Gastrointestinal stromal tumor pathophysiology: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
|||
| Line 16: | Line 16: | ||
*Macroscopically these tumours are rounded with frequent haemorrhagic change. Larger tumours also may demonstrate necrosis and cystic change. Size is variable ranging form 1 to 30cm. | *Macroscopically these tumours are rounded with frequent haemorrhagic change. Larger tumours also may demonstrate necrosis and cystic change. Size is variable ranging form 1 to 30cm. | ||
*Histology demonstrates a relatively cellular | *Histology demonstrates a relatively cellular [[tumor]] comprised of spindle cells (70-80%) and or plump epithelioid cells (20-30%). They appear to arise from the muscularis propria layer.<ref>{{Cite web | title = Gastrointestinal stromal tumour| url = http://radiopaedia.org/articles/gastrointestinal-stromal-tumour-1}}</ref> | ||
[[Image:gist.jpg|thumb|left|Gastrointestinal stromal tumor of stomach. Courtesy of Ed Uthman, MD.]] | [[Image:gist.jpg|thumb|left|Gastrointestinal stromal tumor of stomach. Courtesy of Ed Uthman, MD.]] | ||
<br clear="left"/> | <br clear="left"/> | ||
Revision as of 20:28, 3 September 2015
|
Gastrointestinal stromal tumor Microchapters |
|
Differentiating Gastrointestinal stromal tumor from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Gastrointestinal stromal tumor pathophysiology On the Web |
|
American Roentgen Ray Society Images of Gastrointestinal stromal tumor pathophysiology |
|
Directions to Hospitals Treating Gastrointestinal stromal tumor |
|
Risk calculators and risk factors for Gastrointestinal stromal tumor pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Parminder Dhingra, M.D. [2]
Overview
On microscopic histopathological analysis, spindle cells or plump epithelioid cells are characteristic findings of gastrointestinal stromal tumor.
Pathophysiology
- GISTs are thought to arise from interstitial cells of Cajal (ICC),[1] that are normally part of the autonomic nervous system of the intestine. They serve a pacemaker function in controlling motility.
- GISTs are believed to arise from the interstitial cells of Cajal, with 95% staining positive for CD117 (c-KIT) and 70% for CD34. The former is a tyrosine kinase growth factor receptor and the target of ST-571 (Imatinib; Glivec).
- Grading GISTs requires assessment of both tumour size and mitotic index. Smaller lesions have less aggressive biological behaviour, as do stomach GISTs when compared to tumours elsewhere along the gastrointestinal tract.
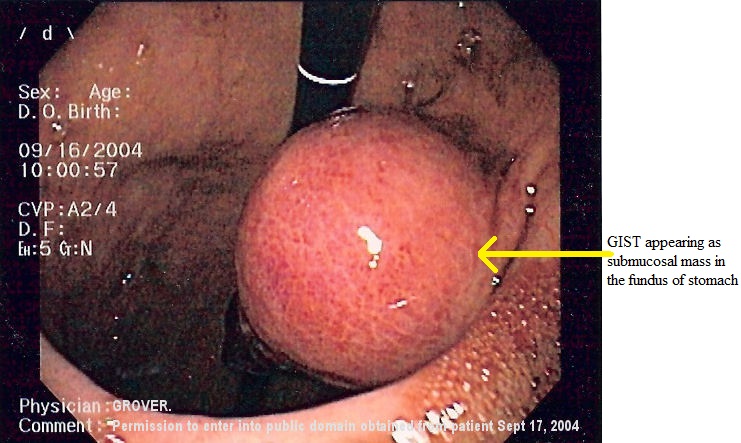
- Macroscopically these tumours are rounded with frequent haemorrhagic change. Larger tumours also may demonstrate necrosis and cystic change. Size is variable ranging form 1 to 30cm.
- Histology demonstrates a relatively cellular tumor comprised of spindle cells (70-80%) and or plump epithelioid cells (20-30%). They appear to arise from the muscularis propria layer.[2]


References
- ↑ Miettinen M, Lasota J (2006). "Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis". Arch Pathol Lab Med. 130 (10): 1466–78. PMID 17090188.
- ↑ "Gastrointestinal stromal tumour".