Hydrocephalus
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Hydrocephalus |
|
Articles |
|---|
|
Most recent articles on Hydrocephalus Most cited articles on Hydrocephalus |
|
Media |
|
Powerpoint slides on Hydrocephalus |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Hydrocephalus at Clinical Trials.gov Trial results on Hydrocephalus Clinical Trials on Hydrocephalus at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Hydrocephalus NICE Guidance on Hydrocephalus
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Hydrocephalus Discussion groups on Hydrocephalus Patient Handouts on Hydrocephalus Directions to Hospitals Treating Hydrocephalus Risk calculators and risk factors for Hydrocephalus
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Hydrocephalus |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun M.D., PhD.
For patient information click here
Synonyms and keywords: Water on the brain
Overview
Hydrocephalus is a term derived from the Greek words "hydro" meaning water, and "cephalus" meaning head, and this condition is sometimes known as "water on the brain". People with this condition have abnormal accumulation of cerebrospinal fluid (CSF) in the ventricles, or cavities, of the brain. This may cause increased intracranial pressure inside the skull and progressive enlargement of the head, convulsion, and mental disability.
Historical Perspective
Hydrocephalus was first described by the ancient Greek physician Hippocrates, but it remained an intractable condition until the 20th century, when shunts and other neurosurgical treatment modalities were developed. The condition has been often informally referred to as "water on the brain".
Classification
Hydrocephalus can be caused by impaired cerebrospinal fluid (CSF) flow, reabsorption, or excessive CSF production.
- The most common cause of hydrocephalus is CSF flow obstruction, hindering the free passage of cerebrospinal fluid through the ventricular system and subarachnoid space (e.g., stenosis of the cerebral aqueduct or obstruction of the interventricular foramina - foramina of Monro secondary to tumors, hemorrhages, infections or congenital malformations).
- Hydrocephalus can also be caused by overproduction of cerebrospinal fluid (relative obstruction) (e.g., papilloma of choroid plexus).
Based on its underlying mechanisms, hydrocephalus can be classified into communicating, and non-communicating (obstructive). Both communicating and non-communicating forms can be either congenital, or acquired.
Communicating hydrocephalus
Communicating hydrocephalus, also known as non-obstructive hydrocephalus, is caused by impaired cerebrospinal fluid resorption in the absence of any CSF-flow obstruction. It has been theorized that this is due to functional impairment of the arachnoid granulations, which are located along the superior sagittal sinus and is the site of cerebrospinal fluid resorption back into the venous system. Various neurologic conditions may result in communicating hydrocephalus, including subarachnoid/intraventricular hemorrhage, meningitis, Chiari malformation, and congenital absence of arachnoidal granulations (Pacchioni's granulations).
- Normal pressure hydrocephalus (NPH) is a particular form of communicating hydrocephalus, characterized by enlarged cerebral ventricles, with only intermittently elevated cerebrospinal fluid pressure. The diagnosis of NPH can be established only with the help of continuous intraventricular pressure recordings (over 24 hours or even longer), since more often than not, instant measurements yield normal pressure values. Dynamic compliance studies may be also helpful. Altered compliance (elasticity) of the ventricular walls, as well as increased viscosity of the cerebrospinal fluid, may play a role in the pathogenesis of normal pressure hydrocephalus.
- Hydrocephalus ex vacuo also refers to an enlargement of cerebral ventricles and subarachnoid spaces, and is usually due to brain atrophy (as it occurs in dementias), post-traumatic brain injuries and even in some psychiatric disorders, such as schizophrenia. As opposed to hydrocephalus, this is a compensatory enlargement of the CSF-spaces in response to brain parenchyma loss - it is not the result of increased CSF pressure.
Non-communicating hydrocephalus
Non-communicating hydrocephalus, or obstructive hydrocephalus, is caused by a CSF-flow obstruction (either due to external compression or intraventricular mass lesions).
- Foramen of Monro obstruction may lead to dilation of one or, if large enough (e.g., in colloid cyst), both lateral ventricles.
