Generic drug
|
WikiDoc Resources for Generic drug |
|
Articles |
|---|
|
Most recent articles on Generic drug Most cited articles on Generic drug |
|
Media |
|
Powerpoint slides on Generic drug |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Generic drug at Clinical Trials.gov Clinical Trials on Generic drug at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Generic drug
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Generic drug Discussion groups on Generic drug Patient Handouts on Generic drug Directions to Hospitals Treating Generic drug Risk calculators and risk factors for Generic drug
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Generic drug |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Overview
A generic drug (pl. generic drugs, short: generics) is a drug which is produced and distributed without patent protection. A generic must contain the same active ingredients as the original formulation. In most cases, it is considered bioequivalent to the brand name counterpart with respect to pharmacokinetic and pharmacodynamic properties. By extension, therefore, generics are assumed to be identical in dose, strength, route of administration, safety, efficacy, and intended use. In most cases, generic products are not available until the patent protections afforded to the original developer have expired. When generic products become available, the market competition often leads to substantially lower prices for both the original brand name product and the generic forms. The time it takes a generic drug to appear on the market varies. Drug patents give twenty years of protection, but they are applied for before clinical trials begin, so the effective life of a drug patent tends to be between seven and twelve years.
Economics
The principal reason for the relatively low price of generic medicines is that these companies incur fewer costs in creating the generic drug, and are therefore able to maintain profitability while offering the drug at a lower cost to consumers. The costs of these generic drugs are so low that many developing countries can easily afford. For example Thailand is going to import millions of generic version pills of Plavix, a blood-thinning treatment to prevent heart attacks, costs just 3 US cents per pill from India, the leading manufacturer of generic drugs.
Generic manufacturers do not incur the cost of drug discovery, and instead are able to reverse-engineer known drug compounds to allow them to manufacture bioequivalent versions. Generic manufacturers also do not bear the burden of proving the safety and efficacy of the drugs through clinical trials, since these trials have already been conducted by the brand name company. In most countries, generic manufacturers must only prove that their preparation is bioequivalent to the existing drug in order to gain regulatory approval. It has been estimated that the average cost to brand-name drug companies of discovering and testing a new innovative drug (with a new chemical entity) may be as much as $800 million.[1] However, these estimations are strongly disputed as much too high.
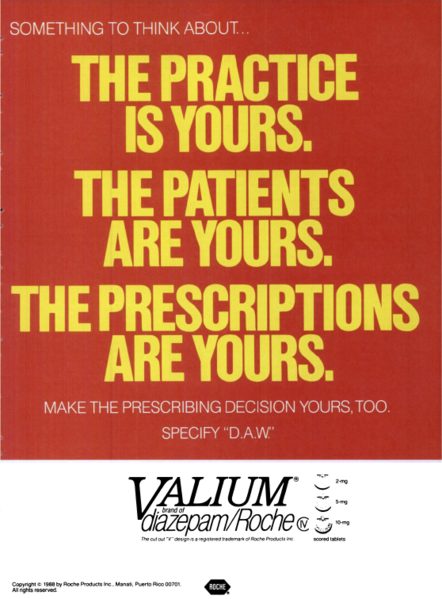
Generic drug companies may also receive the benefit of the previous marketing efforts of the brand-name drug company, including media advertising, presentations by drug representatives, and distribution of free samples. Many of the drugs introduced by generic manufacturers have already been on the market for a decade or more, and may already be well-known to patients and providers (although often under their branded name).
Prior to the expiration of a drug patent, a brand name company enjoys a period of "market exclusivity" or monopoly, in which the company is able to set the price of the drug at the level which maximizes profitability. This price often greatly exceeds the production costs of the drug, which can enable the drug company to make a significant profit on their investment in research and development. The advantage of generic drugs to consumers comes in the introduction of competition, which prevents any single company from dictating the overall market price of the drug. With multiple firms, the profit-maximizing price generally reflects the ongoing cost of producing the drug, which is usually much lower than the monopoly price.
