Glomerular disease: Difference between revisions
No edit summary |
No edit summary |
||
| Line 26: | Line 26: | ||
2- Isolated proteinuria | 2- Isolated proteinuria | ||
They are categorized into several different pathological patterns, which are broadly grouped into '''non-proliferative''' or '''proliferative''' types. Diagnosing the pattern of GN is important because the outcome and treatment differs in different types. Primary causes are one which are intrinsic to the kidney, whilst secondary causes are associated with certain infections ([[bacterial]], [[viral]] or [[parasitic]] pathogens), [[drugs]], systemic disorders ([[SLE]], [[vasculitis]]) or [[ cancers]]. | They are categorized into several different pathological patterns, which are broadly grouped into '''non-proliferative''' or '''proliferative''' types. Diagnosing the pattern of GN is important because the outcome and treatment differs in different types. Primary causes are one which are intrinsic to the kidney, whilst secondary causes are associated with certain infections ([[bacterial]], [[viral]] or [[parasitic]] pathogens), [[drugs]], systemic disorders ([[SLE]], [[vasculitis]]) or [[ cancers]]. | ||
Revision as of 14:03, 30 April 2018
This page contains general information about Glomerular disease. For more information on specific types, please visit the pages on [[
| Glomerular disease | |
 | |
|---|---|
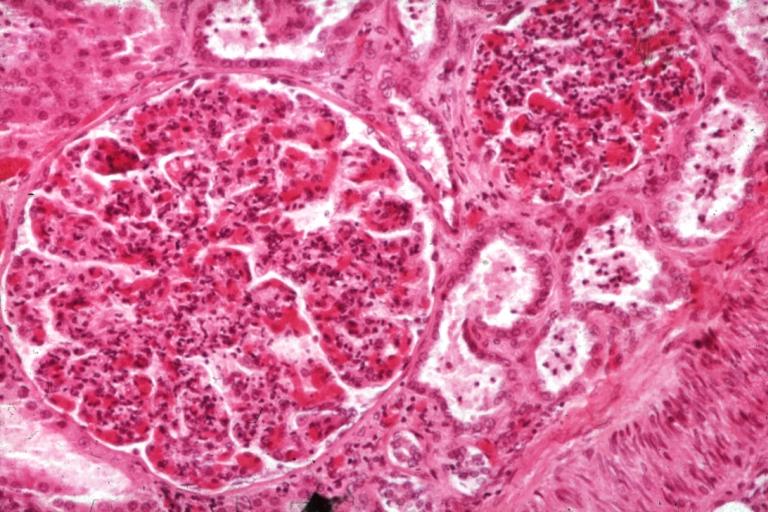
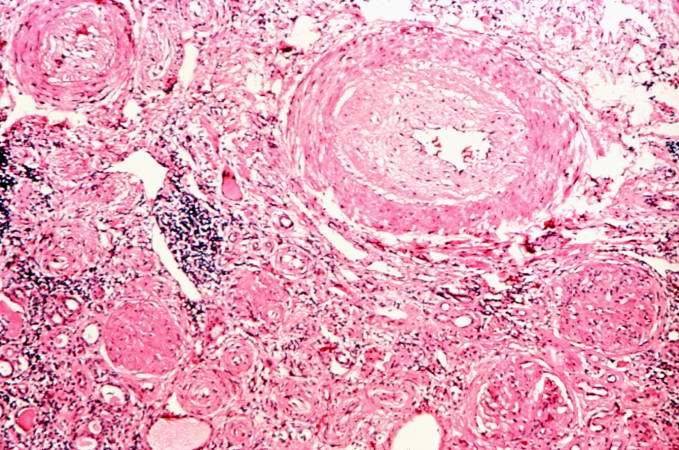
| Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mehrian Jafarizade, M.D [2]
Overview
Glomerular disease are conditions that affect the glomerulus. Glomerular diseases can be classified into glomerulonephritis characterized by an inflammatory process, and glomerulosclerosis which is characterized by fibrosis of the glomerulus.