- The aqueduct of Sylvius, normally narrow to begin with, may be obstructed by a number of genetically or acquired lesions (e.g., atresia, ependymitis, hemorrhage, tumor) and lead to dilatation of both lateral ventricles as well as the third ventricle.
- Fourth ventricle obstruction will lead to dilatation of the aqueduct as well as the lateral and third ventricles.
- The foramina of Luschka and foramen of Magendie may be obstructed due to congenital failure of opening (e.g., Dandy-Walker malformation).
- The subarachnoid space surrounding the brainstem may also be obstructed due to inflammatory or hemorrhagic fibrosing meningitis, leading to widespread dilatation, including the fourth ventricle.
Congenital hydrocephalus
The cranial bones fuse by the end of the third year of life. For head enlargement to occur, hydrocephalus must occur before then. The causes are usually genetic but can also be acquired and usually occur within the first few months of life, which include 1) intraventricular matrix hemorrhages in premature infants, 2) infections, 3) type II Arnold-Chiari malformation, 4) aqueduct atresia and stenosis, and 5) Dandy-Walker malformation.
In newborns and toddlers with hydrocephalus, the head circumference is enlarged rapidly and soon surpasses the 97th%. Since the skull bones have not yet firmly joined together, bulging, firm anterior and posterior fontanelles may be present even when the patient is in an upright position.
The infant exhibits fretfulness, poor feeding, and frequent vomiting. As the hydrocephalus progresses, torpor sets in, and the infant shows lack of interest in his surroundings. Later on, the upper eyelids become retracted and the eyes are turned downwards (due to hydrocephalic pressure on the mesencephalic tegmentum and paralysis of upward gaze). Movements become weak and the arms may become tremulous. Papilledema is absent but there may be reduction of vision. The head becomes so enlarged that the child may eventually be bedridden.
About 80-90% of fetuses or newborn infants with spina bifida - often associated with meningocele or myelomeningocele - develop hydrocephalus.
Acquired hydrocephalus
This condition is acquired as a consequence of CNS-infections, meningitis, brain tumors, head trauma, intracranial hemorrhage (subarachnoid or intraparenchymal) and is usually extremely painful for the patient.
Pathophysiology
Hydrocephalus is usually due to blockage of cerebral spinal fluid (CSF) outflow in the brain ventricles or in the subarachnoid space over the brain. In a normal healthy person, CSF continuously circulates through the brain and its ventricles and the spinal cord and is continuously drained away into the circulatory system. In a hydrocephalic situation, the fluid accumulates in the ventricles, and the skull may become enlarged because of the great volume of fluid pressing against the brain and skull. Alternatively, the condition may result from an overproduction of the CSF fluid, from a congenital malformation blocking normal drainage of the fluid, or from complications of head injuries or infections.[1]
Infants and young children with hydrocephalus typically have abnormally large heads, because the pressure of the fluid causes the individual skull bones — which have not knitted with each other yet — to bulge outward at their juncture points. Compression of the brain by the accumulating fluid eventually may cause convulsions and mental retardation. Hydrocephalus occurs in about one out of every 500 live births[2] and was routinely fatal until surgical techniques for shunting the excess fluid out of the central nervous system and into the blood or abdomen were developed.
The elevated intracranial pressure may cause compression of the brain, leading to brain damage and other complications. Conditions among affected individual vary widely. Children who have had hydrocephalus may have very small ventricles.
If the foramina (pl.) of the fourth ventricle or the cerebral aqueduct are blocked, cereobrospinal fluid (CSF) can accumulate within the ventricles. This condition is called internal hydrocephalus and it results in increased CSF pressure. The production of CSF continues, even when the passages that normally allow it to exit the brain are blocked. Consequently, fluid builds inside the brain causing pressure that compresses the nervous tissue and dilates the ventricles. Compression of the nervous tissue usually results in irreversible brain damage. If the skull bones are not completely ossified when the hydrocephalus occurs, the pressure may also severely enlarge the head. The cerebral aqueduct may be blocked at the time of birth or may become blocked later in life because of a tumor growing in the brainstem.
