Gestational trophoblastic disease: Difference between revisions
No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
'''For patient information on Choriocarcinoma, click [[Choriocarcinoma (patient information)|here]]''' | '''For patient information on Choriocarcinoma, click [[Choriocarcinoma (patient information)|here]]''' | ||
{{ | {{Infobox disease | ||
| Name = Gestational trophoblastic disease | |||
| Image = Intermediate_trophoblast_3_-_low_mag.jpg | |||
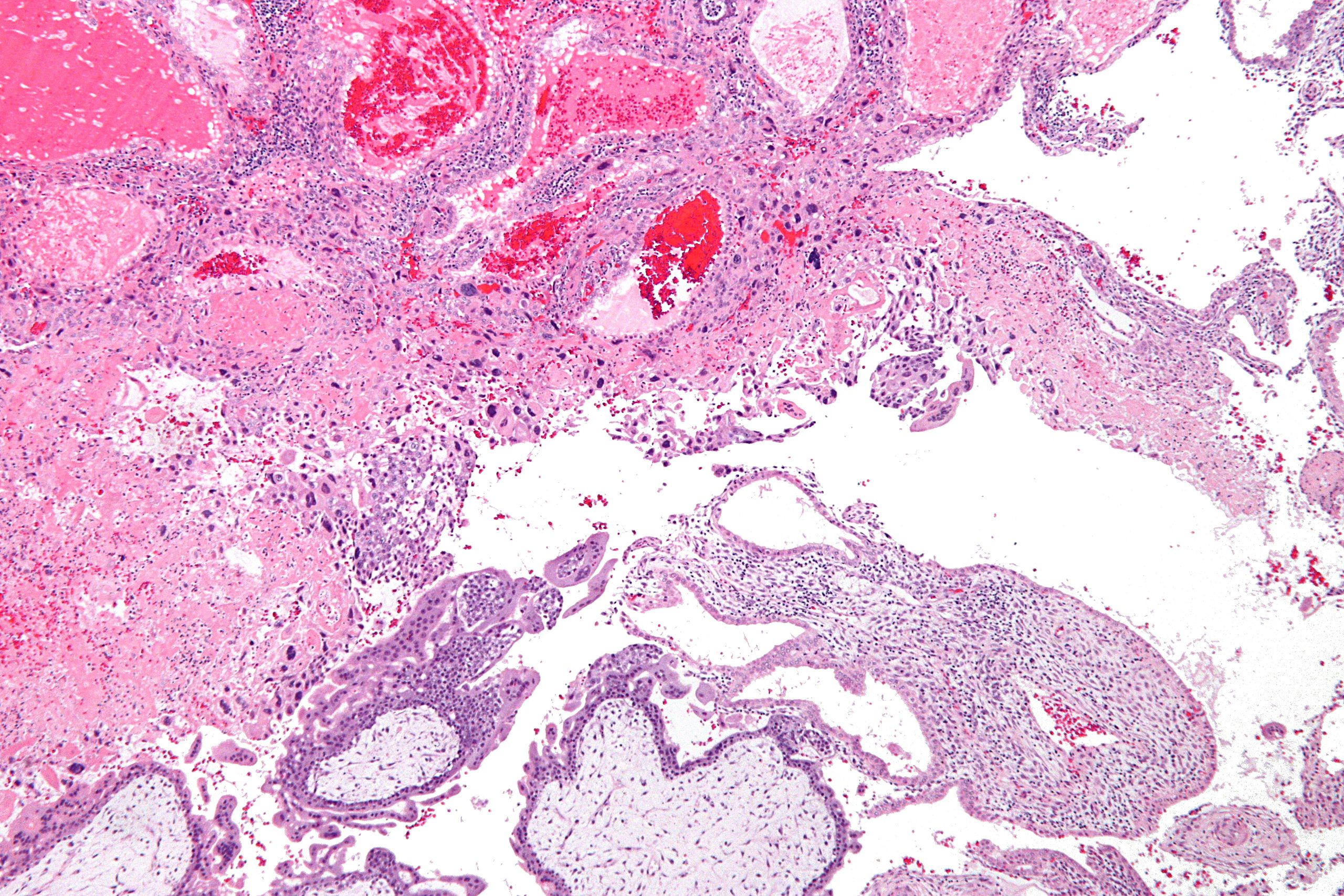
| Caption = [[Micrograph]] of [[intermediate trophoblast]], [[decidua]] and a hydatidiform mole (bottom of image). [[H&E stain]]. | |||
| field = [[Oncology]] | |||
| DiseasesDB = 2602 | | |||
ICD10 = | | ICD10 = | | ||
ICD9 = | | ICD9 = | | ||
| Line 14: | Line 15: | ||
OMIM = | | OMIM = | | ||
MedlinePlus = 001496 | | MedlinePlus = 001496 | | ||
eMedicineSubj = article | | |||
eMedicineTopic = 279116 | | |||
MeshID = D031901 | | MeshID = D031901 | | ||
}} | }} | ||
{{SI}} | {{SI}} | ||
{{CMG}} | {{CMG}} | ||
'''Gestational trophoblastic disease''' (GTD) is a term used for a group of pregnancy-related [[tumour]]s. These tumours are rare, and they appear when cells in the womb start to proliferate uncontrollably. The cells that form gestational trophoblastic tumours are called trophoblasts and come from tissue that grows to form the [[placenta]] during pregnancy. | |||
== | There are several different types of GTD. [[Hydatidiform mole]]s are, in most cases, benign, but may, sometimes, develop into invasive moles, or, in rare cases, into [[choriocarcinoma]], which is likely to spread quickly,<ref>{{cite journal |author=Seckl MJ, Sebire NJ, Berkowitz RS |title=Gestational trophoblastic disease |journal=Lancet |volume=376 |issue=9742 |pages=717–29 |date=August 2010 |pmid=20673583 |doi=10.1016/S0140-6736(10)60280-2 |url=http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(10)60280-2}}</ref><ref>{{cite journal |author=Lurain JR |title=Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole |journal=Am. J. Obstet. Gynecol. |volume=203 |issue=6 |pages=531–9 |date=December 2010 |pmid=20728069 |doi=10.1016/j.ajog.2010.06.073 |url=http://linkinghub.elsevier.com/retrieve/pii/S0002-9378(10)00853-7}}</ref> but which is very sensitive to [[chemotherapy]], and has a very good prognosis. Gestational trophoblasts are of particular interest to cell biologists because, like cancer, these cells invade tissue (the uterus), but unlike cancer, they sometimes "know" when to stop.{{Citation needed|date=August 2011}} | ||
GTD can simulate pregnancy, because the uterus may contain fetal tissue, albeit abnormal. This tissue may grow at the same rate as a normal pregnancy, and produces chorionic gonadotropin, a hormone which is measured to monitor fetal well-being.<ref>Gestational trophoblastic disease: Epidemiology, clinical manifestations and diagnosis. Chiang JW, Berek JS. In: UpToDate [Textbook of Medicine]. Basow, DS (Ed). Massachusetts Medical Society, Waltham, Massachusetts, USA, and Wolters Kluwer Publishers, Amsterdam, The Netherlands. 2010.</ref> | |||
While GTD overwhelmingly affects women of child-bearing age, it may rarely occur in postmenopausal women.<ref>{{cite journal |author=Chittenden B, Ahamed E, Maheshwari A |title=Choriocarcinoma in a postmenopausal woman |journal=Obstet Gynecol |volume=114 |issue=2 Pt 2 |pages=462–5 |date=August 2009 |pmid=19622962 |doi=10.1097/AOG.0b013e3181aa97e7 }}</ref> | |||