Classification
Glomerular diseases can be classified as their clinical symptoms as below: Glomerular hematuria: 1- Glomerulonephritis 2- Isolated hematuria
Proteinuria: 1- Nephrotic syndrome 2- Isolated proteinuria
They are categorized into several different pathological patterns, which are broadly grouped into non-proliferative or proliferative types. Diagnosing the pattern of GN is important because the outcome and treatment differs in different types. Primary causes are one which are intrinsic to the kidney, whilst secondary causes are associated with certain infections (bacterial, viral or parasitic pathogens), drugs, systemic disorders (SLE, vasculitis) or cancers.
Non Proliferative Glomerulonephritis
This is characterised by a lack of hypercellularity in the glomeruli. They usually cause nephrotic syndrome. This includes the following types:
1. Minimal change GN
This form of GN causes 80% of nephrotic syndrome in children, but only 20% in adults. As the name indicates, there are no changes visible on simple light microscopy, but on electron microscopy there is fusion of podocytes (supportive cells in the glomerulus). Immunohistochemistry staining is negative. Treatment consists of supportive care for the massive fluid accumulation in the patients body (= oedema) and as well as steroids to halt the disease process (e.g. Prednisone 1 mg/ kg). Over 90% of children respond well to steroids, being essentially cured after 3 months of treatment. Adults have a lower response rate (80%). Failure to respond to steroids ('steroid resistant') or return of the disease when steroids are stopped ('steroid dependent') may require cytotoxic therapy (e.g. cyclosporin) which is associated with many side-effects. As we all may know
2. Focal Segmental Glomerulosclerosis (FSGS)
FSGS may be primary or secondary to reflux nephropathy, Alport syndrome, heroin use or HIV. FSGS presents as a nephrotic syndrome with varying degrees of impaired renal function (seen as a rising serum creatinine, hypertension). As the name suggests, only certain foci of glomeruli within the kidney are affected, and then only a segment of an individual glomerulus.
The pathological lesion is sclerosis (fibrosis) within the glomerulus and hyalinisation of the feeding arterioles, but no increase in the number of cells (hence non proliferative). The hyaline is an amorphous material, pink, homogeneous, resulting from combination of plasma proteins, increased mesangial matrix and collagen. Staining for antibodies and complement is essentially negative. Steroids are often tried but not shown to be effective. 50% of people with FSGS continue to have progressive deterioration of kidney function, ending in renal failure.
3. Membranous glomerulonephritis
Presents as nephrotic syndrome, leading cause in adults (35%). It is usually idiopathic, but may be associated with cancers (lung, bowel), infection (hepatitis, malaria), drugs (penicillamine), SLE. The basement membrane on which the glomerular cells sit is thickened, but no increase in cells. Immune staining shows diffuse granular uptake of IgG (immunoglobulin G) and complement type 3. A third of people continue having the disease, 1/3 remit, 1/3 progress to end-stage kidney failure. As glomerulonephritis progresses (in any type), the tubules of the kidney (which are separate to the glomerulus) also become affected, showing atrophy and hyalinisation. The kidney grossly appears shrunken. Treatment with steroids is attempted if it is progressive.
Proliferative Glomerulonephritis
This type is characterised by increased number of cells in the glomerulus (hypercellular). Usually present as a nephritic syndrome and usually progress to end-stage renal failure (ESRF) over weeks to years (depending on type).
1. IgA disease (Berger's nephropathy)
This is the most common type of glomerulonephritis in adults world-wide. It usually presents as macroscopic haematuria (visibly bloody urine). It occasionally presents as a nephrotic syndrome. It often affects young males after an upper respiratory tract infection. Microscopic examination of biopsy specimens shows increased number of mesangial cells with increased matrix (the 'cement' which holds everything together). Immuno-staining is positive for immunoglobulin A deposits within the matrix. Prognosis is variable, 20% progress to ESRF. Steroids and immunosuppression are not effective treatments for this disease; ACE inhibitors are the mainstay of treatment.
2. Post-infectious Glomerulonephritis
Post-infectious glomerulonephritis occurs after Streptococcal infection - usually of the skin, after a latency of 10 days. This condition is essentially defined as an inflammation of the kidneys. Light microscopy shows diffuse hypercellularity due to proliferation of endothelial and mesangial cells, inflammatory infiltrate with neutrophils and with monocytes. The Bowman space is reduced (compressed), in severe cases might see cresent formation [see later]. However, biopsy is seldom done because the disease usually regresses. Patients present with a nephritic syndrome. Diagnosis is suggested by positive streptococcal titers in the blood (ASOT). Treatment is supportive, and the disease resolves (as a rule) in 2 weeks.