Usually, hydrocephalus need not cause any intellectual impairment if recognized and properly treated. A massive degree of hydrocephalus rarely exists in normally functioning people, and such rarity may occur if onset is gradual rather than sudden.[3]
Causes
Common Causes
- Brain hemorrhage associated with premature birth
Causes by Organ System
Causes In Alphabetical Order [4] [5]
|
Epidemiology and Demographics
Hydrocephalus affects one in every 500 live births, making it one of the most common birth defects, more common than Down syndrome or deafness.[2] There are an estimated 700,000 children and adults living with hydrocephalus, and it is the leading cause of brain surgery for children in the United States.
Natural History, Complications and Prognosis
One of the most performed treatments for hydrocephalus, the cerebral shunt, has not changed since it was developed in 1960. The shunt must be implanted through neurosurgery into the patient's brain, a procedure which itself may cause brain damage. An estimated 50% of all shunts fail within two years, requiring further surgery to replace the shunts. In the past 25 years, death rates associated with hydrocephalus have decreased from 54% to 5% and the occurrence of intellectual disability has decreased from 62% to 30%.
Because hydrocephalus injures the brain, thought and behavior may be adversely affected. Learning disabilities are common among those with hydrocephalus, who tend to score better on verbal IQ than on performance IQ, which is thought to reflect the distribution of nerve damage to the brain. However, the severity of hydrocephalus differs considerably between individuals and some are of average or above average intelligence. Someone with hydrocephalus may have motivation and visual problems, problems with coordination, and may be clumsy. They may hit puberty earlier than the average child (see precocious puberty). About one in four develops epilepsy.
Elevated intracranial pressure may result in uncal and/or cerebellar tonsill herniation, with resulting life threatening brain stem compression.
Diagnosis
Symptoms
The triad (Hakim triad) of gait instability, urinary incontinence and dementia is a relatively typical manifestation of the distinct entity normal pressure hydrocephalus (NPH). The triad can easily be remembered as "Wacky, Wet, and Wobbly!"
Symptoms of hydrocephalus due to increased intracranial pressure may include:
Physical Examination
HEENT
- Large head
- Papilledema
Neurologic
- Abducens nerve palsy and
- Vertical gaze palsy
- Parinaud syndrome due to compression of the quadrigeminal plate, where the neural centers coordinating the conjugated vertical eye movement are located
Imaging Findings
Because the problem resides inside the head, doctors rely heavily upon computer tomography scanning (CT scans), which may be used frequently to evaluate the condition of the disorder throughout the patient's life. Each CT scan exposes the patient to many times the level of x-ray radiation of a chest x-ray. See CT radiation exposure.
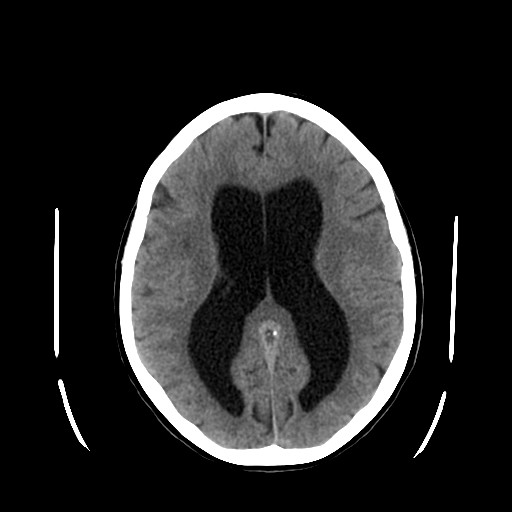
Hydrocephalus
-
Hydrocephalus
-
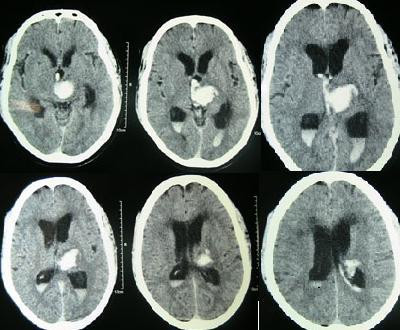
Intracerebral hemorrhage
-
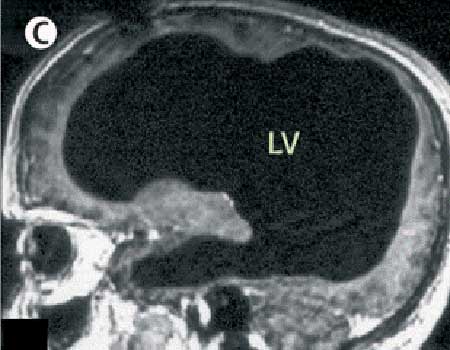
DWS: All of the black in the middle is cerebrospinal fluid and the brain matter is the rim of white along the outside of the skull.
