Deep vein thrombosis ultrasound
| Resident Survival Guide |
Editor(s)-In-Chief: The APEX Trial Investigators, C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2] ; Kashish Goel, M.D.; Assistant Editor(s)-In-Chief: Justine Cadet
|
Deep Vein Thrombosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Deep vein thrombosis ultrasound On the Web |
|
Risk calculators and risk factors for Deep vein thrombosis ultrasound |
Overview
Venous ultrasound (US) is the confirmatory test for the diagnosis of deep vein thrombosis (DVT). The US performed for suspected DVT can be either a proximal compression ultrasound (CUS) or a whole-leg US. The most commonly used form is proximal CUS, which assesses the compressibility of femoral and popliteal veins. The diagnosis of DVT is established if the vein can not be collapsed under gentle ultrasound probe pressure. Depending on the results of other tests, a serial CUS might be performed. Whole-leg ultrasound examines the deep veins of the proximal leg and calf; however, it is less commonly used. Iliac vein ultrasound may be performed if thrombosis is suspected in these veins (e.g.: pregnant women with swelling of the whole leg).
Ultrasound
Compression Ultrasonography
Compression ultrasonography in B-mode has high sensitivity and specificity for detecting proximal deep vein thrombosis in symptomatic patients. The sensitivity lies somewhere between 90 to 100% for the diagnosis of symptomatic deep vein thrombosis, and the specificity ranges between 95 to 100%.
- Three months VTE rate with negative ultrasound is 0.57%
- It is one of the diagnostic tests for confirming the disease.
It is currently the first-line imaging examination for DVT because of the following reasons:
- Relative ease of use
