biopsy may be required to establish the diagnosis. Generally, lung biopsy is only undertaken when it is deemed that its risks are outweighed by the potential benefits of identifying a disease process that may be amenable to a treatment that the patient would likely be able to tolerate.
| |
|
| |
|
| The 2002 American Thoracic Society/European Respiratory Society Consensus Guidelines on the Idiopathic Interstitial Pneumonias have formalized criteria for situations in which it is possible to establish the diagnosis of IPF without a lung biopsy.<ref name=ATS2/>
| |
|
| |
|
| ==Radiology== | | ==Radiology== |
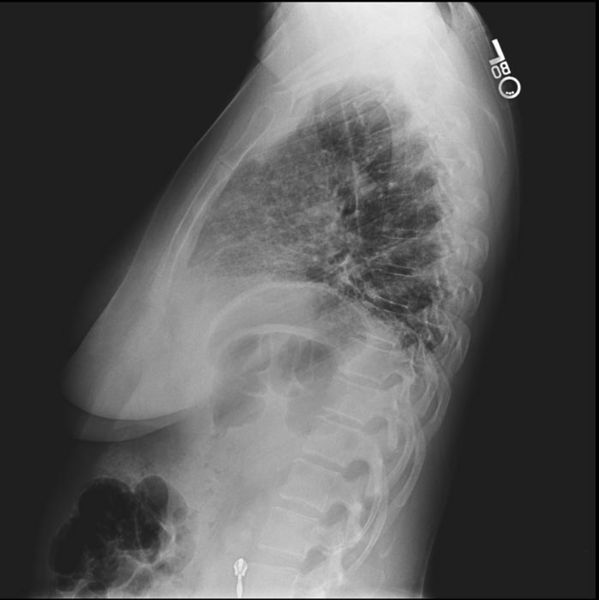
| Plain [[chest x-ray]]s reveal decreased lung volumes, typically with prominent reticular interstitial markings near the lung bases and posteriorly. Honeycombing, a pattern of dense fibrosis characterized by multiple tiny air-filled spaces located at the bases of the lungs, is frequently seen in advanced cases. In less severe cases, these changes may not be evident on a plain chest film.
| |
|
| |
|
| High-resolution CT scans of the chest demonstrate a symmetrical pattern of bibasilar, peripheral, and subpleural intralobular septal thickening, fibrotic changes, honeycombing, and traction bronchiectasis and bronchiolectasis. There may be associated ground glass opacity of the lungs but these changes are relatively minor in comparison with the fibrotic changes.<ref>{{cite book |last=Webb |first=W. Richard |coauthors=Nestor L. Müller and David P. Naidich |title=High-resolution CT of the lung |publisher=Lippincott Williams & Wilkins |location=Philadelphia |year=2001 |pages=196 |isbn=978-0781722780}}</ref>
| |
|
| |
|
| ==Pulmonary function tests==
| |
| [[Spirometry]] classically reveals a reduction in the vital capacity with either a proportionate reduction in airflows, or increased airflows for the observed vital capacity. The latter finding reflects the increased lung stiffness (reduced lung compliance) associated with pulmonary fibrosis, which leads to increased lung elastic recoil.<ref>{{cite journal |last=Pellegrino |first=R. |coauthors=Viegi G., Brusasco V., Crapo RO., et al. |title=Interpretative strategies for lung function tests |url=http://erj.ersjournals.com/cgi/content/full/26/5/948?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=1&andorexacttitle=and&andorexacttitleabs=and&andorexactfulltext=and&searchid=1&FIRSTINDEX=0&sortspec=relevance&volume=26&firstpage=948&resourcetype=HWCIT |journal=European Respiratory Journal |publiser=European Respiratory Society |year=2005 |month=November |volume=26 |number=5 |pages=948-68}}</ref>
| |
|
| |
|
| Measurement of static lung volumes using [[body plethysmography]] or other techniques typically reveals reduced lung volumes (restriction). This reflects the difficulty encountered in inflating the fibrotic lungs.
| |
|
| |
|
| The diffusing capacity for carbon monoxide (DLCO) is invariably reduced in IPF and may be the only abnormality in mild or early disease. Its impairment underlies the propensity of patients with IPF to exhibit oxygen desaturation with exercise.
| |
|
| |
| ==Histology==
| |
| {{main article|Usual interstitial pneumonia}}
| |
|
| |
|
| [[Image:Usual interstitial pneumonia (1).JPG|left|200px|thumb|[[Micrograph]] of usual interstitial pneumonia (UIP). UIP most often represents '''idiopathic pulmonary fibrosis'''. [[H&E stain]]. [[Autopsy]] specimen.]]
| |
|
| |
|
| [[Histology|Histologic]] specimens for the diagnosis of IPF must be large enough that the pathologist can comment on the underlying lung architecture.
| |
|
| |
| Small biopsies, such as those obtained via transbronchial lung biopsy (performed during [[bronchoscopy]]) are generally not sufficient for this purpose. Hence, larger biopsies obtained surgically via a thoracotomy or thoracoscopy are usually necessary.<ref name=ATS2/>
| |
|
| |
| The histological pattern of fibrosis associated with '''IPF''' is referred to as usual interstitial pneumonia (UIP).