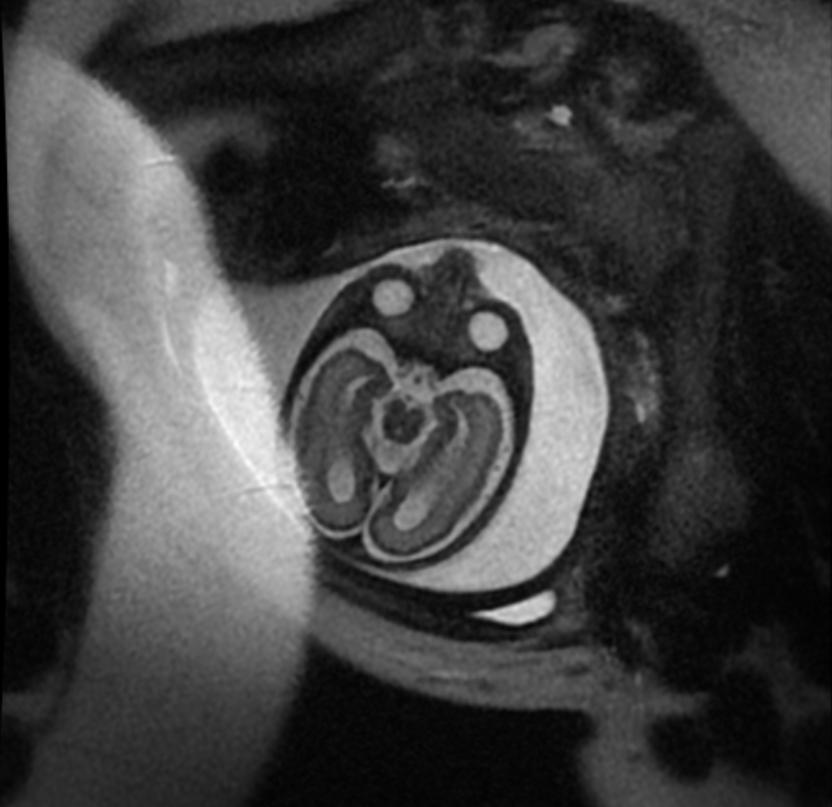
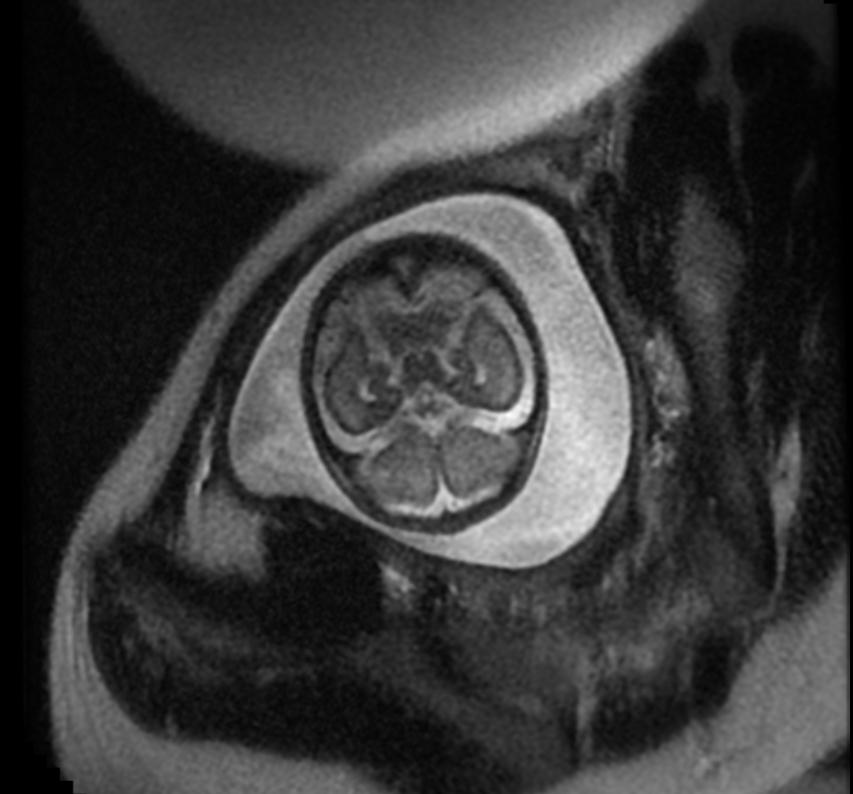
Aqueductal Stenosis
-
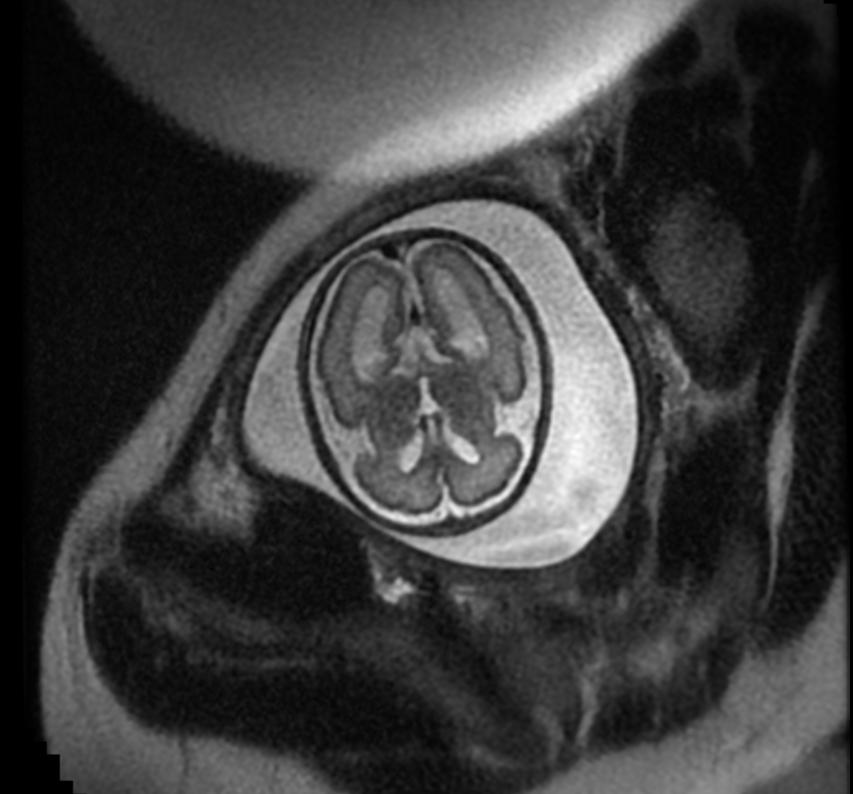
Fetal MRI: Aqueductal stenosis
-
Fetal MRI: Aqueductal stenosis
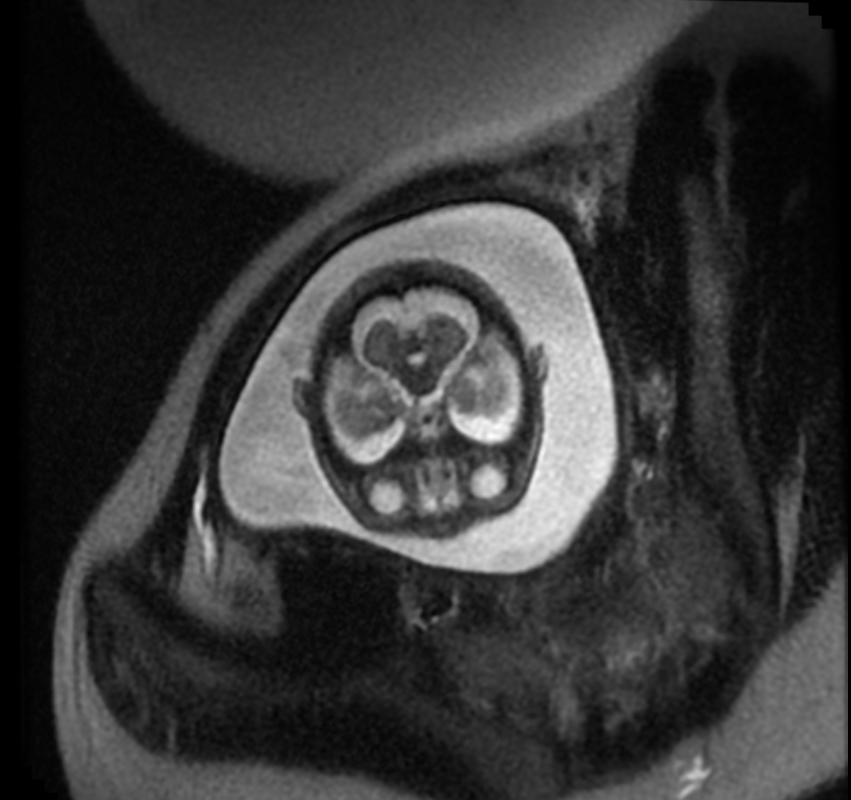
-
Fetal MRI: Aqueductal stenosis
-
Fetal MRI: Aqueductal stenosis
-
Fetal MRI: Aqueductal stenosis
Treatment
Hydrocephalus treatment is surgical. It involves the placement of a ventricular catheter (a tube made of silastic), into the cerebral ventricles to bypass the flow obstruction/malfunctioning arachnoidal granulations and drain the excess fluid into other body cavities, from where it can be resorbed. Most shunts drain the fluid into the peritoneal cavity (ventriculo-peritoneal shunt), but alternative sites include the right atrium (ventriculo-atrial shunt), pleural cavity (ventriculo-pleural shunt), and