3. Mesangiocapillary Glomerulonephritis
This is primary, or secondary to SLE, viral hepatitis, hypocomplementemia. One sees 'hypercellular and hyperlobular' glomeruli due to proliferation of both cells and the matrix within the mesangium. Presents usually with as a nephrotic syndrome but can be nephritic, with inevitable progression to ESRF.
4. Rapidly progressive Glomerulonephritis (Crescentic GN)
As the name suggests, this type has a poor prognosis, with rapid progression to kidney failure over weeks. Any of the above types of GN can be rapidly progressive. Additionally two further causes present as solely RPGN. One is Goodpasture's syndrome. This is an autoimmune disease whereby antibodies are directed against antigens found in the kidney and lungs. As well as kidney failure, patient have hemoptysis (cough up blood). High dose immunosupression is required (intravenous methylprednisone) and cyclophosphamide, plus plasmapharesis. Immunohistochemistry staining of tissue specimens shows linear IgG deposits. The second cause is vasculitic disorders such as Wegener's and polyarteritis. There is a lack of immune deposits on staining, but blood tests are positive for ANCA antibody.
Pathophysiology
Microscopic Pathology
-
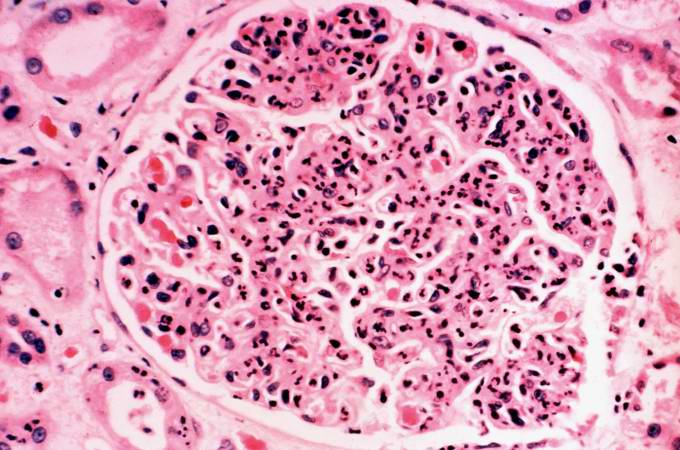
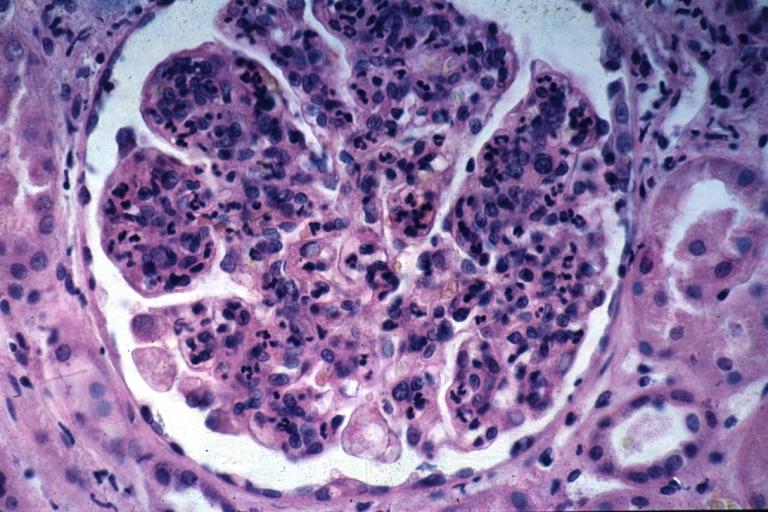
Glomerulonephritis: Micro H&E med mag; an excellent example of AGN with many neutrophils
-
Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis.