Patent issues
When can a generic drug be produced?
When a pharmaceutical company first markets a drug, it is usually under a patent that allows only the pharmaceutical company that developed the drug to sell it. Generic drugs can be legally produced for drugs where: 1) the patent has expired, 2) the generic company certifies the brand company's patents are either invalid, unenforceable or will not be infringed, 3) for drugs which have never held patents, or 4) in countries where a patent(s) is/are not in force. The expiration of a patent removes the monopoly of the patent holder on drug sales licensing. Patent lifetime differs from country to country, and typically there is no way to renew a patent after it expires. A new version of the drug with significant changes to the compound could be patented, but this requires new clinical trials and does not prevent the generic versions of the original drug.
This allows the company to recoup the cost of developing that particular drug. After the patent on a drug expires, any pharmaceutical company can manufacture and sell that drug. Since the drug has already been tested and approved, the cost of simply manufacturing the drug will be a fraction of the original cost of testing and developing that particular drug.
Challenging patents
Brand-name drug companies have used a number of strategies to extend the period of market exclusivity on their drugs, and prevent generic competition. This may involve aggressive litigation to preserve or extend patent protection on their medicines, a process referred to by critics as "evergreening." Patents are typically issued on novel pharmacological compounds quite early in the drug development process, at which time the 'clock' to patent expiration begins ticking. Later in the process, drug companies may seek new patents on the production of specific forms of these compounds, such as single enantiomers of drugs which can exist in both "left-handed" and "right-handed" forms,[2] different inactive components in a drug salt,[3] or a specific hydrate form of the drug salt.[4] If granted, these patents 'reset the clock' on patent expiration. These sorts of patents may later be targeted for invalidation by generic drug manufacturers.[5][6][7]
Generic drug exclusivity
The U.S. Food and Drug Administration offers a 180 day exclusivity period to generic drug manufacturers in specific cases. During this period only one (or sometimes a few) generic manufacturers can produce the generic version of a drug. This exclusivity period is only used when a generic manufacturer argues that a patent is invalid or is not violated in the generic production of a drug, and the period acts as a reward for the generic manufacturer who is willing to risk liability in court and the cost of patent court litigation. There is often contention around these 180 day exclusivity periods because a generic producer does not have to produce the drug during this period and can file an application first to prevent other generic producers from selling the drug.
Large pharmaceutical companies often spend thousands of dollars protecting their patents from generic competition. Apart from litigation, companies use other methods such as reformulation or licensing a subsidiary (or another company) to sell generics under the original patent. Generics sold under license from the patent holder are known as authorized generics; they are not affected by the 180 day exclusivity period as they fall under the patent holder's original drug application.
A prime example of how this works is simvastatin (Zocor), a popular drug created and manufactured by U.S. based pharmaceutical Merck & Co., which lost its US patent protection on June 23, 2006. India-based Ranbaxy Laboratories (at the 80-mg strength) and Israel-based Teva Pharmaceutical Industries (at all other strengths) received 180 day exclusivity periods for simvastatin; due to Zocor's popularity, both companies began marketing their products immediately after the patent expired. However, Dr. Reddy's Laboratories also markets an authorized generic version of simvastatin under license from Zocor's manufacturer, Merck & Co.; some packages of Dr. Reddy's simvastatin even show Merck as the actual manufacturer and have Merck's logo on the bottom.
Approval and regulation
Ensuring bioequivalence
Most nations require generic drug manufacturers to prove that their formulation exhibits bioequivalence to the innovator product. Over the past several years there have been studies that have shown the effectiveness and safety of some generic drugs. Generic drugs are always less expensive and can save patients and insurance companies thousands of dollars supposedly without compromising the quality of care. The FDA must approve generic drugs just as innovator drugs must be approved. Bioequivalence, however, does not mean that generic drugs are exactly the same as their innovator product counterparts, as chemical differences do exist. Some doctors and patients emphatically believe that certain generic drugs are not as effective as the products they are meant to replace (ie. Prozac, Oxycontin), and consumers would undoubtedly benefit from more clinical studies done on drug by drug basis. Generic drugs start out at first being fairly expensive, however the price of the generic product decreases as the rate of production increases.