gallbladder. A shunt system can also be placed in the lumbar space of the spine and have the CSF redirected to the peritoneal cavity (LP Shunt). An alternative treatment for obstructive hydrocephalus in selected patients is the endoscopic third ventriculostomy (ETV), whereby a surgically created opening in the floor of the third ventricle allows the CSF to flow directly to the basal cisterns, thereby shortcutting any obstruction, as in aqueductal stenosis. This may or may not be appropriate based on individual anatomy. Internal hydrocephalus can be successfully treated by placing a drainage tube (shunt) between the brain ventricles and abdominal cavity to eliminate the high internal pressures. There is some risk of infection being introduced into the brain through these shunts, however, and the shunts must be replaced as the person grows. A subarachnoid hemorrhage may block the return of CSF to the circulation. If CSF accumulates in the subarachnoid space, the condition is called external hydrocephalus. In this condition, pressure is applied to the brain externally, compressing neural tissues and causing brain damage. Thus resulting to a much further damage of the brain tissue and leading to necrotization
Shunt complications
Examples of possible complications include shunt malfunction, shunt failure, and shunt infection. Although a shunt generally works well, it may stop working if it disconnects, becomes blocked, or it is outgrown. If this happens the cerebrospinal fluid will begin to accumulate again and a number of physical symptoms will develop, some extremely serious, like seizures. The shunt failure rate is also relatively high and it is not uncommon for patients to have multiple shunt revisions within their lifetime.