Glomerulonephritis Videos
Rapidly progressive glomerulonephritis
{{#ev:youtube|CqSyj4cVZPE}}
Chronic glomerulonephritis
{{#ev:youtube|eA1vYarRAWo}}
Images
-
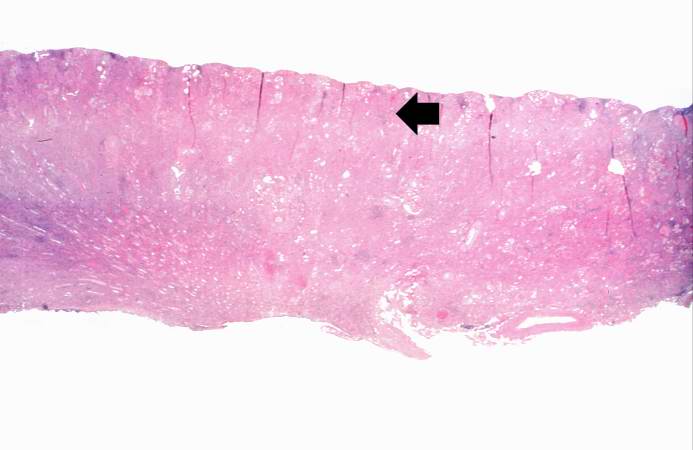
This is a low-power photomicrograph of a saggital section of end stage chronic glomerulonephritis (GN). Note the marked thinning of the cortex (arrow).
-
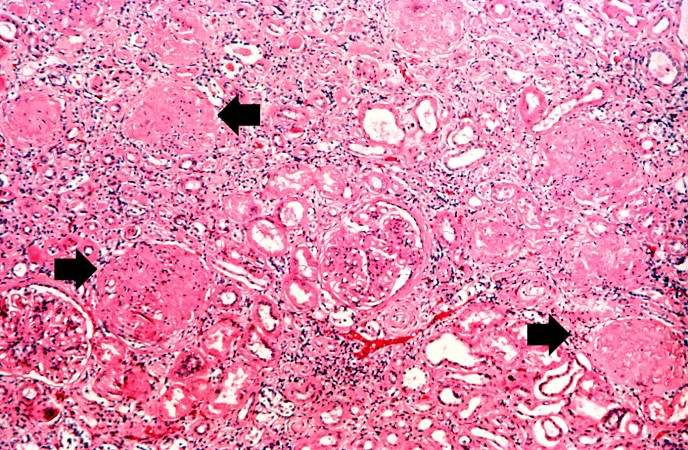
This is a higher-power photomicrograph of hyalinized glomeruli (arrows) and glomeruli with thick basement membranes.
-
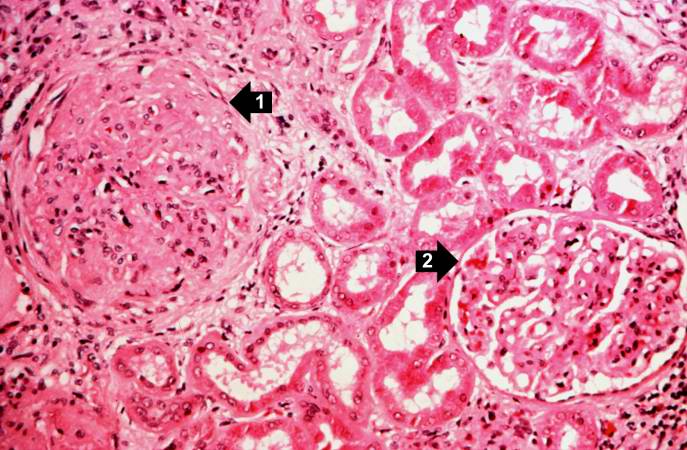
This is a higher-power photomicrograph of hyalinized glomeruli (1) and glomeruli with thickened basement membranes (2).
-
This is a photomicrograph of interstitial and vascular lesions in end stage renal disease.
