Galactosemia overview: Difference between revisions
| Line 30: | Line 30: | ||
The order of these three types is not the same as the order that the enzymes are encountered by galactose on its metabolic path (which is closer to GALK, GALT, and then GALE, though many variations can occur.) | The order of these three types is not the same as the order that the enzymes are encountered by galactose on its metabolic path (which is closer to GALK, GALT, and then GALE, though many variations can occur.) | ||
==Pathophysiology== | ==Pathophysiology== | ||
Revision as of 17:34, 26 December 2013
|
Galactosemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Galactosemia overview On the Web |
|
American Roentgen Ray Society Images of Galactosemia overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Dayana Davidis, M.D. [2]
Overview
Galactosemia is a rare genetic metabolic disorder which affects an individual's ability to properly metabolize the sugar galactose. In individuals with galactosemia, the enzymes needed for further metabolism of galactose are severely diminished or missing entirely, leading to toxic levels of galactose to build up in the blood, resulting in hepatomegaly (an enlarged liver), renal failure, cataracts, and brain damage.
Historical Perspective
Von Ruess in a 1908 publication entitled Sugar Excretion In Infancy reported on a breast fed infant with hepatomegaly and spleen enlargement, failure to thrive and galactosuria.
Goppert first described the disease in 1917,[1] with its cause as a defect in galactose metabolism being identified by a group led by Herman Kalckar in 1956.[2]
Classification
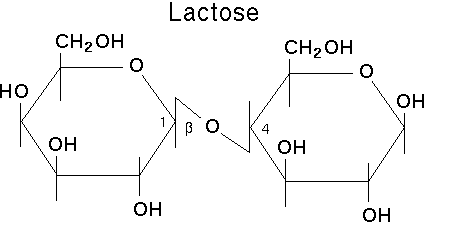
Galactosemia is an inherited rare autosomal recessive trait that leads to the build up of galactose in the blood. The word galactosemia means too much galactose, which is a simple sugar obtained after lactose, the sugar found in dairy products, is broken down by enzymes found in the body into galactose and glucose.
Galactose is converted into glucose by the action of three enzymes, known as the Leloir pathway. Accordingly, there are 3 known types of Galactosemia; type 1, 2 and 3:
| Type | Diseases Database | OMIM | Gene | Locus | Enzyme | Name |
| Type 1 | Template:DiseasesDB2 | 230400 | GALT | 9p13 | galactose-1-phosphate uridyl transferase | classic galactosemia |
| Type 2 | Template:DiseasesDB2 | 230200 | GALK1 | 17q24 | galactokinase | galactokinase deficiency |
| Type 3 | Template:DiseasesDB2 | 230350 | GALE | 1p36-p35 | UDP galactose epimerase | galactose epimerase deficiency, UDP-Galactose-4-epimerase deficiency |
The order of these three types is not the same as the order that the enzymes are encountered by galactose on its metabolic path (which is closer to GALK, GALT, and then GALE, though many variations can occur.)
Pathophysiology
Lactose in food (such as dairy products) is broken down by the body into glucose and galactose.
In individuals with galactosemia, the enzymes needed for further metabolism of galactose are severely diminished or missing entirely, leading to toxic levels of galactose to build up in the blood, resulting in hepatomegaly (an enlarged liver), renal failure, cataracts, and brain damage. Without treatment, mortality in infants with galactosemia is about 75%.
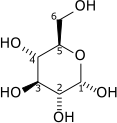
Shown below is a diagram depicting galactose metabolism and the different enzymes involved in it.
Differential Diagnosis
Galactosemia is sometimes confused with lactose intolerance, but galactosemia is a more serious condition. Lactose intolerant individuals have an acquired or inherited shortage of the enzyme lactase, and experience abdominal pains after ingesting dairy products, but no long-term effects. In contrast, a galactosemic individual who consumes galactose can cause permanent damage to their bodies.
Epidemiology and Demographics
Its incidence is about 1 per 47,000 births (classic type). It is much rarer in Japan and much more common in Italy, specifically the traveler region.
Complications
Long term complication of galactosemia includes:
- Speech deficits
- Ataxia
- Dysmetria
- Diminished bone density
- Premature ovarian failure
- Cataract
Diagnosis
Infants are now routinely screened for galactosemia in the United States, and the diagnosis is made while the person is still an infant. Almost all the states require testing the newborn for high galactose and galactose-1-phosphate levels in the blood, if either is high further blood and DNA testing are done to confirm the diagnosis. Newborns who do not accept milk and experience vomiting may not have high levels of galactose or galactose-1-phosphate in their blood, in these cases if galactosemia is suspected, further enzyme tests should be performed.
Treatment
The only treatment for classic galactosemia is eliminating lactose and galactose from the diet. Even with an early diagnosis and a restricted diet, however, some individuals with galactosemia experience long-term complications such as speech difficulties, learning disabilities, neurological impairment (e.g. tremors, etc), and in girls, ovarian failure. These complications are treated if they appear in a manner similar to the way they would be treated in a non-galactosemic. Such complications have not been associated with Duarte galactosemia, and many individuals with Duarte galactosemia do not need to restrict their diet at all. Infants with classic galactosemia cannot be breast-fed due to lactose in human breast milk and are usually fed a soy-based formula.[3]
References
- ↑ Goppert F. Galaktosurie nach Milchzuckergabe bei angeborenem, familiaerem chronischem Leberleiden. Klin Wschr 1917;54:473-477.
- ↑ Isselbacher KJ, Anderson EP, Kurahashi K, Kalckar HM (1956). "Congenital galactosemia, a single enzymatic block in galactose metabolism". Science. 13 (123): 635–6. PMID 13311516.
- ↑ http://www.cdc.gov/breastfeeding/disease/contraindicators.htm