The diagnosis of cerebrospinal fluid buildup is complex and requires specialist expertise.
Another complication can occur when CSF drains more rapidly than it is produced by the choroid plexus, causing symptoms - listlessness, severe headaches, irritability, light sensitivity, sound sensitivity, nausea, vomiting, dizziness, vertigo, migraines, seizures, a change in personality, weakness in the arms or legs, excessive head growth (seen infants, children under age 2), strabismus, and double vision - to appear when the patient is vertical. If the patient lies down, the symptoms usually vanish in a short amount of time. A CT scan may or may not show any change in ventricle size, particularly if the patient has a history of slit-like ventricles. Difficulty in diagnosing overdrainage can make treatment of this complication particularly frustrating for patients and their families.
Resistance to traditional analgesic pharmacological therapy may also be sign of shunt overdrainage or failure. Diagnosis of the particular complication usually depends on when the symptoms appear.
Case Studies
One interesting case involving a person with past hydrocephalus was a 44-year old French man, whose brain had been reduced to little more than a thin sheet of actual brain tissue, due to the buildup of fluid in his skull. The man, who had a shunt inserted into his head to drain away fluid (which was removed when he was 14), went to a hospital after he had been experiencing mild weakness in his left leg.
In July of 2007, Fox News quoted Dr. Lionel Feuillet of Hopital de la Timone in Marseille as saying: "The images were most unusual... the brain was virtually absent."[6] When doctors learned of the man's medical history, they did a computed tomography (CT) scan and another type of scan called magnetic resonance imaging (MRI), and were astonished to see "massive enlargement" of the lateral ventricles in the skull. Intelligence tests showed the man had an IQ of 75, below the average score of 100 but not considered mentally retarded or disabled, either.
Remarkably, the man was a married father of two children, and worked as a civil servant, leading a normal life, despite having little brain tissue. "What I find amazing to this day is how the brain can deal with something which you think should not be compatible with life," commented Dr. Max Muenke, a pediatric brain defect specialist at the National Human Genome Research Institute. "If something happens very slowly over quite some time, maybe over decades, the different parts of the brain take up functions that would normally be done by the part that is pushed to the side."[7]
See also
- Spina bifida
- Acquired hydrocephalus (causes of it)
- Arachnoid granulation
- Brain
- Cerebrospinal fluid
- Intracranial pressure
- Normal pressure hydrocephalus
- Cerebral shunt
- Subarachnoid space
- Ventricular system
- HEC syndrome
References
- ↑ "Hydrocephalus Fact Sheet", National Institute of Neurological Disorders and Stroke. (August 2005).
- ↑ 2.0 2.1 Eat your way to a better brain for your baby December 2005. Virtual Learning Environment (VLE)
- ↑ "Man with tiny brain shocks doctors", New Scientist (2007-07-20).
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016
- ↑ Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X
- ↑ "Man with Almost No Brain Has Led Normal Life", Fox News (2007-07-25). Also see "Tiny brain, normal life; French doctors are puzzling over the case of 44-year-old civil servant who has led a quite normal life -- but with an extraordinarily tiny brain", Physorg.com (2007-07-20); "Tiny Brain, Normal Life", ScienceDaily (2007-07-24).
- ↑ Man Lives Normal Life Despite Having Abnormal Brain
External links
- International Federation for Spina Bifida and Hydrocephalus (IF), the umbrella organisation for national spina bifida and hydrocephalus organisations
- Hydrocephalus Association at hydroassoc.org, US
- Information on fetal hydrocephalus at fetalhydrocephalus.com
- Is the brain really necessary? at flatrock.org.nz
- Living with congenital hydrocephalus at Associated Content
Template:Diseases of the nervous system Template:Congenital malformations and deformations of nervous system
ca:Hidrocefàlia da:Hydrocephalus de:Hydrocephalus id:Hydrocephalus it:Idrocefalo nl:Hydrocefalus no:Hydrocephalus sr:Хидроцефалија fi:Vesipää sv:Vattenskalle