-
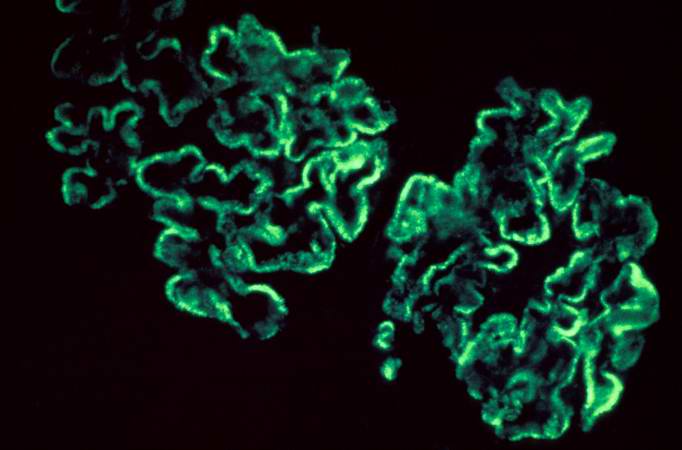
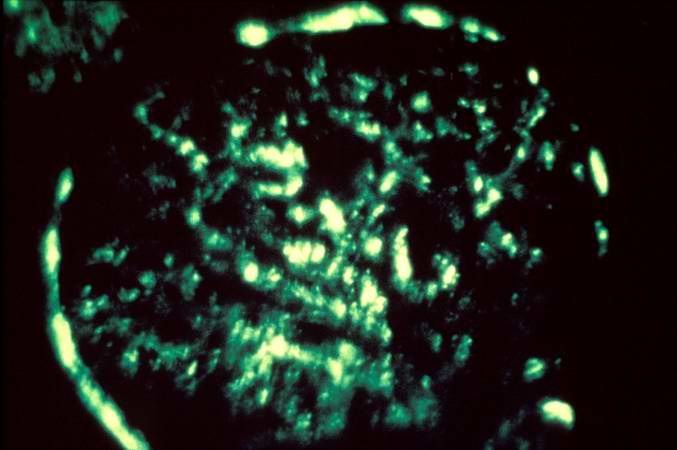
This is an immunofluorescent photomicrograph of granular membranous immunofluorescence (immune complex disease). The antibody used for these studies was specific for IgG.
-
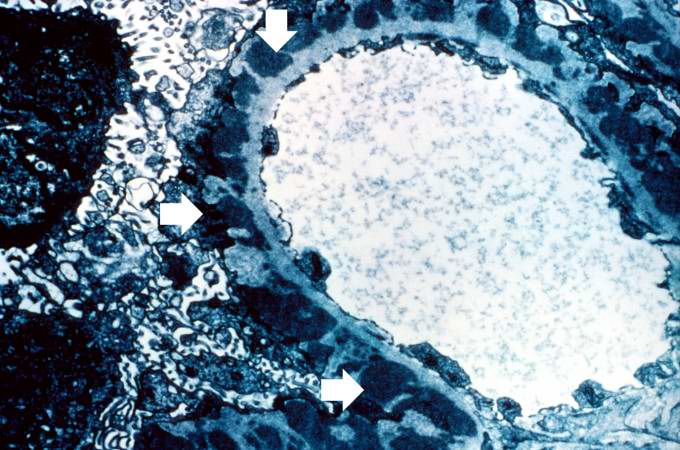
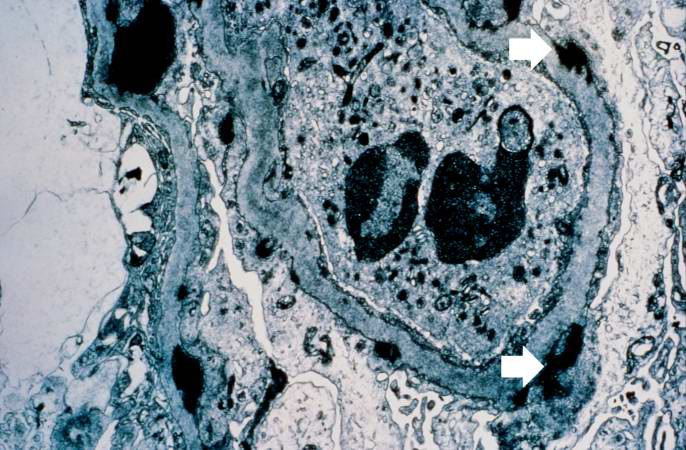
This is an electron micrograph of subepithelial granular electron dense deposits (arrows) which correspond to the granular immunofluorescence seen in the previous image.
-
This is a photomicrograph of a glomerulus from another case with acute poststreptococcal glomerulonephritis. In this case the immune complex glomerular disease is ongoing with necrosis and accumulation of neutrophils in the glomerulus.
