Glucose-6-phosphate dehydrogenase deficiency
For patient information click here
Template:DiseaseDisorder infobox
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Priyamvada Singh, M.D. [2]
Overview
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is an X-linked recessive hereditary disease featuring abnormally low levels of the G6PD enzyme, which plays an important role in red blood cell function. Individuals with the disease may exhibit non-immune hemolytic anemia in response to a number of causes. It is closely linked to favism, a disorder characterized by a hemolytic reaction to consumption of broad beans, with a name derived from the Italian name of the broad bean (fava). Sometimes the name, favism, is alternatively used to refer to the enzyme deficiency as a whole.
Epidemiology and Demographics
- G6PDD is said to be the most common enzyme deficiency disease in the world, affecting approximately 400,000,000 people globally.[1]
- A side effect of this disease is that it confers protection against malaria, in particular the form of malaria caused by Plasmodium falciparum, the most deadly form of malaria.
- A similar relationship exists between malaria and sickle-cell disease. An explanation is that cells infected with the Plasmodium parasite are cleared more rapidly by the spleen. This phenomenon might give G6PD deficiency carriers an evolutionary advantage.
Classification
There are four forms of G6PD:
- Hereditary nonspherocytic hemolytic anemia
- Severe deficiency
- Mild deficiency
- Non-deficient variant
- Favism is a disorder characterized by hemolytic anemia in response to ingestion of fava beans. Favism as a diagnosis has been known since antiquity, perhaps in relation to Pythagoras, among others. All individuals with favism show G6PD deficiency. However, not all individuals with G6PD deficiency show favism. For example, in a small study of 757 Saudi men, more than 42% showed G6PD deficiency, but none reported symptoms of favism, despite fava in the diet.[2] Favism is known to be more prevalent in infants and children, and G6PD genetic variant can influence chemical sensitivity. Other than this, the detailed chemical relationship between favism and G6PD is not well known.
Pathophysiology
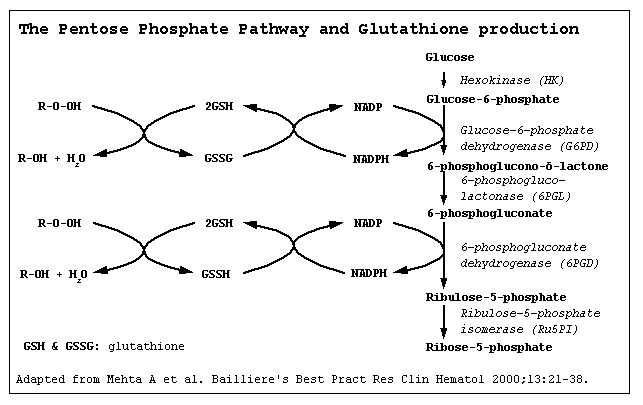
- Glucose-6-phosphate dehydrogenase (G6PD) is an enzyme in the pentose phosphate pathway, a metabolic pathway that supplies reducing energy to cells (most notably erythrocytes) by maintaining the level of the co-enzyme nicotinamide adenine dinucleotide phosphate (NADPH).
- The NADPH in turn maintains the level of glutathione in these cells that helps protect the red blood cells against oxidative damage. G6PD converts glucose-6-phosphate into 6-phosphoglucono-δ-lactone and is the rate-limiting enzyme of the pentose phosphate pathway.
- Patients with G6PD deficiency are at risk of hemolytic anemia in states of oxidative stress. This can be in severe infection, medication and certain foods. Broad beans contain high levels of vicine, divicine, convicine and isouramil — all are oxidants.
- In states of oxidative stress, all remaining glutathione is consumed. Enzymes and other proteins (including hemoglobin) are subsequently damaged by the oxidants, leading to electrolyte imbalance, membrane cross-bonding and phagocytosis and splenic sequestration of red blood cells. The hemoglobin is metabolized to bilirubin (causing jaundice at high concentrations) or excreted directly by the kidney (causing acute renal failure in severe cases).
- Deficiency of G6PD in the alternative pathway causes the build up of glucose and thus there is an increase of advanced glycation endproducts (AGE). The deficiency also causes a reduction of NADPH which is necessary for the formation of Nitric Oxide (NO). The high prevalence of diabetes mellitus type 2 and hypertension in Afro-Caribbeans in the West could be directly related to G6PD deficiency.[3]
- Some other epidemiological reports have pointed out, however, that G6PD seems to decrease the susceptibility to cancer, cardiovascular disease and stroke.
- Although female carriers can have a mild form of G6PD deficiency (dependent on the degree of inactivation of the unaffected X chromosome - see lyonization), homozygous females have been described; in these females there is co-incidence of a rare immune disorder termed chronic granulomatous disease (CGD).
History and Symptoms
History
- Patients are almost exclusively male, due to the X-linked pattern of inheritance, but female carriers can be clinically affected due to lyonization where random inactivation of an X-chromosome in certain cells creates a population of G6PD deficient red cells coexisting with normal red cells.