==Classification== | ==Classification== | ||
Revision as of 15:55, 6 October 2015
For patient information on Hydatiform mole, click here
For patient information on Choriocarcinoma, click here
| Gestational trophoblastic disease | |
| Classification and external resources | |
| |
|---|---|
| Micrograph of intermediate trophoblast, decidua and a hydatidiform mole (bottom of image). H&E stain. | |
| DiseasesDB | 2602 |
| MedlinePlus | 001496 |
| eMedicine | article/279116 |
| MeSH | D031901 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Gestational trophoblastic disease (GTD) is a term used for a group of pregnancy-related tumours. These tumours are rare, and they appear when cells in the womb start to proliferate uncontrollably. The cells that form gestational trophoblastic tumours are called trophoblasts and come from tissue that grows to form the placenta during pregnancy.
There are several different types of GTD. Hydatidiform moles are, in most cases, benign, but may, sometimes, develop into invasive moles, or, in rare cases, into choriocarcinoma, which is likely to spread quickly,[1][2] but which is very sensitive to chemotherapy, and has a very good prognosis. Gestational trophoblasts are of particular interest to cell biologists because, like cancer, these cells invade tissue (the uterus), but unlike cancer, they sometimes "know" when to stop.[citation needed]
GTD can simulate pregnancy, because the uterus may contain fetal tissue, albeit abnormal. This tissue may grow at the same rate as a normal pregnancy, and produces chorionic gonadotropin, a hormone which is measured to monitor fetal well-being.[3]
While GTD overwhelmingly affects women of child-bearing age, it may rarely occur in postmenopausal women.[4]
Classification
There are profound differences in pathological morphology and clinical behavior in various forms of GTD. Types include:
- Abnormal placenta, mostly due to abnormal fertilization
- Hydatidiform mole (HM)
- Frank malignant tumors of trophoblast
- Invasive mole, choriocarcinoma (CCA)
- Placental site trophoblastic tumor (PSTT)
- Epithelioid trophoblastic tumor (ETT)
- Not true neoplasms, representing abnormally formed placentas
- Exaggerated placenta site (EPS)
- Placental site nodule (PSN)
Pathophysiology
It is the result of a (purely chance) genetic error during the fertilization process that in turn causes the growth of abnormal tissue (which is not an embryo) within the uterus. The growth of this material is disproportionately rapid when compared to normal fetal growth.
References
- ↑ Seckl MJ, Sebire NJ, Berkowitz RS (August 2010). "Gestational trophoblastic disease". Lancet. 376 (9742): 717–29. doi:10.1016/S0140-6736(10)60280-2. PMID 20673583.
- ↑ Lurain JR (December 2010). "Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole". Am. J. Obstet. Gynecol. 203 (6): 531–9. doi:10.1016/j.ajog.2010.06.073. PMID 20728069.
- ↑ Gestational trophoblastic disease: Epidemiology, clinical manifestations and diagnosis. Chiang JW, Berek JS. In: UpToDate [Textbook of Medicine]. Basow, DS (Ed). Massachusetts Medical Society, Waltham, Massachusetts, USA, and Wolters Kluwer Publishers, Amsterdam, The Netherlands. 2010.
- ↑ Chittenden B, Ahamed E, Maheshwari A (August 2009). "Choriocarcinoma in a postmenopausal woman". Obstet Gynecol. 114 (2 Pt 2): 462–5. doi:10.1097/AOG.0b013e3181aa97e7. PMID 19622962.