-
This immunofluorescent photomicrograph of a glomerulus from a case of acute poststreptococcal glomerulonephritis shows a granular immunofluorescence pattern consistent with immune complex disease. The primary antibody used for this staining was specific for IgG; however antibodies for complement would show a similar pattern.
-
This electron micrograph demonstrates scattered subepithelial dense deposits (arrows) and a polymorphonuclear leukocyte in the lumen.
-
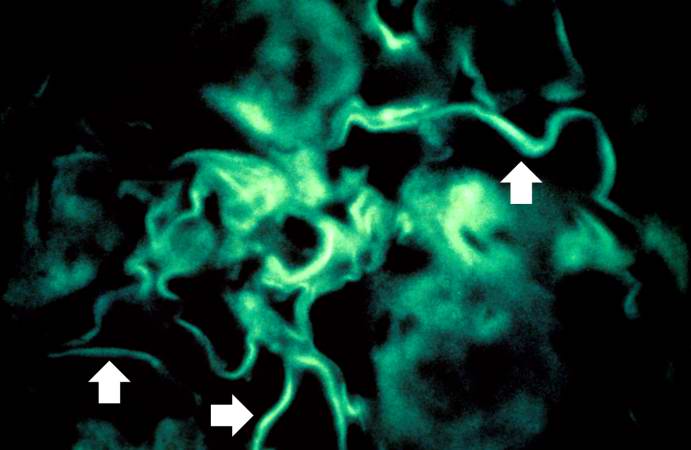
For comparison this is an immunofluorescent photomicrograph of a glomerulus from a patient with Goodpasture's syndrome. The linear (arrows) immunofluorescence is characteristic of Goodpasture's syndrome.
Images:
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Associate Editor(s)-in-Chief: Syed Hassan A. Kazmi BSc, MD [4]
Overview
Glomerulonephritis may be proliferative or non-proliferative and may be associated with nephrotic or nephritic features. The various types of glomerulonephritides should be differentiated from each other based on associations, presence of pitting edema, hemeturia, hypertension, hemoptysis, oliguria, peri-orbital edema, hyperlipidemia, type of antibodies, light and electron microscopic features.
Differential Diagnosis
The following table differentiates between various types of glomerulonephritides:
| Glomerulonephritis | Sub-entity | Causes and associations | History and Symtoms | Laboratory Findings | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hyperlipidemia and hypercholesterolemia | Nephrotic features | Nephritic features | ANCA | Anti-glomerular basement membrane antibody (Anti-GBM antibody) | Immune complex formation | Light microscope | Electron microscope | Immunoflourescence pattern | ||||||||||
| History | Pitting edema | Hemeturia (pre-dominantly microscopic) | Hypertension | Hemoptysis | Oliguria | Peri-orbital edema | ||||||||||||
| Non-proliferative | Minimal change disease |
|
|
+ |
- |
- |
- |
+/- |
- |
+ |
+ |
- |
- |
- |
- |
|
|
- |
| Focal segmental glomerulosclerosis |
|
|
+ | - | - | - | +/- | - | + | + | - | - | - | - |
|
|
- | |
| Membranous glomerulonephritis |
|
+ | - | - | - | +/- | - | + | + | - | - | - | + |
|
|
- | ||
| Proliferative | IgA nephropathy |
|
|
+/- | + | + | - | + | +/- | - | - | + | - | - | + |
|
|
- |
| Rapidly progressive glomerulonephritis |
|
|
+/- | + | + | + | + | + | - | - | + | - | + | + |
|
|
+ (Linear) | |
|
|
+/- | + | + | + | + | + | - | - | + | - | - | + |
|
|
+ (Granular) | ||
|
|
+/- | + | + | + | + | + | - | - | + | + (C-ANCA) | - | - |
|
- (pauci-immune) | +/- | ||
|
|
+/- | + | + | + | + | + | - | - | + |
+ (C-ANCA) |
- | - |
|
- (pauci-immune) | - | ||
|
|
+/- | + | + | + | + | + | - | - | + |
+ (P-ANCA) |
- | - |
|
- (pauci-immune) | - | ||
| Membranoproliferative glomerulonephritis |
|
|
+/- | + | + | + | + | + | - | + | - | - | - | + |
|
|
+ (Granular) | |