As an interesting case study in the use of generic equivalents of name-brand agents, warfarin has been only available under the trade name Coumadin in North America until recently. Warfarin (either under the trade name or the generic equivalent) has a narrow therapeutic window and requires frequent blood tests to make sure patients do not have a subtherapeutic or a toxic level. A study performed in the Canadian province of Ontario showed that replacing Coumadin with generic warfarin was considered safe.[8] In spite of the study, many physicians are not comfortable in allowing their patients to take the branded generic equivalent agents.[9]
U.S. generics approval process
Enacted in 1984, the U.S. Drug Price Competition and Patent Term Restoration Act, informally known as the "Hatch-Waxman Act", standardized U.S. procedures for recognition of generic drugs. An applicant files an Abbreviated New Drug Application (or "ANDA") with the Food and Drug Administration (FDA) and seeks to demonstrate therapeutic equivalence to a specified,previously approved "reference listed drug." When an ANDA is approved, the FDA adds the drug to its Approved Drug Products list, also known as the "Orange Book", and annotates the list to show equivalence between the reference listed drug and the approved generic. The FDA also recognizes drugs using the same ingredients with different bioavailability and divides them into therapeutic equivalence groups. For example, as of 2006 diltiazem hydrochloride had four equivalence groups all using the same active ingredient but considered equivalent only within a group.[10]
See also
- Approval process for generic drugs
- Clinical monitoring
- Clinical protocol
- Clinical research
- Clinical trial management
- Research exemption (in patent law)
References
- ↑ "The price of innovation: new estimates of drug development cost" (pdf) DiMasi J.A. et al.: , Journal of Health Economics 22(2003), 151-185. Accessed 31st of May 2007
- ↑ [1] U.S. Patent 4,721,723: Dextro-rotatory enantiomer of methyl alpha-5 (4,5,6,7-tetrahydro (3,2-c) thieno pyridyl) (2-chlorophenyl)-acetate
- ↑ [2] U.S. Patent 4,879,303: Amlodipine besylate
- ↑ [3] U.S. Patent 4,721,723: Paroxetine hydrochloride hemihydrate
- ↑ [4] Brisol-Myers Squibb press release on successful defense of Plavix patent
- ↑ [5] Apotex press release on successful challenge of Norvasc patent
- ↑ [6] Apotex press release on successful challenge of Paxil patent
- ↑ Pereira JA, Holbrook AM, Dolovich L, Goldsmith C, Thabane L, Douketis JD, Crowther MA, Bates SM, Ginsberg JS. (2005). "Are brand-name and generic warfarin interchangeable? Multiple n-of-1 randomized, crossover trials". Ann Pharmacother. 39 (7–8): 1188–93. PMID 15914517.
- ↑ Pereira JA, Holbrook AM, Dolovich L, Goldsmith C, Thabane L, Douketis JD, Crowther M, Bates SM, Ginsberg JS. (2005). "Are brand-name and generic warfarin interchangeable? A survey of Ontario patients and physicians" (PDF). Can J Clin Pharmacol. 12 (3): e229–39. PMID 16278495.
- ↑ Approved Drug Products with Therapeutic Equivalence Evaluations, Preface. - an explanation of FDA terms and procedures
External links
- USFDA, Office of Generic Drugs
- UK Department of Health, generic drugs
- USAN (broken link) stem name list
- Generic Pharmaceutical Manufacturers Resource Center
- The Medical Letter on Drugs and Therapeutics
- Fighting generic competition: strategies for research-based companies - Urch Publishing
- Profiting from Drug Patent Expirations