- Absence of irradiation or contrast material
- High sensitivity and specificity
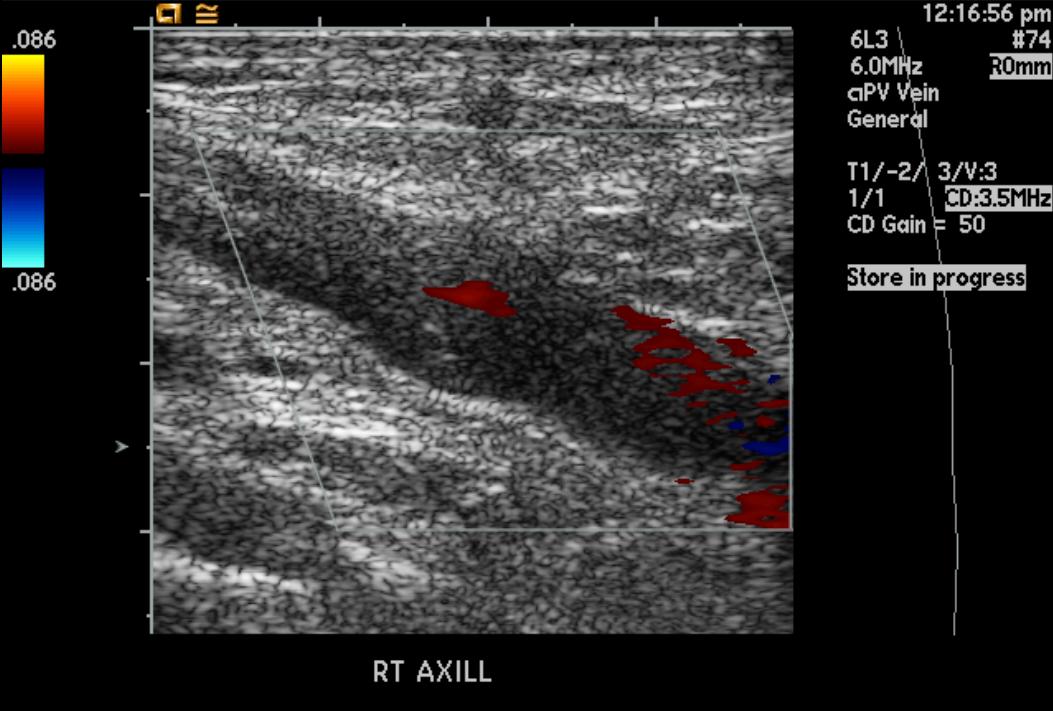
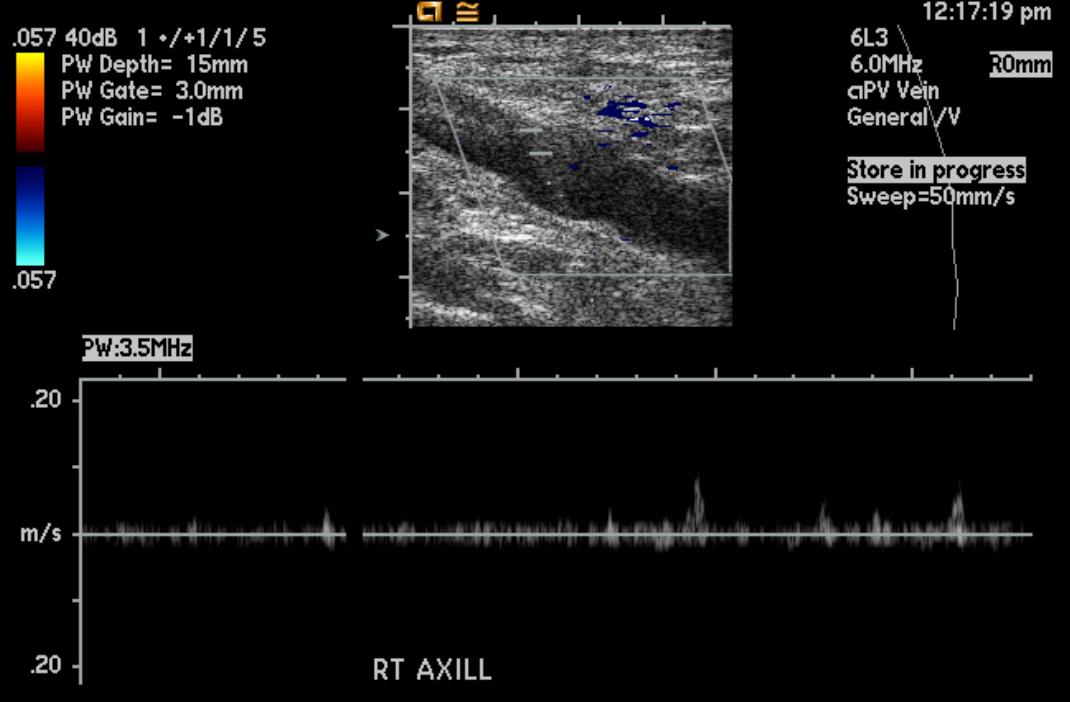
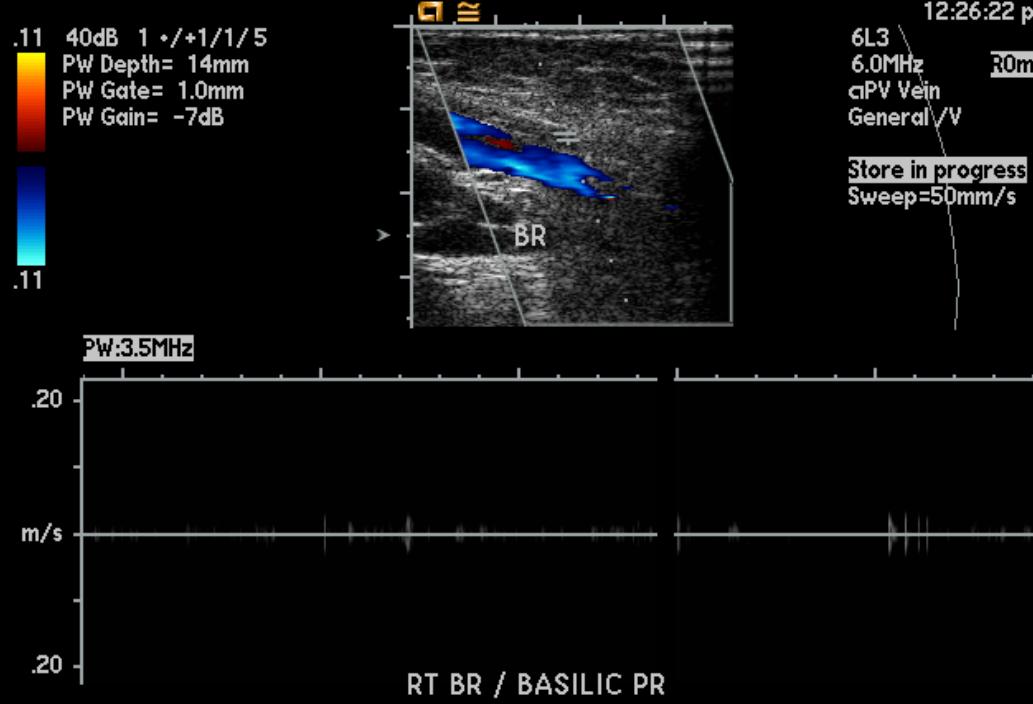
Ultrasound Images Demonstrating Upper Extremity Deep Vein Thrombosis
Whole Leg Ultrasound
Whole-leg ultrasound examines the deep veins of the proximal leg and calf; however, it is less commonly used
Ultrasound in Suspected Recurrent Lower Extremity DVT
Shown below are the definitions of negative, positive, and non-diagnostic ultrasound for recurrent DVT.
- Negative ultrasound:
- Normal US, or
- Increase in residual diameter of less than 2 mm, or
- Area of prior non-compressibility with a decreased or stable residual diameter
- Non-diagnostic US:
- Ultrasound that is technically limited, or
- Area of prior non-compressibility with an increment in residual venous diameter of < 4 mm yet ≥ 2 mm, or
- Area of prior non-compressibility in the absence of a previous measurement of the residual diameter
- Positive US:
- New non-compressible segment, or
- Area of prior non-compressibility with an increment in residual venous diameter of ≥ 4 mm[1]
Limitations
It has several limitations.
- As with impedance plethysmography, the results are limited in patients with deformities or a plaster cast.
- Isolated thrombi, present in the following locations, are not identified:
- In the iliac vein
- Femoral vein within the adductor canal.
- Serial studies may be needed, if the initial test is negative.
References
- ↑ Bates SM, Jaeschke R, Stevens SM, Goodacre S, Wells PS, Stevenson MD; et al. (2012). "Diagnosis of DVT: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e351S–418S. doi:10.1378/chest.11-2299. PMC 3278048. PMID 22315267.