Hemorrhoids differential diagnosis
|
Hemorrhoids Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hemorrhoids differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Hemorrhoids differential diagnosis |
|
Risk calculators and risk factors for Hemorrhoids differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ahmed Younes M.B.B.CH [2]
Overview
Hemorrhoids should be differentiated from other diseases causing anal discomfort and pain with defecation such as rectal cancer, anal fissure, anal abscess, anal fistula.
Differentiating Hemorrhoids from other Diseases
Hemorrhoids should be differentiated from other diseases causing anal discomfort and pain with defecation.
| Disease | History | Physical exam findings | Sample image |
|---|---|---|---|
| Anal fissure |
|
|
 |
| Rectal prolapse |
|
|
 |
| Perianal abscess |
|
|
 |
| anal cancer |
|
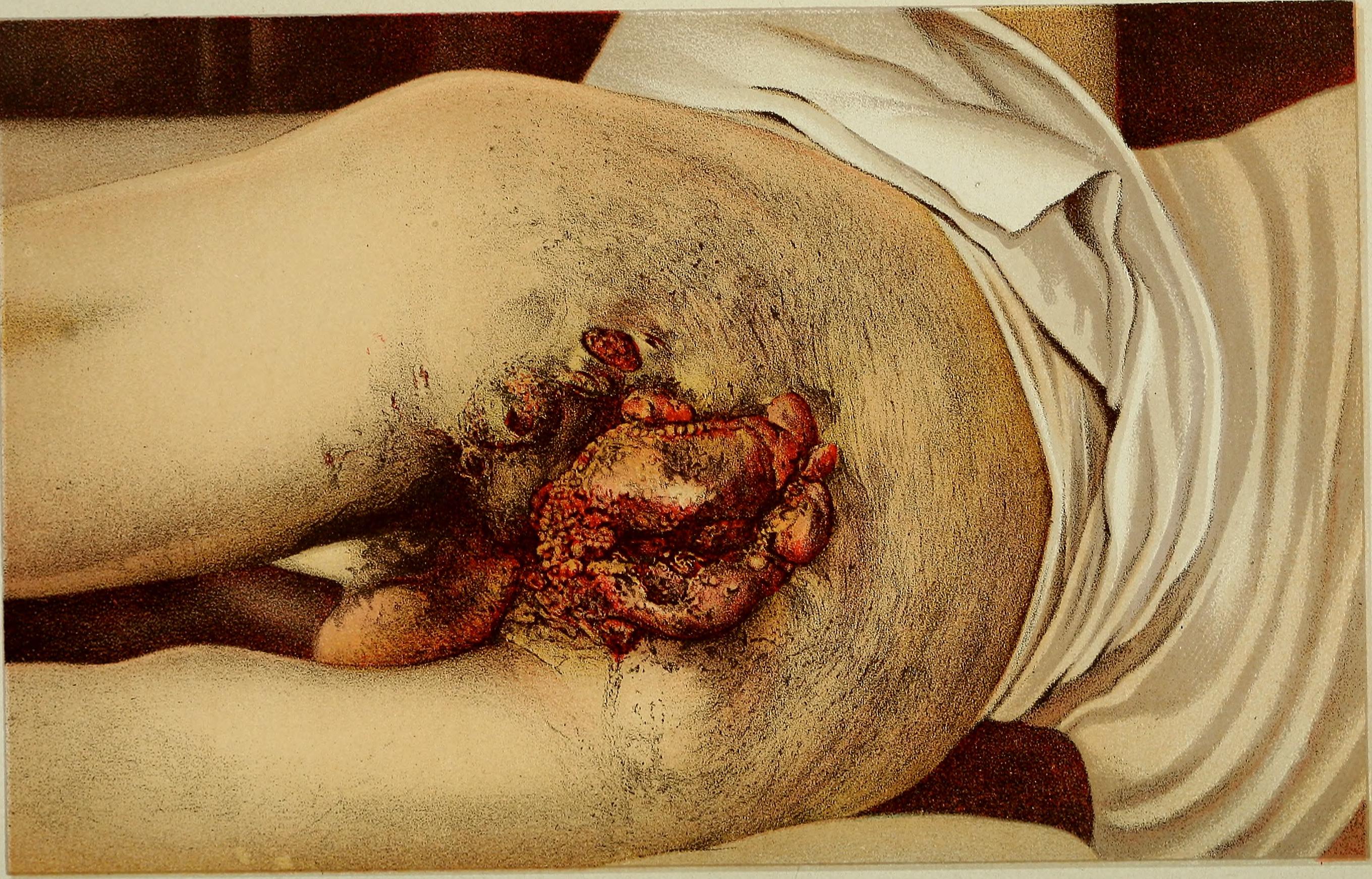 | |
| Condylomata acuminata |
|
|
 |
References
- ↑ Schlichtemeier S, Engel A (2016). "Anal fissure". Aust Prescr. 39 (1): 14–7. doi:10.18773/austprescr.2016.007. PMC 4816871. PMID 27041801.
- ↑ Beaty JS, Shashidharan M (2016). "Anal Fissure". Clin Colon Rectal Surg. 29 (1): 30–7. doi:10.1055/s-0035-1570390. PMC 4755763. PMID 26929749.
- ↑ Cannon JA (2017). "Evaluation, Diagnosis, and Medical Management of Rectal Prolapse". Clin Colon Rectal Surg. 30 (1): 16–21. doi:10.1055/s-0036-1593431. PMID 28144208.
- ↑ Blaker K, Anandam JL (2017). "Functional Disorders: Rectoanal Intussusception". Clin Colon Rectal Surg. 30 (1): 5–11. doi:10.1055/s-0036-1593433. PMID 28144206.
- ↑ Sahnan K, Adegbola SO, Tozer PJ, Watfah J, Phillips RK (2017). "Perianal abscess". BMJ. 356: j475. PMID 28223268.
- ↑ Moureau-Zabotto L, Vendrely V, Abramowitz L, Borg C, Francois E, Goere D, Huguet F, Peiffert D, Siproudhis L, Ducreux M, Bouché O (2017). "Anal cancer: French Intergroup Clinical Practice Guidelines for diagnosis, treatment and follow-up". Dig Liver Dis. doi:10.1016/j.dld.2017.05.011. PMID 28610905.
- ↑ Prigge ES, von Knebel Doeberitz M, Reuschenbach M (2017). "Clinical relevance and implications of HPV-induced neoplasia in different anatomical locations". Mutat. Res. 772: 51–66. doi:10.1016/j.mrrev.2016.06.005. PMID 28528690.
- ↑ Wieland U, Kreuter A (2017). "[Genital warts in HIV-infected individuals]". Hautarzt (in German). 68 (3): 192–198. doi:10.1007/s00105-017-3938-z. PMID 28160045.
- ↑ Köhn FM, Schultheiss D, Krämer-Schultheiss K (2016). "[Dermatological diseases of the external male genitalia : Part 2: Infectious and malignant dermatological]". Urologe A (in German). 55 (7): 981–96. doi:10.1007/s00120-016-0163-9. PMID 27364818.