Hamartoma
| Hamartoma | |
| ICD-10 | Q85.9 |
|---|---|
| ICD-9 | 757.32, 759.6 |
| DiseasesDB | 19785 |
| MeSH | D006222 |
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
A hamartoma is a focal malformation that resembles a neoplasm in the tissue of its origin. This is not a malignant tumor, and it grows at the same rate as the surrounding tissues. It is composed of tissue elements normally found at that site but that are growing in a disorganized mass. They occur in many different parts of the body and are most often asymptomatic and undetected unless seen on an image taken for another reason. Hamartomas result from an abnormal formation of normal tissue, although the underlying reasons for the abnormality are not fully understood. They grow along with, and at the same rate as, the organ from whose tissue they are made, and, unlike cancerous tumors, only rarely invade or compress surrounding structures significantly.
A hamartoma, while generally benign, can cause problems due to their location. When located on the skin, especially the face or neck, they can be extremely disfiguring, as in the case of a man with a hamartoma the size of a small orange on his eyelid.[1] They may obstruct practically any organ in the body, such as the eye, the colon, etc. They are particularly likely to cause major health issues when located in the hypothalamus, spleen or kidneys.
Lung
The most common hamartomas occur in the lungs. About 5-8% of all solitary lung tumors, about 75% of all benign lung tumors are hamartomas. They almost always arise from connective tissue and are generally formed of cartilage, fat, and connective tissue cells, although they may include many other types of cells. The great majority of them form in the connective tissue on the outside of the lungs, although about 10% form deep in the linings of the bronchii. They can be worrisome, especially if situated deep in the lung, as it is important and sometimes difficult to distinguish them from malignancies. An x-ray will often not provide definitive diagnosis, and even a CAT scan may be insufficient if the hamartoma atypically lacks cartilage and fat cells. Lung hamartomas are more common in men than in women and may present additional difficulties in smokers.
Some lung hamartomas can compress surrounding lung tissue to a degree, but this is generally not debilitative or even noticed by the patient, especially for the more common peripheral growths. They are treated, if at all, by surgical resection, with an excellent prognosis: generally, the only real danger is the inherent possibility of surgical complications.
Heart
Cardiac rhabdomyomas are hamartomas comprised of altered cardiac myocytes that contain large vacuoles and glycogen. They are the second most common tumor of the heart in children and infants (after fibromas). There is a strong association between cardiac rhabdomyomas and tuberous sclerosis (characterized by hamartomas of the central nervous system, kidneys and skin, as well as pancreatic cysts; 25-50% of patients with cardiac rhabdomyomas will have tuberous sclerosis, and up to 100% of patients with tuberous sclerosis will have cardiac masses by echocardiography. Symptoms depend on the size of the tumor, its location relative to the conduction system, and whether it obstructs blood flow. Symptoms are usually from congestive heart failure (in utero heart failure may occur). If patients survive infancy, their tumors may regress spontaneously; resection in symptomatic patients has good results.
Hypothalamus
One of the most troublesome hamartomas occurs on the hypothalamus. Unlike most such growths, a hypothalamic hamartoma is symptomatic; it most often causes gelastic seizures, and can cause visual problems, other seizures, rage disorders associated with hypothalamic diseases, and early onset of puberty. The symptoms typically begin in early infancy and are progressive, often into general cognitive and/or functional disability. Moreover, resection is usually difficult, as the growths are generally adjacent to, or even intertwined with, the optic nerve; however, the symptoms are resistant to medical control. Luckily, surgical techniques are improving and can result in immense improvement of prognosis. [2]
Kidneys, spleen, and other vascular organs
One general danger of hamartoma is that they may impinge into blood vessels, resulting in a risk of serious bleeding. Because hamartoma typically lacks elastic tissue, it may lead to the formation of aneurysms and thus possible hemorrhage. Where a hamartoma impinges into a major blood vessel, such as the renal artery, hemorrhage must be considered life-threatening.
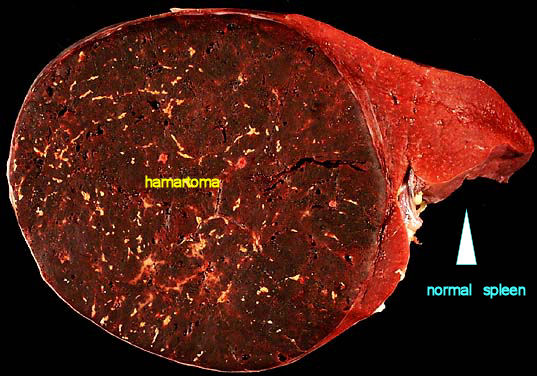
Hamartoma of the kidney is also called angiomyolipoma and can be associated with tuberous sclerosis. It is one of the more frequently seen hamartomas. The condition is more prevalent in women than men, and generally occurs in the right kidney. Hamartomas of the spleen are uncommon, but can be dangerous. About 50% of such cases manifest abdominal pain and they are often associated with hematologic abnormalities and spontaneous rupture.
Angiomyolipoma is not a hamartoma by definition, because fat and smooth muscles are not normal constituents of renal parenchyma. It is a Choristoma (microscopically normal cells or tissues in abnormal locations).
Cowden syndrome
Cowden Syndrome or Cowden Disease is a serious genetic disorder [3] characterized by multiple hamartomas. Usually skin hamartomas exist, and commonly (about 66% of cases) hamartoma of the thyroid gland exists. Additional growths can form in many parts of the body, especially in mucosa, the GI tract, bones, CNS, the eyes, and the genourinary tract. The hamartomas themselves may cause symptoms or even death, but morbidity is more often associated with increased occurrence of malignancies, usually in the breast or thyroid.
Notes
- ↑ http://dermatlas.med.jhmi.edu/derm/IndexDisplay.cfm?ImageID=2040682463
- ↑ http://www.emergemd.com/bniq2/article.asp?article_ref_id=20-1-1 Barrow Neurological Institute
- ↑ Mutation of PTEN gene on arm 10q or rarely germline mutation in BMPR1A
External links
Template:Tumors
Template:Phakomatoses and other congenital malformations not elsewhere classified
Template:SIB