- History of hemolytic crises in response to:
- Certain drugs:
- Primaquine (an antimalarial)
- Sulphonamide antibiotics
- Sulphones (e.g. dapsone, used against leprosy)
- Other sulphur-containing drugs: glibenclamide (an anti-diabetic drug)
- Nitrofurantoin (an antibiotic often used for urinary tract infections)
- Vitamin K analogues
- Several others[4]
- Henna can cause a haemolytic crisis in G6PD deficient infants.[5]
- Certain foods, most notably broad beans
- Illness (severe infections)
- Diabetic ketoacidosis
- Certain drugs:
Symptoms
- Symptoms suggestive of anemia such as fatigue, palpitation
- Prolonged jaundice
- Hemolytic features like dark colored urine
- Abdominal or back pain
- Very severe crises can cause acute renal failure
Diagnosis
Laboratory diagnosis
The diagnosis is generally suspected when patients from certain ethnic groups develop anemia, jaundice and symptoms of hemolysis after challenge to any of the above causes, especially when there is a positive family history. At 2 to 4 days after introduction of the oxidative stress in patients with G6PD deficiency, onset of jaundice and dark urine occurs, with or without abdominal and back pain. The hemoglobin level decreases by 3 to 4 g/dL (30 to 40 g/L), and there is an appropriate increase in reticulocytes. The hemolysis spontaneously resolves in approximately 1 week as the older enzyme-depleted cells are replaced by new cells with sufficient G6PD to prevent further hemolysis. Additional laboratory findings in patients with G6PD deficiency include a negative direct and indirect antiglobulin (Coombs) test and the presence of "bite" or "blister" cells, produced when accumulated oxidized hemoglobin remains adherent to the erythrocyte membrane with an adjacent membrane-bound clear zone. Such cells are visible on this patient's peripheral blood smear. Because reticulocytes can have normal G6PD levels, measuring G6PD levels during an acute episode may produce a false-negative result.
Generally, tests will include:
- Complete blood count
- Reticulocyte count
- Haptoglobin (decreased in hemolysis);
- A "direct antiglobulin test" (Coombs' test) - this should be negative, as hemolysis in G6PD is not immune-mediated
- Liver enzymes (to exclude other causes of jaundice)
- In active G6PD, Heinz bodies can be seen in red blood cells on a blood film;
- TSH measurement.
- When there are sufficient grounds to suspect G6PD, a direct test for G6PD is the "Beutler fluorescent spot test", which has largely replaced an older test (the Motulsky dye-decolouration test).
- Other possibilities are direct DNA testing and/or sequencing of the G6PD gene.
Heinz bodies: Early diagnosis
When a macrophage in the spleen "sees" an RBC with a Heinz body, it removes the precipitate and a small piece of the membrane, leading to characteristic "bite cells". However, if a large number of Heinz bodies are produced, as in the case of G6PD deficiency, some Heinz bodies will nonetheless be visible when viewing RBCs that have been stained with crystal violet. This easy and inexpensive test can lead to an initial presumption of G6PD deficiency, which can be confirmed with the other tests.
Beutler fluorescent spot test: Late diagosis
The Beutler fluorescent spot test is a rapid and inexpensive test that visually identifies NADPH produced by G6PD under ultraviolet light. When the blood spot does not fluoresce, the test is positive; it can be false-positive in patients who are actively hemolysing. It can therefore only be done several weeks after a hemolytic episode.
Treatment
- In the acute phase of hemolysis, blood transfusions might be necessary. Blood transfusion is an important symptomatic measure, as the transfused red cells are generally not G6PD deficient.
- Dialysis in acute renal failure
- Some patients benefit from removal of the spleen (splenectomy), as this is an important site of red blood cell destruction. * Folic acid should be used in any disorder featuring a high red blood cell turnover.
- Although vitamin E and selenium have antioxidant properties, their use does not decrease the severity of G6PD deficiency.
Primary Prevention
- The most important measure is prevention - avoidance of the drugs and foods that cause hemolysis.
- Vaccination against some common pathogens (e.g. hepatitis A) may prevent infection-induced attacks.
References
- ↑ http://www.rddiagnostics.com/g6pd_faq.htm
- ↑ "Common G6PD variant from Saudi population". Retrieved 2007-10-28.
- ↑ Gaskin RS, Estwick D, Peddi R (2001). "G6PD deficiency: its role in the high prevalence of hypertension and diabetes mellitus". Ethnicity & disease. 11 (4): 749–54. PMID 11763298.
- ↑ "The G6PD Deficiency Homepage -- Table 2". Retrieved 2007-10-28.
- ↑ Raupp P, Hassan JA, Varughese M, Kristiansson B (2001). "Henna causes life threatening haemolysis in glucose-6-phosphate dehydrogenase deficiency". Arch. Dis. Child. 85 (5): 411–2. PMID 11668106.
bn:গ্লুকোজ-৬-ফসফেট ডিহাইড্রোজেনেজ স্বল্পতা bg:Глюкозо-6-фосфатдехидрогеназна недостатъчност de:G6PD-Mangel hr:Manjak enzima glukoza-6-fosfat dehidrogenaze he:חוסר G6PD simple:Favism th:โรคพร่องเอนไซม์ G-6-PD