| |
|
| |
| Although '''UIP''' is required for the diagnosis of '''IPF''', it can be seen in other diseases as well.<ref>{{cite book |title=Robbins and Cotran's Pathological Basis of Disease |edition=7th ed. |first=Vinay |last=Kumar |coauthors=Nelso Fausto and Abul Abbas |year=2005 |publisher=Saunders |isbn=978-0721601878 |pages=729}}</ref>
| |
|
| |
| Key features of UIP include fibroblast foci, a pattern of temporal heterogeneity, dense interstitial fibrosis in a paraseptal and subpleural distribution, and a relatively mild or minor component of interstitial chronic inflammation.<ref name=ATS2/> To help narrow the differential diagnosis, an absence of significant [[granuloma|granulomatous]] inflammation, [[microorganism]]s, [[eosinophil]]s, and [[asbestosis|asbestos bodies]] is required.
| |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| The diagnosis of IPF can be made by demonstrating UIP pattern on lung biopsy in a patient without clinical features suggesting an alternate diagnosis (see clinical features, above). Establishing the diagnosis of IPF without a lung biopsy has been shown to be reliable when expert clinicians and radiologists concur that the presenting features are typical of IPF.<ref>{{cite journal |last=Flaherty |first=Kevin R. |coauthors=Talmadge E. King, Jr., Ganesh Raghu, Joseph P. Lynch, III, Thomas V. Colby, William D. Travis, Barry H. Gross, Ella A. Kazerooni, Galen B. Toews, Qi Long, Susan Murray, Vibha N. Lama, Steven E. Gay, and Fernando J. Martinez |title=Idiopathic interstitial pneumonia: what is the effect of a multidisciplinary approach to diagnosis? |url=http://ajrccm.atsjournals.org/cgi/content/full/170/8/904 |journal=American Journal of Respiratory and Critical Care Medicine |year=2004 |volume=170 |pages=904-10}}</ref> Based on this evidence, the 2002 ATS/ERS Multidisciplinary Consensus Statement on the Idiopathic Interstitial Pneumonias proposes the following criteria for establishing the diagnosis of IPF without a lung biopsy:<ref name=ATS2/>
| |
|
| |
| Major criteria (all 4 required):
| |
| * Exclusion of other known causes of interstitial lung disease (drugs, exposures, connective tissue diseases)
| |
| * Abnormal [[pulmonary function test]]s with evidence of restriction (reduced [[vital capacity]]) and impaired gas exchange (pO<sub>2</sub>, p(A-a)O<sub>2</sub>, [[DLCO]])
| |
| * Bibasilar reticular abnormalities with minimal ground glass on high-resolution CT scans
| |
| * Transbronchial lung biopsy or bronchoalveolar lavage (BAL) showing no features to support an alternative diagnosis
| |
|
| |
|
| Minor criteria (3 of 4 required):
| |
| * Age > 50
| |
| * Insidious onset of otherwise unexplained exertional dyspnea
| |
| * Duration of illness > 3 months
| |
| * Bibasilar inspiratory crackles
| |
|
| |
|
| '''Radiographs and CT demonstrate usual intersitial pneumonia''' | | '''Radiographs and CT demonstrate usual intersitial pneumonia''' |
| Line 111: |
Line 65: |
| </gallery> | | </gallery> |
|
| |
|
| ==Treatment==
| |
| There is currently no consensus on the treatment of IPF. Hence, none of what follows should be taken as specific advice regarding therapy, as the latter is a decision that must be made on a case-by-case basis in individual patients.<ref name="Walter">{{cite journal | last=Walter | first=N | coauthors=Collard HR, Talmadge E. King, Jr. | title=Current perspectives on the treatment of idiopathic pulmonary fibrosis | journal=Proceedings of the American Thoracic Society | volume=3 | issue=4 | pages=330–338 | publisher=American Thoracic Society | month=June |year=2006 | url=http://pats.atsjournals.org/cgi/content/full/3/4/330 | pmid=16738197 | accessdate=2008-03-05 }}</ref>
| |
|
| |
|
| There is a lack of large, randomized placebo-controlled trials of therapy for IPF. Moreover, many of the earlier studies were based on the hypothesis that IPF is an inflammatory disorder, and hence studied anti-inflammatory agents such as [[corticosteroids]]. Another problem has been that studies conducted prior to the more recent classification of idiopathic interstitial pneumonias failed to distinguish IPF/UIP from NSIP in particular. Hence, many patients with arguably more steroid-responsive diseases were included in earlier studies, confounding the interpretation of their results.<ref name="Selman"/>
| |
|
| |
|
| Small early studies demonstrated that the combination of [[prednisone]] with either [[cyclophosphamide]] or [[azathioprine]] over many months had very modest, if any, beneficial effect in IPF, and were associated with substantial adverse effects (predominantly myelotoxicity). Other treatments studied have included [[interferon gamma]]-1b and the antifibrotic agent pirfenidone. While neither drug has been shown to have substantial benefits over time, both are currently being studied in patients with IPF. Finally, the addition of the [[antioxidant]] [[N-acetylcysteine]] to [[prednisone]] and [[azathioprine]] produced a slight benefit in terms of FVC and DLCO over 12 months of follow up. However, the major benefit appeared to be prevention of the myelotoxicity associated with [[azathioprine]].<ref>{{cite journal |last=Demedts |first=Maurits |coauthors=Juergen Behr; Roland Buhl; et al |title=High-dose acetylcysteine in idiopathic pulmonary fibrosis. The IFIGENIA Study |url=http://content.nejm.org/cgi/content/full/353/21/2229 |journal=New England Journal of Medicine |year=2005 |volume=353 |number=21 |pages=2229-2242}}</ref>
| |
|
| |
|
| ==References== | | ==References== |